
Macalester College. W. Grompel, MD: "Order Tadapox online no RX - Best online Tadapox OTC".
This can be clarifed by using contrast agents and by follow-up examinations within hours order tadapox toronto how is erectile dysfunction causes. If blood is demonstrated with B-scan ultrasound 80mg tadapox amex erectile dysfunction from steroids, colour Doppler may allow the source of a still-active bleeding to be found buy generic tadapox 80mg on-line erectile dysfunction. It is advisable to cover the transducer with a glove, to use disinfectants and to protect health-care personnel, especially if invasive procedures (guided puncture) are carried out. In many situations, the ultrasound fndings will be aspecifc and the particular disease will not be evident. It is ofen difcult to diferentiate between infectious and neoplastic diseases; for example, if atypical enlarged lymph nodes (Fig. Systematic review: evidence-based management of hepatocellular carcinoma–an updated analysis of randomized controlled trials. Current expert opinion and recommendations derived from the 10th World Congress on Gastrointestinal Cancer, Barcelona, 2008. Puncture aspiration injection re-aspiration: an option for the treatment of cystic echinococcosis. Axial resolution: Absorption coefficient: the ability to distinguish objects in the direction of Product of absorption constant (of a medium) the ultrasound beam emitted by a transducer. B-scan: Acoustic enhancement: Mode of display in which echoes are presented as Relative intensification of the echoes distal light spots on the screen. Acoustic shadow: Echo-free or relatively echo-poor (partial Colour Doppler technique: shadow) area on an ultrasonic image occurring Duplex technique in which the Doppler signals are distal to interfaces, resulting in total reflection displayed as coloured pixels, depending on their of the ultrasound (gas, foreign bodies) or mean velocity. Contrast agent: Encapsulated microbubbles used intravenously to Acoustic streaming: enhance the Doppler signal from streaming blood. Movement of fluid due to ultrasound (demonstrated as movement of the echoes Contrast harmonic imaging: arising within a non-homogeneous fluid). Based on a technique to receive only echoes with a doubled frequency (second harmonic) rather Anechoic, anechogenic: than the fundamental (emitted) frequency. Denotes the absence of (internal) echoes, Enables better differentiation of the signals due to typically for fluid (synonym: Echo free). Feature on an ultrasonic image that is not Coronal plane: referable to real structures with regard to shape, Plane corresponding to the long axis of the body intensity or location. Crystal:Cry Echo poor: Polar crystals used as ultrasound transducersansdu Echo pattern consisting of a few weak echoes. Curved array: Transducer with two or usually more crystals Far field: arranged on a convex surface. Focus: Natural focus, the narrowest point of the Depth gain compensation: ultrasound field between the near and the far Synonym for time gain compensation. Adjustment of the ultrasound beam to a Doppler effect: particular distance (depth), to obtain the best Change in the original (emitted) frequency resolution of the region of interest. Doppler frequency: Gain: Difference between original (emitted) and Relation between energy output and input in an received frequency. Duplex technique: Hertz: Fixed combination of a Doppler system with the Unit of frequency, equal to one cycle per second. Part of the ultrasound field between the transducerP eu ndfi d and the focus (synonym: Fresnel zone). Technically, a part interposed between two structural components to compensate for their Piezoelectric effect: imperfect fit. Property of polar crystals to convert mechanical energy (pressure and tension) into electrical Lateral resolution: energy (ultrasound receiver) and vice versa (Poorer) resolution in a direction transversal to (reverse piezoelectric effect: ultrasound the ultrasound beam. Linear array: Pulse-echo technique: Linear arrangement of two or more crystals, Ultrasound technique in which the ultrasound which are activated electronically in groups. B-scan technique with rapid construction of Mechanical index: images (about 15 per s), creating the impression Amount of negative acoustic pressure in the of a continuous image. Reverberation: Mirror effect: Reflection of ultrasound between two nearly Total reflection of ultrasound pulses by some parallel surfaces backward and forward structures, e. The repeated echoes arrive at the transducer with a delay and are positioned in the M-mode: image at a doubled or multiple distance. Section of the body or organ passed by thepasse e uultrasound beams of the actual scan. Sector scan: Two-dimensional B-scan produced by diverging Transducer: ultrasound beams (typical of mechanical real Device that converts one form of energy into time and curved array transducers). Sonolucent: Tissues and structures with a low (below Transverse scan: average) attenuation of ultrasound. Spectral Doppler: Display of all frequencies of the Doppler signal Ultrasound: over time. Specular reflector: Reflector (tissue surface or vessel wall) with a Wavelength: smooth surface and a diameter greater than the Length of a single cycle of a (ultrasound) wave, diameter of the wavelength. Stimulated acoustic emission: Short but strong signal created by destruction of microbubbles by ultrasound (high mechanical index) used e. Thermal index: Measure of heating of tissue by absorption; ratio of power used to that required to cause a maximum temperature increase of 1 °C. With increasing use of ultrasonography in medical settings, the need for education and training became essential. Soon, however, rapid developments and improvements in equipment and indications for the extension of medical ultrasonography into therapy indicated the need for a totally new ultrasonography manual. The contributors (more than 50 for the two volumes) belong to five different continents, to guarantee that manual content represents all clinical, cultural and epidemiological contexts. This new publication, which covers modern diagnostic and therapeutic ultrasonography extensively, will certainly benefit and inspire medical professionals in improving ‘health for all’ in both developed and emerging countries. Anaphylactic shock Hypovolemic shock is present when marked reduction in oxygen delivery results from diminished cardiac output secondary to inadequate vascular volume. In general, it results from loss of fluid from circulation, either directly or indirectly. Septic Shock (vasogenic shock) develops as a result of the systemic effect of infection. It is the result of a septicemia with endotoxin and exotoxin release by gram-negative and gram-positive bacteria. Despite normal or increased cardiac output and oxygen delivery, cellular oxygen consumption is less than normal due to impaired extraction as a result of impaired metabolism. Neurogenic shock results primarily from the disruption of the sympathetic nervous system which may be due to pain or loss of sympathetic tone, as in spinal cord injuries. This circulatory response to hypotension is to conserve perfusion to the vital organs (heart and brain) at the expense of other tissues. Progressive vasoconstriction of skin, splanchnic and renal vessels leads to renal cortical necrosis and acute renal failure. If not corrected in time, shock leads to organ failure and sets up a vicious circle with hypoxia and acidosis. But in general patients with hypotension and reduced tissue perfusion presents with: Tachycardia Feeble pulse Narrow pulse pressure Cold extremities (except septic shock) Sweating, anxiety Breathlessness / Hyperventilation Confusion leading to unconscious state 2 Summary: Clinical features of hypovolemic shock in adults with estimated volume loss. Estimated blood loss 750-1500ml 1500ml-2000ml >2000 ml Blood pressure Normal Reduced Severely Reduced Pulse rate >100/min >120/m >140/m very feeble Capillary refill Slow Slow Undetectable Respiratory rate 20-30/m 30-40/m >35/m Urinary flow rate 20-30/hr 10-20/hr 0-10/hr (Normal: 30-60 ml/hr or 0. General Management • Monitor the airway, breathing and circulation as first priority • Stop bleeding • Fluid resuscitation, preferably crystalloids • Head down position • Treat the cause • Transfusion of compatible blood if indicated • Oxygen and other supportive measures like inotropic agents • Monitoring of resuscitation effectiveness: e.
Ankle Fractures Classifcation (Weber) Type A • Avulsion of the fbula to the joint line • Syndesmotic ligament intact • Medial malleolus undamaged or fractured in a shear –type pattern with the fracture line angulating in a proximal medial direction from the corner of the morti: • Oblique orOblique or spiral frala beginningfbula beginning at the level of the joint up to the shaf of the fbula buy generic tadapox on-line statistics of erectile dysfunction in us. Surgery Clinical Treatment Guidelines 25 Chapiter 1: Orthopaedic Surgery • Medial malleolus intact or sustain a transverse avulsion fracture tadapox 80 mg low price jack3d causes erectile dysfunction. If the medial malleolus is lef intact there can be a tear of the deltoid ligament cheap tadapox uk erectile dysfunction diabetes medication. Management Principles of initial treatment of ankle fractures • Immediate closed reduction and splinting, with the joint held in the most normal position possible to prevent neurovascular compromise of the foot. If this fragment represents less than 25% of the articular surface of the tibial plafond and there is less that 2 mm of displacement, internal fxation is not always required. In the rare instance of symptomatic non-union, careful excision is indicated • Intra-articular fractures → Treatment of displaced intraarticular fractures remains controversial → Some surgeons still advise conservative treatment → Other surgeons advocate early closed manipulation of displaced intra-articular fractures, to at least partially restore the external anatomic confguration of the heel region. Internal fxation with percutaneous pins (Essex-Lopresti technique) may be performed. Fractures and dislocations may disrupt this vascularization, causing delayed healing or avascular necrosis. Management Type 1 • Non-weight–bearing below-knee cast for 2–3 months until clinical and radiologic signs of healing are present Type 2 • Closed reduction. If open reduction, with or without bone grafing, is elected, prolonged protection from weight bearing is the best means of preventing collapse of the healing area. Fractures of the Phalanges of the Toes Management A weight-bearing removable immobilization Spiral or oblique fracture of the proximal or middle phalanges of the lesser toes can be treated adequately by binding the involved toe to the adjacent uninjured toe (buddy taping) Comminuted fractures of the distal phalanx are treated as sof tissue injuries 1. Fracture of the Sesamoids of the Great Toe Management Undisplaced fractures: Hard-soled shoe or metatarsal bar Displaced fractures: Immobilization in a walking boot or cast, with the toe strapped in fexion If conservative modalities have been exhausted: The last resort treatment is excision Treatment of fractures in children: The treatment of the majority of fractures in children and adolescents will be conservative. Indications for surgical treatment of fractures in children include: • Open fractures • Polytrauma • Patients with head injuries • Femoral fractures in adolescents • Femoral neck fractures • Certain types of forearm fractures • Certain types of physeal injuries • Fractures associated with burns 32 Surgery Clinical Treatment Guidelines Chapiter 1: Orthopaedic Surgery 1 1. Epiphyseal Fracture The cartilage physeal plates are a region of low strength relative to the surrounding bone and are susceptible to fracture in children. Tus, open reduction is more likely in fractures involving physes and joints than in other pediatric fractures. Forearm Fracture In children, most forearm fractures that involve both bones can be treated successfully by closed reduction and casting. Minor angular mal-alignment can easily be tolerated if rotational alignment of the bone end is accurate. Rarely severely angulated or rotationally mal-aligned metacarpals and phalanges can be managed by immobilization for 2–3 weeks. Gross displacement is fairly uncommon and can usually be treated symptomatically because the intact periosteum stabilizes the large fat bones. Femoral neck fractures in children are generally treated by reduction and fxation. In rare and unstable cases, some open fractures, or fractures in older children may also require operative treatment. Open Fractures Defnition: An Open Fracture is when disruption of the skin and underlying sof tissue results in communication between the fracture and the outside environment. Causes Motor vehicle accidents Farm accidents Sports accidents A force large enough to cause a fracture Signs and symptoms Associated with neuro-vascular injury 36 Surgery Clinical Treatment Guidelines Chapiter 1: Orthopaedic Surgery 1 Diagnosis Clinical examination of the specifc fracture should include the site of the fracture and severity of the fracture. The primary injury is the result of the 38 Surgery Clinical Treatment Guidelines Chapiter 1: Orthopaedic Surgery 1 initial, mechanical forces, resulting in shearing and compression of neuronal, glial, and vascular tissue. The secondary injury is described as the consequence of further physiological insults, such as ischaemia, re-perfusion and hypoxia, to areas ‘at risk’ in the brain in the period afer the initial injury. Critical care of multiple injuries Defnition: Multi-trauma are physical insults or injuries occurring simultaneously on several parts of the body. General Consideration Defnition: Complete separation and loss of 2 articulating bone contact surfaces. Acromio-Clavicular Joint Dislocation Defnition: Classifed in 6 diferent types depending on which ligaments are sprained or torn. Recommendations Physical therapy under supervision post immobilization removal Pre and post reduction: X-Ray and Neuro-Vascular status evaluation is mandatory 1. Hip Dislocation Description Traumatic hip dislocation of the hip joint may occur with or without fracture of the acetabulum of the proximal end of the femur. Traumatic Knee Dislocation Defnition: Is the complete displacement of the tibia with respect to the femur and with disruption of 3 or more of the stabilizing ligaments. Surgery Clinical Treatment Guidelines 51 Chapiter 1: Orthopaedic Surgery Management A knee dislocation is a potentially limb threatening condition, therefore immediate reduction is recommended even before a radiography evaluation. Conservative • Immediate closed reduction and immobilization at 20-30o of fexion for 6 weeks • Range of motion/exercise should be instituted afer adequate sof tissue healing 6-12 weeks Surgical • Indications → Unsuccessful closed reduction → Open injuries → Vascular injuries → Residual sof tissue interposition Recommendations Acute repair of lateral ligament followed by early functional bracing is advised (meniscal injuries to be addressed at time of surgery Medial collateral injuries generally heal without surgery The role of cruciate reconstruction in the acute setting remains controversial 1. Patellar Dislocation Description: Patella dislocation is more common particularly in females due to physiologic laxity and in patients with hyper mobility (athletes) Causes Physiological laxity Direct trauma to the patella Connective tissue disease (Marfan Syndrome) Congenital abnormality of the patella and trochlea Hypoplasia of the Vastus Medialis muscle Hypertrophy of the lateral retinacular 52 Surgery Clinical Treatment Guidelines Chapiter 1: Orthopaedic Surgery 1 Signs and symptoms Pain focused around the knee joint Inability to fex knee Hemarthrosis Swelling with tenderness of the knee Palpated displaced patella Investigation X-ray of the knee (Anteroposterior and Axial views) Complications Recurrent dislocation Re-dislocation Patella-femoral Arthritis Management Conservative • Closed reduction with cylinder casting for 2 3 weeks • Isometric quadriceps exercises afer removal of the cast Surgery • Recurrent episodes require operative repair Surgery Clinical Treatment Guidelines 53 Chapiter 1: Orthopaedic Surgery 1. Septic Arthritis Defnition: Septic arthritis is the infammation of a synovial membrane with purulent efusion into the joint space usually caused by bacteria. Chronic Osteomyelitis Defnition: Exogenous or hematogenous infection that has gone untreated or has failed to respond to treatment. Fracture of Wrist Bones Description Carpal/wrist bones are in 2 rows: • A wrist fracture is a break in one or more of the bones in the wrist. Causes Fall on the outstretched hand and extended wrist Motor vehicle accident Sports contact injury 1. Fracture of the Scaphoid Bone Description: Scaphoid fractures are by far the most common of the carpal fractures, estimated at 70-79%. Classifcation Herbert classifcation of scaphoid fractures Type A fractures are stable and acute including: • A1: Fracture of the tubercle • A2: Incomplete fractures of the scaphoid waist Type B fractures are unstable and include: • B1: Distal oblique fractures • B2: Complete fracture of the waist • B3: Proximal pole fractures • B4: Transscaphoid perilunate fracture dislocation of the carpus Type C fractures are characterized by delayed union. Other Wrist Bone Fractures Description: Commonly associated with above carpal bone fractures. Metacarpal Fractures Description: Metacarpal bones are located between carpal bones and phalanges. From radial to ulna we have thumb (First) Metacarpal and second to ffh metacarpal. Bennett’s and Rolando’s Fractures Description Bennett’s fracture is an intra articular fracture of the base of the thumb metacarpal characterized by one small ulna fragment. Causes Fall with axial loading through the thumb metacarpal Direct blow of the thumb metacarpal Injury involving forced abduction of the thumb Signs and symptoms Pain and swelling Decreased range of motion of the thumb Shortening of the thumb Dorsal and radial displacement of the metacarpal bone Surgery Clinical Treatment Guidelines 65 Chapiter 1: Orthopaedic Surgery Investigations Plain x-ray (Antero-posterial and oblique views) Management Surgical • If the Bennett’s fragment is less than 15-20% of the articular surface: Closed reduction and percutaneous pin fxation followed by a thumb spica splint for 4-6 weeks. Fractures of Phalanges Proximal and middle phalanges Defnition/Description: Fracture of the bones of the proximal or middle phalanges of the fngers. Distal Phalanges and Nail Bed Injuries Description: Distal phalanges fractures are ofen associated with nail bed laceration. Dislocations of the Hand Joints Defnition: A dislocation is a misalignment of the bones forming a joint. If relocation is difcult under those circumstances do an open reduction • Splinting in functional position for 4 weeks and then physiotherapy Surgical • Sometime the volar plate or tendons can be entrapped into the joint and that is why it may be impossible to do a closed reduction. Recommendation Refer to orthopedic surgeon or hand surgeon any dislocation that can’t be relocated conservatively. Burns Wound management of the burned hand follows the general principles of burn wound management.
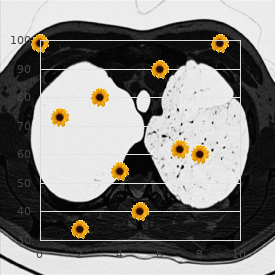
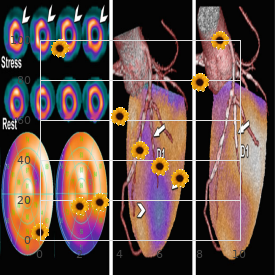
Multiple nodules may also be found in patients with splenic infections buy generic tadapox top 10 causes erectile dysfunction, particularly in those who are immunocompromised (Fig buy tadapox 80 mg with visa erectile dysfunction prevalence age. The so-called ‘wheels-within wheels’ appearance of target lesions suggests micro-abscesses caused by fungus or miliary tuberculosis purchase cheap tadapox impotence yoga postures. Intrasplenic masses Splenic masses may be single or multiple and well defned or irregular in outline. Malignant tumours The commonest malignant neoplasms involving the spleen are lymphomas, which may produce either focal hypoechoic masses or difuse enlargement of the spleen (Fig. Splenomegaly is a frequent fnding in lymphoma, but a normal-sized spleen does not exclude the diagnosis. Longitudinal scan: lymphoma of the spleen Malignant tumours of the spleen, either primary or metastatic, are very rare. Metastatic deposits from primary tumours of the lungs, breast, ovary and stomach can produce multiple foci of varying echotexture. Multifocal or difuse lesions, mixed or hyperechoic patterns and target lesions (usually larger than 1 cm) tend to indicate malignancy (Fig. Splenic infarction Splenic infarcts are typically seen in patients prone to embolic phenomena. Splenic infarcts may initially be large and then become small and echogenic as fbrosis occurs. Haemangiomas Haemangiomas are most ofen well defned focal, echogenic lesions (Fig. Although splenic haemangiomas may have an echogenic appearance similar to that of the liver, the sonographic appearance is variable. Lymphangiomas may also occur in the spleen and appear as a multiloculated cystic mass with internal septations (Fig. Metastatic tumours of the spleen may manifest as multiple hypoechoic nodules scattered through the splenic parenchyma Fig. Transverse scan shows a well defned hyperechoic mass with internal hypoechoic area in the spleen 216 Fig. Lymphangioma in the spleen Enlarged splenic vein A normal splenic vein does not exclude portal hypertension; however, the presence of portosystemic collateral vessels, ascites and cirrhosis of the liver indicates portal hypertension. If the splenic vein appears large and remains larger than 10 mm in diameter on normal respiration, portal hypertension should be suspected. A portal vein that is larger than 13 mm in diameter and does not vary with respiration is strongly correlated with portal hypertension (Fig. Two patients with dilatation of the splenic vein and multiple varicosities, the results of portal hypertension 217 Trauma Ultrasound can be very useful and highly accurate in the diagnosis of subcapsular and pericapsular haematomas of the spleen. The advantages of ultrasound in assessing splenic trauma include speed, portability with no delay of therapeutic measures and absence of ionizing radiation. The examination should include a survey of the outline of the spleen to identify any area of local enlargement, followed by a survey of the abdomen to determine whether free intraperitoneal fuid is present. Repeat the scan afer a few days if the clinical condition of the patient does not improve. If there is free intraperitoneal or subphrenic fuid and an irregular splenic outline, a splenic tear or injury is likely. If the fuid collection is half-moon-shaped and follows the contour of the spleen, it suggests subcapsular haematoma (Fig. Subcapsular and intraparenchymal haematomas are seen Immediately afer a traumatic accident, the haematoma is liquid and can easily be diferentiated from splenic parenchyma; however, within hours or days, the echogenicity of the perisplenic clot may closely resemble that of normal splenic parenchyma. Old, temporally remote splenic injuries ofen present sonographically as almost purely cystic collections or calcifed masses consisting of irregular clumps of calcifcation or curvilinear, dense echogenicity. Haematoma If the capsule of the injured spleen remains intact, an intraparenchymal or subcapsular haematoma may result (Fig. The echogenicity of a haematoma depends on the stage at which the scan is performed. An enlarged spleen due to portal hypertension, in which a solitary haemangioma was an incidental fnding. Intraparenchymal haematoma of the spleen and perisplenic fuid collection 219 Chapter 11 Gastrointestinal tract Preliminary note 223 Oesophagus 224 224 Indications 224 Examination technique 225 Normal findings 225 Pathological findings Stomach, including distal oesophagus 225 and proximal duodenum 225 Indications 226 Examination technique 226 Normal findings 228 Pathological findings 238 Differential diagnosis Small and large bowel 238 238 Indications 239 Examination technique 239 Normal findings 242 Pathological findings 256 Differential diagnosis 11 Gastrointestinal tract Preliminary note Both the cervical and distal abdominal part of the oesophagus can be visualized by transcutaneous ultrasound. As the thoracic part is hidden behind the gas-containing lung and the spine, the wall of this major part of the oesophagus can be visualized only by endoscopic ultrasound. Generally, the stomach and the small and large bowel are accessible to transcutaneous ultrasound, whereas the rectum, especially the distal part, can be examined by endoscopic ultrasound much better than externally through the fuid-flled bladder. Use of the transcutaneous technique permits diferentiation of the layers of the wall. In this way, a thickening not only of the whole wall but also of a single layer or the destruction of layers by an infltrating process can be visualized. With a transducer of lower frequency or of lower quality, especially a sector scanner, only marked alterations, e. Five layers of the wall of the gastrointestinal tract can be diferentiated by high frequency transcutaneous ultrasound and by endoscopic ultrasound (Fig. The echo-rich lines 1 and 5 are due to interface echoes that arise at the border between the (fuid-flled) lumen and the wall (layer 1) and the wall and the surrounding tissue (layer 5), respectively. The echo-poor layer 2 corresponds to the mucosa; the echo-rich layer 3 corresponds to the submucosa, which includes the echoes from the muscularis mucosae. In thedeeper parts of thecolon and in therectum, a thinecho-rich line can be visualized, which marks the border between the inner circular muscle layer and the outer longitudinal muscles. Distinguishing the anatomical layers of the wall of the gastrointestinal tract depends on the frequency and the quality of the transducer on the one hand and, on the other, on the thickness of the layers. The layers of the gastric wall or the rectum can be readily visualized, but not thoseof thewallof thesmallbowel, because thethickness of the diferent layers of the bowel wall lies in the range of the axial resolution of the ultrasound transducers used. Echo-rich layers ofen appear too thick, as the strong interface echoes between the border of echo-poor (mucosa and muscularis propria) and echo-rich layers (submucosa) add to the echo-rich layer in the ultrasound image. The borderline echoes of the posterior wall are neither very striking (layer 1) nor discernible from the surrounding tissue (layer 5) Oesophagus Indications Tere are no clear indications for ultrasonography of the oesophagus for pathological conditions, because the major part is not accessible to transcutaneous ultrasound. In some situations, difculties in swallowing may be an indication to examine the cervical and abdominal parts of the oesophagus (and the stomach), if an endoscopic examination is not immediately possible. Normal findings The cervical part of theoesophagus can be seen as a tubular structure behind thethyroid gland (see Fig. Pathological findings A tumour of thecervical part of theoesophagus can be seen as anecho-poor mass with an irregular outline behind the thyroid (Fig. Infltration of the thyroid or into the surrounding tissue can be seen directly or may be assumed if no movement is seen during swallowing. Oesophageal carcinoma: echo-poor thickened wall and stenotic lumen (bright echoes) of the lower cervical part of the oesophagus behind the thyroid. Shadow behind air echoes cranial to the tumour Stomach, including distal oesophagus and proximal duodenum Indications The indications for ultrasonography of the stomach are: pain in the upper abdomen dysphagia and vomiting palpable mass in the upper abdomen suspected dysfunction (e. A more selective examination of the stomach is useful if endoscopy is not available. In certain diferential diagnoses arising during gastroscopy, transabdominal ultrasonography of the stomach is as useful as endoscopic ultrasound. Preparation The stomach should be empty (fasting period, 4–6 h), as the gastric contents mask pathological conditions.
Blood or meconium on the baby‟s skin should be wiped away; however cheap 80 mg tadapox mastercard erectile dysfunction after vasectomy, the white greasy substance covering the baby‟s body (vernix) should not be wiped off tadapox 80mg otc erectile dysfunction causes mental. Because this vernix helps to protect the baby‟s skin and gets reabsorbed very quickly tadapox 80mg for sale erectile dysfunction treatment ginseng. A normal newborn should be crying vigorously or breathing regularly at a rate of 40-60 breaths per minute. If the baby is not breathing well, then the steps of resuscitation have to be carried out as explained in the lesson on „Resuscitation‟. Leave the baby between the mother’s breasts to start skin-to-skin care Once the cord is cut, the baby should be placed between the mother‟s breasts to initiate skin-to-skin care. This will help in maintaining the normal temperature of the baby as well as in promoting early breastfeeding. Place an identity label on the baby This helps in easy identification of the baby, avoiding any confusion. Both the mother and the baby should be covered with a warm cloth, especially if the delivery room is cold (temperature less than 250C). Since head is the major contributor to the surface area of the body, a newborn baby‟s head should be covered with a cap to prevent loss of heat. Encourage the initiation of breastfeeding Breastfeeding should be initiated with in one hour of birth in all babies. Emphasize on cord and eye care with a doll, fresh (or preserved) umbilical cord, sterile tie and blades, pieces of cloth, etc. Keeping the baby between the mother‟s breasts also ensures that the baby‟s temperature is kept at the correct level for as long as the skin contact continues. This first skin-to-skin contact should last uninterrupted for at least one hour after birth or until after the first breastfeed. The mother and baby should be covered with a warm and dry cover, especially if the room temperature is lower than 250C. The steps of prevention of heat loss are explained in the lesson on ‘Thermal protection’. For maintaining the temperature, it is important to understand the concept of „Warm chain‟. It means that the temperature maintenance should be a continuous process starting from the time of delivery and continued till the baby is discharged from the hospital. If the baby is crying vigorously or breathing adequately (chest is rising smoothly at a rate of 40 to 60 times per minute), then no intervention is needed. However, if the baby is not breathing or gasping, then skilled care in the form of positive pressure ventilation might be required. This rest period may vary from a few minutes to 30 or 40 minutes before the baby shows signs of wanting to breastfeed. After this period, (remember: each baby is different and this period might vary) the baby will usually open his/her mouth and start to move the head from side to side; may also begin to dribble. The baby should be put next to the mother‟s breast with his mouth opposite the nipple and areola. When they are born, they have to be protected from the adverse environment of the surroundings. Cleanliness at delivery reduces the risk of infection for the mother and baby, especially neonatal sepsis and tetanus. Cleanliness requires mothers, families, and health professionals to avoid harmful traditional practices, and prepare necessary materials. Hand washing is the single most important step to be emphasized to both family members and health care workers. Similar to warm chain, „Clean chain‟ has to be followed both at the time of delivery and then till the time of discharge to protect the infant from infections. Enumerate the „Six cleans‟ one has to follow at the time of delivery: i) ii) iii) iv) v) vi) 32 Lesson 2/ Care of the baby at birth 8. The steps of clamping, cutting the cord and its care after cutting are summarized in the box below: Immediate care of the umbilical cord Steps: 1. Put the baby on mother’s abdomen or on a warm, clean and dry surface close to the mother. Put ties (using a sterile tie) tightly around cord at 2 cm and 5 cm from the abdomen. Note: Applying traditional remedies to the cord may cause infections and tetanus. The baby‟s eyes should be wiped as soon as possible after birth both eyes should be wiped gently with separate sterile swabs soaked in warm sterile water. In areas with a high incidence of sexually transmitted diseases such as gonorrhoea, eye drops or ointment should also be instilled (as per local guidelines) within one hour of delivery of the placenta. This can be done after the baby has been dried or when he is being held by his mother. After instilling the eye drops, care should be taken so that the drug is not washed away. A baby’s eyes should be wiped as soon as possible after birth; In areas where sexually transmitted diseases are common, an anti-microbial eye medicine should be applied within one hour of birth. Both of them should remain in the delivery room for the first hour to facilitate monitoring. During the first hour after birth babies need to be monitored every -------------minutes 2. Name the two most important parameters that need to be monitored in the first hour after birth: i. Feel free to consult your text material, if you need assistance in recapitulating. Normally the newborn is free from harmful organisms for initial few hours after birth. Staff working in health facilities tend to transmit organisms during routine procedures, thus leading to colonization of organisms on surrounding skin of the abdomen, the perineum, groins and respiratory tract. Prevention of infection is more cost effective than treating infection in neonates. Personnel with active infection should not be allowed entry into the baby care area. Basic requirements for asepsis in baby care area include: 2. Single Most Important, Very Simple and Cheap method for prevention of infection in baby care area is 3. To keep the environment clean, in each unit of ward, the waste should be disposed off in a proper way.