
Elms College. Y. Cobryn, MD: "Buy online Suhagra cheap no RX - Trusted online Suhagra OTC".
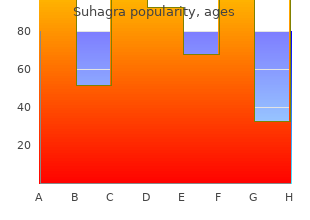
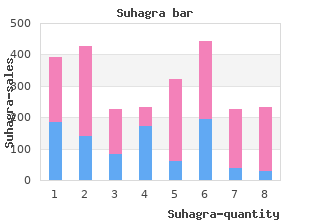
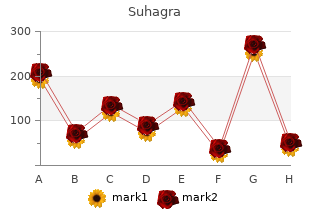
As well buy 100mg suhagra erectile dysfunction doctor in kolkata, differences in physiologic requirements of various athletic activities and their associated risks are discussed purchase generic suhagra online erectile dysfunction rings for pump. Finally discount suhagra 100 mg mastercard injections for erectile dysfunction cost, what is known about the ability to participate in and the risks of athletic activities for the individual groups of congenital cardiac defects is discussed with emphasis on what is known about preathletic screening and recommendations for activities of daily living, leisure and recreational athletics, and participation in competitive sports. These in turn may be influenced by a number of factors such as age, sex, height, weight, and especially cardiovascular conditioning. The ability to successfully and safely undertake a given athletic activity depends on the combination of these factors and the requirements of the activity. All athletic activities can be roughly broken down into their “static” and “dynamic” components (8). This is what is traditionally considered isometric activity or the muscles working against resistance. Examples of activities requiring high static forces are weight lifting and wrestling. The cardiovascular effects of isometric activity depend on the intensity of the activity (e. The dynamic component of exercise can be thought of as the activity that results in muscle contraction and body movement. The cardiovascular effects of high dynamic activity are quite different from static activity. To meet this2 oxygen demand, cardiac output may rise fivefold or more in well-conditioned athletes. Thus, dynamic exercise results primarily in a volume load being placed on the heart as opposed to the pressure load that results from highly static activity. In truth, there are no pure “static” or “dynamic” activities, and all athletic activities are to some degree, a combination of both types. There are sports such as rowing and cycling that require both high static and high dynamic components. This classification is based on peak static and dynamic components achieved during competition. The lowest total cardiovascular demands (cardiac output and blood pressure) are shown in green and the highest in red. Blue, yellow, and orange depict low moderate, moderate, and high moderate total cardiovascular demands, respectively. It is important to remember that the values for this table refer only to competitive sports in adolescents and adults. The contents of this table have little or no relevance to competitive sports participation in the preadolescent population. Much of preadolescent competitive sport training focuses on learning basic skills and coordination. Strength and endurance training have very little or no place in competitive sports at this age. Any parent will tell you that soccer played by a group of 7-year-olds bears almost no relationship to soccer being played by a group of 17-year-olds. Types of Physical Activity Physical activities can be divided into three broad types of activities: (a) activities of daily living, (b) leisure and recreational sports, and (c) competitive sports. Activities of Daily Living “Activities of daily living” is an inclusive term that encompasses all the physical activities required by an individual as part of his or her routine daily tasks. These requirements will vary greatly depending on the age of the individual as well as many other unique circumstances. These studies used various types of motion detectors as well as recall questionnaires. It is also worth noting that most children tend to overestimate the amount of physical activity they perform (17,18). There is at least some evidence that this is due to activity restrictions that have been imposed by physicians, parents, and in some cases by the children themselves (19). Obesity in this population mirrors that of the general pediatric population and occurs even in populations with otherwise excellent cardiac repair and normal or near normal exercise capacities (3,4,19). There is at least some evidence that the amount of obesity is related to daily amounts of physical activity (21). The intensity of physical activity can obviously vary greatly from individual to individual depending on the nature of their employment. Although this may seem obvious, the little research available would suggest that patients and physicians largely ignore this aspect of care. Of concern is the finding that the most common reason patients do not seek information about appropriate level of physical activities is a mistaken belief that all activities are safe to perform (22). Although there may be no formal coaching, some of these activities have significant organization and structure. Intramural sports at the high school or college level may often fall into this category. Less structured activities such as playground “pick-up” games as well as physical activities that may be undertaken by an individual such as cycling or jogging would also fall under this category of leisure or recreational sports. Clearly, the intensity with which these leisure activities are performed may vary widely with the age and circumstances in which they are undertaken (13). This also highlights the importance of understanding the difference and intensity of sports at a recreational level as opposed to a competitive level. For example, intramural flag football has little in common with competitive high school football. Competitive Sports Competitive sports are those that are generally organized, coached, and played at high skill levels. The intensity with which an individual participates in competitive sports is influenced by their personal motivation as well as the outside influences of the coach, other team members, parents and other family members, as well as spectators. The end result is the potential for the individuals to push themselves to participate beyond the level they might otherwise choose to or which might be considered safe by their physician (12). The training for competitive sports may in many cases be of higher intensity than participation in the actual sport. For example, weight training and physical conditioning undertaken by high school athletes playing baseball may easily exceed the intensity of the activity they achieve in the actual game. It is also important to remember, as stated earlier, that “competitive” does not necessarily mean the same thing for all ages. None of the factors that influence high levels of performance in adolescents and adults, such as coaching and spectators, are likely to have much of an effect on young children. Especially at early ages, children are very unlikely to perform beyond a level that they would otherwise choose to self-limit. As such, these “competitive” sports should be thought of more as activities to teach basic physical skills rather than true competitive athletics (12,23). Regardless of age, in the vast majority of the population, the recommended level of 60 minutes of moderate to vigorous physical activities per day is probably appropriate. As will be discussed later in this chapter, this is a level of physical activity that is often achieved in recreational activity or in many cases through competitive sports and is both safe and desirable for many individuals with simple congenital heart defects.
A palliative approach to complete trans- of babies will need to remain intubated and receive inotropic position of the great arteries purchase 100mg suhagra erectile dysfunction questions. Transposition of the great arteries and intact ventricular septum: anatomical can be extubated but must remain in the intensive care unit repair in the neonate suhagra 100 mg amex incidence of erectile dysfunction with age. Tetralogy of Fallot: underdevelopment of the pulmonary infundibulum and Second-Stage Arterial Switch its sequelae buy generic suhagra on-line impotence while trying to conceive. Double-outlet right switch other than the need to remove the band and to clip and ventricle: anatomic types and developmental implications based on a study of 101 autopsied cases. Intermediate Because the child who has had a Mustard or Senning has results of the arterial switch repair. J Thorac Cardiovasc Surg a normal arterial oxygen saturation it is not necessary to 1988;96:854–62. Nevertheless, these individuals can be quite unstable, par- Anatomic causes of pulmonary stenosis in complete transpo- sition. Anomalous origin of the left main coronary artery of sudden ventricular fbrillation unheralded by ventricular from the right sinus of Valsalva. Aortic intramural coronary artery in three hearts with transposition of the great arteries. Fate of intra- Between 1986 and 1988, 11 patients at Children’s Hospital mural coronary arteries after arterial switch operation. Thorac Boston underwent frst-stage preparation for a two-stage Cardiovasc Surg 2002;50:40–4. Semin Thorac median interval period was 9 days before the arterial switch Cardiovasc Surg Pediatr Card Surg Annu 2001;4:34–57. Early and mid- ventricular mass increased by a mean of 85% during this term results of the arterial switch operation for transposi- short interval. J Thorac Cardiovasc Surg pressure ratio was increased by the preparatory frst stage 1990;100:261–69. Anatomy of the coronary arter- stage procedure and no early deaths in the 10 patients who ies in transposition of the great arteries and methods for their had an arterial switch procedure. Coronary artery anatomy Late studies of ventricular function82 have documented that and transposition of the great arteries. Factors infuenc- slightly reduced relative to normal and relative to patients ing early and late outcome of the arterial switch operation for who have undergone a primary arterial switch procedure. J Thorac Cardiovasc Surg Today it is exceedingly rare that the situation arises where 1995;109:289–301. Arterial switch patients are generally in the gray zone of 4–8 weeks of age operation with a single coronary artery. J Thorac Cardiovasc where a primary arterial switch followed by support with a Surg 2002;123:1164–72. The tion for anatomical correction of transposition of the great pulmonary vascular bed in patients with complete transposi- arteries with intact interventricular septum. Reconstruction of the cular disease in complete transposition of the great arteries. Coronary artery pat- nary vascular disease in transposition of the great arteries. Enlarged bron- septostomy is associated with preoperative stroke in neonates chial arteries after early repair of transposition of the great with transposition of the great arteries. Ann Thorac gram: an improved angiographic view for demonstration of Surg 1993;55:1093–103. Moderate versus deep operative brain injuries do not worsen with surgery in neo- hypothermia for the arterial switch operation – experience nates with congenital heart disease. Primary arterial switch rial switch operation in patients with transposition of the great operation in children presenting late with d-transposition of arteries and abnormalities of the mitral valve or left ventricu- great arteries and intact ventricular septum. Eur J Cardiothorac Surg switch operation for transposition of the great arteries with 2003;24:1–9. J Thorac dictors of aortic root dilation and aortic regurgitation after Cardiovasc Surg 1993;106:111–15. Successful two stage correction of transposition in transposition of the great arteries: impact on outcome. Arrhythmias and operation in the treatment of transposition of the great intracardiac conduction after the arterial switch operation. Current quality of life after surgical repair of transposition of the results with the Mustard operation in isolated transposition of great arteries: atrial versus arterial switch operation. Length of stay the left ventricle after arterial switch operation for transposi- after infant heart surgery is related to cognitive outcome at age tion of the great arteries. Early results for anatomic correction ease on brain development and neurodevelopmental outcome. J Thorac Cardiovasc Surg tors infuencing early mortality of the arterial switch opera- 2007;133:461–9. J and complete transposition of the great arteries: a technical Thorac Cardiovasc Surg 2008;135:331–8. Eur J Cardiothorac Surg obstruction after the arterial switch operation for transpo- 2010;37:1239–45. Protooncogene induc- lowing the arterial switch operation for transposition of the tion and reprogramming of cardiac gene expression produced great arteries. Rapid, two-stage arte- anatomy after arterial switch operation for transposition of rial switch for transposition of the great arteries and intact the great arteries: detection by 16-row multislice computed ventricular septum beyond the neonatal period. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu of the perioperative neurologic effects of hypothermic circula- 2000;3:198–215. Patterns of devel- tolic mechanics late after an acute pressure overload stimulus opmental dysfunction after surgery during infancy to cor- in infancy. Developmental and and aortopulmonary shunt placement for transposition of the neurological status of children at 4 years of age after heart great arteries with low left ventricular pressure. Judgement of the left ventricle retraining in the rapid two stage-switch operation. Isolated primary congeni- tal aortic regurgitation where the valve itself is congenitally In Chapter 14, Choosing the Right Biomaterial, the many structurally abnormal is a relatively rare entity, certainly options available for valve replacement are described. Chapter 14 also emphasizes that all presently available valve replacement options have important disadvantages. Most Anatomy importantly, all replacement options including the Ross pro- Primary Congenital Aortic Valve Regurgitation cedure do not incorporate growth potential. For this reason, Congenital aortic valve regurgitation is often the result of valve repair is preferred for essentially all congenital valve 3,4 incomplete formation of a bicuspid valve. Although repair does not create a perfect valve nary leafet is frequently affected. It may be very hypoplastic it does allow the child to live a good quality life, free of the and incompletely fused with either the non or left leafet. The risk of thromboembolism and free of the need to take anti- resulting fused leafet may have poor commissural support coagulant medication. However, there is hope 1 secondary to the large volume load passing through the valve.
Our evolving knowledge of fundamental mechanisms has led to new and improved treatments and holds great promise for the development of future therapies purchase online suhagra erectile dysfunction medicine names. Updated Classification of Pulmonary Hypertension from the 5th World Symposium on Pulmonary Hypertension in Nice generic suhagra 100 mg erectile dysfunction treatment medications, France in 2013 discount suhagra online american express erectile dysfunction treatment in mumbai. A variety of physiologic factors appeared to contribute to the severity and rate at which vascular disease developed in patients with congenital heart defects (Table 65. The term plexogenic arteriopathy or plexiform lesions has been adopted to refer to those occlusive and dilatation lesions containing expansion of smooth muscle- and endothelial-like cells. Curiously, there have been reports of late progression of pulmonary vascular disease in infants with transposition of the great arteries even after successful and timely surgical correction. Patients with cyanotic heart defects who had large, surgically created systemic-to-pulmonary artery shunts were also at risk for pulmonary vascular disease. Several investigators tried to quantify the degree of medial hypertrophy, but their measurements did not correlate closely with the preoperative level of pulmonary vascular resistance or with its change postoperatively (4). Structural Remodeling and Growth Beginning in 1965, a new and quantitative method of analysis of the pulmonary vascular bed was developed that was particularly applicable to the study of infants and young children because it incorporated features of altered growth of the pulmonary circulation. This method was based upon extensive studies carried out using a technique of radiopaque barium–gelatin arterial injection of a postmortem lung specimen. It was observed from the postmortem arteriograms that the vessels are prominent in the newborn, whereas in the adult they are obscured by a dense background haze produced by the addition of many small intra-acinar arteries not present at birth (5). On microscopic examination, three features of normal remodeling and growth of the pulmonary vascular bed were established (6). With increasing age, muscle is observed in arteries located more peripherally within the acinus. At first, nonmuscular arteries become partially muscular, and later they become fully muscularized. At birth, the muscularized arteries are thick walled, but within a few days, the smallest muscular arteries dilate, and their walls thin to adult levels. When infants are 4 months of age, this process has included the largest muscular pulmonary arteries and is complete. Although alveoli also proliferate, the ratio of alveoli to arteries actually decreases from the newborn value of 20:1 to the value of 8:1, which is achieved first in early childhood and which persists (Fig. Tenascin-C, proliferation and subendothelial fibronectin in progressive pulmonary vascular disease. Lung biopsy in congenital heart disease: a morphometric approach to pulmonary vascular disease. Morphometric analysis of the lungs of patients with congenital heart defects revealed disturbed growth and remodeling of the pulmonary vascular bed (Table 65. On microscopic examination of the pulmonary vascular bed, muscle had extended precociously into normally nonmuscular peripheral arteries, regression of the perinatal musculature had not occurred, and there was additional medial hypertrophy. Also, the peripheral arteries had not grown normally in that they were small and few. Because there were no regional variations in the lung, it was feasible to apply the morphometric technique to analysis of lung biopsy tissue in assessing abnormal muscularity and evaluating arterial size and number (8). Lung Biopsy Lung biopsy studies indicated that the severity of altered growth and development of the pulmonary vascular bed correlates with the hemodynamic state. With grade A, there is abnormal extension of muscle into small peripheral arteries, or, in addition, there is a mild increase in wall thickness of the normally muscular arteries (<1. These patients have increased pulmonary blood flow and increased pulse pressure but normal mean pulmonary artery pressure. Meyrick and Reid (9) showed from ultrastructural studies of lung biopsy tissue that this change is due to precocious differentiation of pericytes to mature smooth muscle cells in the nonmuscular region of the artery and the intermediate cell in the partially muscular region. Because arteries become more muscular as they increase in size, it is tempting to speculate that, in the altered hemodynamic setting of chronic high flow and high pressure, “stretch” is the stimulus for smooth muscle cell differentiation from precursor cells. With grade B, as in grade A, there is increased extension of muscle, but, in addition, there is more severe medial hypertrophy of normally muscular arteries. The medial thickness is due to hypertrophy as well as hyperplasia of pre- existing smooth muscle cells and also to an increase in the intercellular connective tissue proteins. With grade C, in addition to the findings of severe grade B, arterial concentration and usually artery size are 2 reduced. Patients with these changes generally have a pulmonary vascular resistance of greater than 3. When the artery number is less than half of normal (severe grade C), pulmonary vascular resistance values are 2 often in excess of 6 U·m. The basis for grade C is likely the failure of new vessels to grow normally, although some loss of arteries also may occur. Morphometric grades A and B are refinements of Heath–Edwards grade I; grade C is a new feature that also appears to be of important functional significance. Whether and to what extent abnormal growth and structural remodeling of the pulmonary vascular bed are permanent and result in persistent pulmonary hypertension was estimated by correlating these features with postoperative hemodynamic studies. The quantitative features of abnormal growth and remodeling of the pulmonary arteries and the qualitative changes described by Heath and Edwards correlate with the hemodynamic behavior of the pulmonary circulation in the immediate postoperative period in the intensive care unit 1 day after repair and at the time of routine cardiac catheterization study 1 year later (10). Patients with grade A or mild grade B changes have normal pulmonary artery pressures in the early postoperative period or only a minimal degree of elevation. The pulmonary hypertension is frequently labile and almost always can be controlled; the mechanism and treatment are discussed in the next section. One year after repair, however, patients operated within the first 8 months of life tend to have normal pulmonary hemodynamics regardless of the severity of vascular changes on lung biopsy, as do patients with severe grade B (Heath–Edwards I) abnormalities, regardless of their age at repair. While not often used clinically in the current era, quantitative techniques have been applied successfully to the analysis of lung biopsy tissue prepared by frozen section to aid decision making between a palliative or corrective procedure when preoperative hemodynamic data are borderline or difficult to obtain or to interpret. The ability to predict whether even mild elevation in pulmonary vascular resistance will be present postoperatively is of P. Patients with tricuspid atresia who have had previous systemic-to-pulmonary artery shunts and those with single-ventricle and previous pulmonary artery bands are at particular risk. Even minor vascular changes on lung biopsy tissue (mild grade B) are associated with increased morbidity after the Fontan procedure, as gauged by prolonged hospitalization; the need for increased ventilator support; and drainage from chest tubes (unpublished observations). This highlights the need for more sensitive noninvasive techniques to determine the presence of pulmonary vascular disease in this population. The dashed vertical lines separate the normal from the abnormally elevated pressure values, and the dotted horizontal lines separate the biopsy grades. Note that with the more severe Heath–Edwards changes on lung biopsy tissue, there is a trend toward a greater proportion of patients with elevated pulmonary arterial pressures and higher values. B: Graph correlating lung biopsy grade with pulmonary vascular resistance 1 year after cardiac repair. Patients who underwent repair within the first 8 months of life, but not those operated on later, had normal pulmonary vascular resistance regardless of the severity of their structural changes. Vascular structure in lung biopsy tissue correlated with pulmonary hemodynamic findings after repair of congenital heart defects. A technique has been described that allows quantitative assessment of abnormalities in a pulmonary wedge angiogram (12). A balloon catheter is directed to the origin of the axial artery of the posterior basal segment of the right lower lobe; contrast material is injected, and the injection is filmed on biplane cineangiography. The rate of tapering of the arteries is assessed by measuring the length of a segment over which the lumen diameter narrows from 2.
However order suhagra cheap erectile dysfunction urethral medication, the achievement of comprehensive care for these patients has been elusive purchase suhagra 100mg amex erectile dysfunction drugs india. Below is a review of the empirical basis for psychosocial interventions and a working model of psychosocial needs for pediatric device patients buy generic suhagra 100 mg online erectile dysfunction pump on nhs. Data evaluating the outcomes of psychological interventions in pediatric patients with heart disease are limited and more so in pediatric device patients. However, exercise training did not improve anxiety, depression, or externalizing behaviors. Disease self-management groups are common in other areas of pediatric medicine and have generally been shown as helpful in reducing disease burdens in areas such as epilepsy, diabetes, and asthma (46,47,48,49,50). Mean tailored cardiac rehabilitation significantly longer in cardiac rehab (2003) age = therapy group (p = 0. However, the goal of fully addressing the patient and family adjustment to the disease and device is worth pursuing. To address this, we suggest a working framework in which the majority of the psychosocial issues associated with cardiac devices could be conceptualized as an interconnected triad of fears in the categories of “Self,” “Device/Disease,” and “Relationship to Society/Peers” (Fig. Fears relating to “Self” can include issues with self-image (perceiving oneself as “different”), body image, self-esteem, and coping with personal limitations, whether self-imposed or medically mandated. For a young person, and particularly for adolescents, whose emerging identity is strongly influenced by peers and their surroundings, the concerns about “Relationships to Society/Peers” are particularly important. These may include fear of not belonging to their peer group, fear of being perceived as different, frustrations with parental overprotection, and the challenges of dealing with isolation, rejection, and discrimination. Creating a clinical safety net for our pediatric device patients can be initiated with attention to this triad of fears. We suggest that the conceptualization of fears leads to specific clinical actions that P. For clinicians, the first step is to acknowledge that most pediatric patients with an implantable cardiac device are at risk of psychosocial sequelae. Discussions of stress, anxiety, and activity should be integrated into the visit with a goal of recognizing patient and family distress. Demonstrating openness and confidence in referring for psychological assessment and treatment is key. Finally, we suggest that a set of clinical strategies for routine maintenance of care “beyond the device” can be instituted. Educating the patient and family about the disease and device, including the development of a “shock plan,” can empower families by eliminating some elements of the unknown. Ensuring age-appropriate device programming and reassessing activity restrictions on an individual basis allow the clinician to advocate more confidently for increased physical activity in those patients who have limited themselves due to avoidance. In those whose condition mandates limitations, focus on improving quality of life by exploring skills and identifying interests within the constraints of their device and disease. Consider recommending participation in cardiac disease–specific camps, which may restore some sense of “belonging” to patients who feel isolated by their disease (54,55). Finally, refer for psychological evaluation and therapy with an emphasis on normalizing patient and family stress. Recognize and normalize pediatric patient and family distress Consider risk and resilience factors to promote adjustment Provide supportive care as a healthcare team by reinforcing/praising personal coping efforts of patients and families Demonstrate openness and familiarity with referring for psychosocial care Encourage behavioral activation in patients and families Concentrate on and develop conversation on quality-of-life activities vs. The current chapter identified common challenges for pediatric patients with devices including differences in quality of life, psychological distress, and social functioning that warrant additional clinical consideration and research. Many of the fears of pediatric device patients can be conceptualized as an interconnected triad of fears in the categories of “Self,” “Device/Disease,” and “Relationship to Society/Peers. Machines in Our Hearts: The Cardiac Pacemaker, the Implantable Defibrillator and American Health Care. Implantation trends and patient profiles for pacemakers and implantable cardioverter defibrillators in the United States: 1993–2006. Cardiac rhythm devices in the pediatric population: utilization and complications. Implantable cardioverter defibrillator criteria for primary and secondary prevention of pediatric sudden cardiac death. Sudden cardiac death and the use of implantable cardioverter- defibrillators in pediatric patients: The pediatric electrophysiology society. Pediatric bridge to heart transplantation: Application of the Berlin Heart, Medos and Thoratec ventricular assist devices. Mechanical left ventricular support as a bridge to cardiac transplantation in childhood. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Patient acceptance of the implantable cardioverter defibrillator in ventricular tachyarrhythmias. Securing life through technology acceptance: The first six months after transvenous internal cardioverter implantation. Health related quality of life and social support in pediatric patients with pacemakers. Psychosocial aspects of caring for pediatric pacemaker recipients and their families. Quality of life in pediatric patients with implantable cardioverter defibrillators. Perceived self-competence, psychosocial adjustment, and quality of life in pediatric patients with pacemakers. Quality of life and functional capacity after long-term right ventricular pacing in pediatrics and young adults with congenital atrioventricular block. Psychiatric functioning and quality of life in young patients with cardiac rhythm devices. Implantable cardioverter defibrillator therapy for life-threatening arrhythmias in young patients. Psychosocial factors and quality of life in children and adolescents with implantable cardioverter-defibrillators. Psychological functioning and disease-related quality of life in pediatric patients with an implantable cardioverter defibrillator. Acceptance and psychological impact of implantable defibrillators amongst adults with congenital heart disease. Outpatient left ventricular assist device support: A destination rather than a bridge. Recovery of major organ function in patients awaiting heart transplantation with Thoratec ventricular assist devices. Assessment of submaximal exercise capacity in patients with left ventricular assist devices. Exercise performance in patients with end-stage heart failure after implantation of a left ventricular assist device and after heart transplantation: an outlook for permanent assisting?
Buy suhagra 100mg. How to cure Erectile Dysfunction with no Viagra for VEGANS.