
College of Idaho. Z. Zarkos, MD: "Purchase online Female Cialis cheap no RX - Trusted online Female Cialis OTC".
In patients with cystic fibrosis order female cialis with mastercard menstruation underwear, even with normal lung function buy discount female cialis line womens health magazine recipes, resection should be avoided because repeated episodes in other areas are likely to occur discount 10mg female cialis overnight delivery breast cancer jersey. A patient with a 1-second forced expiratory volume of less than 2 L or a maximum voluntary ventilation of less than 50% of predicted should not undergo surgery unless split-lung function studies reveal that the patient is not likely to be left a respiratory cripple because of disabling dyspnea. With respect to surgery, it is clear that no treatment preference can be recommended for all patients on the basis of reported studies. The trials of therapy span different decades of practice, have widely differing causes of hemoptysis in their populations, and use several different definitions for massive hemoptysis. A review of the literature suggests the following strategy: (a) patients who are not candidates for surgery because of their pulmonary function, general medical condition, or diffuse nature of their lesions should be treated with selective embolization; (b) resectional surgery should be performed in operable patients when surgery is the definitive treatment for the underlying disease; and (c) all potentially operable patients who continue to bleed at rates of more than 1 L per day despite supportive, conservative care and subsequent embolization should undergo surgical resection. The correct therapy in a given patient depends on the cause of the bleeding, lung function, availability of resources, and local expertise. When corticosteroid therapy is given alone for critically ill patients with immunologic lung diseases, the dose is 1 mg/kg/d of intravenous methylprednisolone or the equivalent dose of another corticosteroid. In general, corticosteroids should be administered initially in round-the-clock divided doses until substantial improvement has occurred. When combined corticosteroid and cytotoxic drug therapy is given, it is usually prescribed for immunologic lung diseases caused by vasculitides (e. Sakr L, Dutau H: Massive hemoptysis: An update on the role of bronchoscopy in diagnosis and management. Savale L, Parrot A, Khalil A, et al: Cryptogenic hemoptysis: from a benign to a life-threatening pathologic vascular condition. Remy J, Remy-Jardin M, Voisin C: Endovascular management of bronchial bleeding; in Butler J (ed): the Bronchial Circulation. Saumench J, Escarrabill J, Padro L, et al: Value of fiberoptic bronchoscopy and angiography for diagnosis of the bleeding site in hemoptysis. De Lassence A, Fleury-Feith J, Escudier E, et al: Alveolar hemorrhage: diagnostic criteria and results in 194 immunocompromised hosts. Ewig S, Soler N, Gonzalez J, et al: Evaluation of antimicrobial treatment in mechanically ventilated patients with severe chronic obstructive pulmonary disease exacerbations. Hamaguchi S, Nakajima Y: Two cases of tracheoinnominate artery fistula following tracheostomy treated successfully by endovascular embolization of the innominate artery. Valipour A, Kreuzer A, Koller H, et al: Bronchoscopy-guided topical hemostatic tamponade therapy for the management of life-threatening hemoptysis. Exceptions are a large hemothorax for monitoring bleeding rate and hemodynamic status and an unstable secondary spontaneous pneumothorax or large unilateral or bilateral pleural effusions that have caused acute respiratory failure. A pleural effusion may not be seen on the supine chest radiograph because a diffuse alveolar filling process can mask the posterior layering of fluid or because bilateral effusions without parenchymal infiltrates are misinterpreted as an underexposed film or objects outside the chest. Pneumothorax may remain undetected in the supine patient because pleural air tends to be situated anteriorly and does not produce the diagnostic visceral pleural line seen on an upright radiograph. When the patient on mechanical ventilation is at increased risk for barotrauma because airway pressures are high, the index of suspicion for pneumothorax should be heightened; if there is evidence of pulmonary interstitial gas (see the following discussion) or subcutaneous emphysema, appropriate radiologic studies should be obtained. When chest radiographs are obtained in other than the erect position, free pleural fluid and air change position and result in a different radiographic appearance. Furthermore, when in the supine position, breast and pectoral tissue tend to fall laterally away from the lung base. Thus, an effusion should be suspected if there is increased homogeneous density over the lower lung fields compared to the upper lung fields. However, failure of chest wall tissue to move laterally, cardiomegaly, prominent epicardial fat pad, and lung collapse or consolidation may obscure a pleural effusion on a supine radiograph. An absent pectoral muscle, prior mastectomy, unilateral hyperlucent lung, scoliosis, previous lobectomy, hypoplastic pulmonary artery, or pleural or chest wall mass may lead to unilateral homogeneous increased density and mimic an effusion. Approximately 175 to 525 mL of pleural fluid results in blunting of the costophrenic angle on an erect radiograph. This quantity of effusion can be detected on a supine radiograph as an increased density over the lower lung zone. Failure to visualize the hemidiaphragm, absence of the costophrenic angle meniscus, and apical capping are less likely to be seen with effusions of less than 500 mL [1]. The major radiographic finding of a pleural effusion in a supine position is increased homogeneous density over the lower lung field that does not obliterate normal bronchovascular markings, does not show air bronchograms, and does not show hilar or mediastinal displacement until the effusion is massive. C: A complex, septae pleural effusion seen in a patient with severe sepsis owing to the presence of an empyema. D: A complex pleural effusion with an anechoic area assoicated with an increased echogenic density in the dependent area of the fluid collection. This is called the “hematocrit sign” and occurred in a patient who developed a hemothorax as a result of extravascular migration of a central line into the pleural space. Patients with multiple lines or compromised hemodynamic and oxygenation status will be difficult to position sitting upright in bed. One option is for the examiner to place the transducer in the posterior axillary line while angling the probe up toward the center of the body to visualize smaller effusions. For unstable patients who have effusions that are difficult to visualize, positioning the patient in a lateral decubitus position may be helpful. The examiner should always use a systematic approach to identify the following three findings to confirm the presence of a pleural effusion (see Video 1-25 in Chapter 12 Cases). Anatomic boundaries: An identification of the diaphragm and subdiaphragmatic organs (the liver or the spleen, depending on the side), the chest wall, and the lung, which should be clearly differentiated from the pleural effusion. Echo-free space: the relatively echo-free space surrounded by typical anatomic boundaries is the pleural effusion. Another characteristic sign of pleural effusions is the plankton sign, which is caused by swirling debris agitated by cardiac or respiratory motion in a pleural effusion. In the case of parapneumonic effusions, these findings typically indicate the presence of a complicated parapneumonic effusion or an empyema [7]. The base, lateral chest wall, and juxtacardiac area should be carefully visualized for evidence of pneumothorax. An erect or a decubitus (suspected hemithorax up) radiograph should be obtained to assess for the presence of a pneumothorax. Among individuals without pneumothorax, the lung– chest wall interface, which represents a to-and-fro movement synchronized with respiration, can be identified. However, the absence of lung sliding may be caused by the presence of large bullae or pleural symphysis caused by previous pleurodesis or pleural adhesions as a result of previous pleural disease. Hence, the absence of lung sliding is not specific for pneumothorax, but detection of lung sliding reliably excludes the presence of pleural air in the examined area. We recommend that preprocedural scanning be performed to determine the presence of lung sliding prior to the placement of a central venous line. The presence of lung sliding before and after the placement of a central venous catheter is reassuring for excluding an iatrogenic pneumothorax. Underlying lung disease may prevent total lung collapse, even if tension is present; for patients on mechanical ventilation, little or no midline mediastinal shift may result from the tension. Among the latter, a depressed ipsilateral diaphragm is a more reliable sign of tension than mediastinal shift.
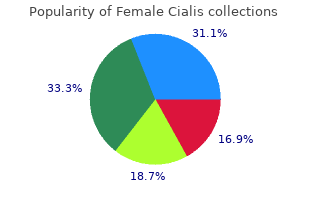
Issuance of a “card” is neither a license to perform these techniques nor a guarantee of skill order female cialis amex breast cancer 3 day walk, but simply an acknowledgment that an individual attended a specific course and passed the required tests purchase cheap female cialis on line pregnancy ultrasound at 7 weeks. If employers or government agencies require such a card of their health workers purchase line female cialis breast cancer x ray, it is by their own mandate. A major focus of the 2010 guidelines is on the supremacy of effective compressions, with limited interruptions. Respiratory Arrest Respiratory arrest may result from airway obstruction, near-drowning, stroke, smoke inhalation, drug overdose, electrocution, or physical trauma. The heart usually continues to circulate blood for several minutes, and the residual oxygen in the lungs and blood may keep the brain viable. Early intervention by opening the airway and providing ventilation may prevent cardiac arrest and may be all that is required to restore effective respiration. In the intubated patient, careful suctioning of the airway and attention to the ventilator settings are required. Lay rescuers should not check for a pulse, but if a health care professional ascertains that the patient does have a pulse, then rescue breaths should be performed at a rate of one breath every 5 to 6 seconds while arranging for more definitive airway management. This mnemonic is useful for teaching the public, but it should be remembered that each step is preceded by assessment of the need for intervention: before starting compressions, the rescuer determines unresponsiveness; before breathing, the rescuer determines breathlessness (Table 14. Simultaneous High airway pressures of 60–110 mm Hg [14,16] chest are used to augment carotid flow, compression and requiring intubation and a mechanical lung inflation ventilator. Studies have demonstrated adverse effects on coronary perfusion, cerebral oxygenation, and canine resuscitation Redding [17] Koehler et al. High impulse and high compression rates can result in rescuer fatigue and increased injury Cohen et al. In either case, the rescuer must react promptly to assess the person’s responsiveness by attempting to wake and communicate with the person by tapping or gently shaking and shouting. Early recognition of cardiac and respiratory arrests is facilitated by electronic and video monitoring. Unfortunately, it is quite possible for a patient to become lost behind this profusion of electronic signals, the dependability of which varies widely. The overall efficacy of the monitoring devices depends highly on meticulous skin preparation and care of electrodes, transducers, pressure cables, as well as caregiver response to alarms. Sudden apparent loss of consciousness, occasionally with seizures, may be the first signal of arrest and requires prompt reaction. After determining unresponsiveness, the pulse is assessed by a health care provider for no more than 10 seconds. Compressions should be performed at a rate of 100 per minute, compressing the chest 2 inches with each repetition and allowing the chest to recoil fully. Interruptions to compressions should only be allowed for essential interventions, such as intubation or defibrillation. Meticulous attention to establishing an airway and supplying adequate ventilation is essential to any further resuscitative effort. The team leader must carefully monitor the adequacy of ventilation, as well as direct the resuscitative effort. Because considerable cervical hyperextension occurs, this method should be avoided in patients with cervical injuries or suspected cervical injuries. The jaw-thrust maneuver provides the safest initial approach to opening the airway of a patient with a cervical spine injury; it usually allows excellent airway opening with a minimum of cervical extension. The angles of the mandible are grasped using both hands and lifting upward, thus tilting the head gently backward. Rescue Breathing If spontaneous breathing is absent, rescue breathing with an airway– mask–bag unit must be initiated (see Chapter 8). If equipment is immediately available and the rescuer is trained, intubation and ventilatory adjuncts should be used initially. Each breath should be delivered during 1 second, allowing the patient’s lungs to deflate between breaths. A rate of 10 to 12 breaths per minute is maintained for as long as necessary, with tidal volumes of approximately 600 mL. Delivering the breath during 1 second helps to prevent gastric insufflation compared with faster delivery. If the patient wears dentures, they are usually best left in place to assist in forming an adequate seal. If air cannot be passed into the patient’s lungs, another attempt at opening the airway should be made. If subsequent attempts at ventilation are still unsuccessful, the patient should be considered to have an obstructed airway and attempts should be made to dislodge a potential foreign body obstruction. Chest Compressions Artificial circulation depends on adequate chest compression through sternal depression. The safest manner of depressing the sternum is with the heel of the rescuer’s hand at the nipple line, with the fingers kept off the rib cage. It is usually most effective to cover the heel of one hand with the heel of the other, the heels being parallel to the long axis of the sternum. If the rescuer’s hands are placed either too high or too low on the sternum, or if the fingers are allowed to lie flat against the rib cage, broken ribs and organ laceration can result. Although it is important to allow the chest to recoil to its normal position after each compression, it is not advisable to lift the hands from the chest or change their position. The rescuer’s elbows should be kept locked and the arms straight, with the shoulders directly over the patient’s sternum. This position allows the rescuer’s upper body to provide a perpendicularly directed force for sternal depression. In large patients, a slightly greater depth of sternal compression may be needed to generate a palpable carotid or femoral pulse. At the end of each compression, pressure is released and the sternum is allowed to return to its normal position. Equal time should be allotted to compression and relaxation with smooth movements, avoiding jerking or bouncing the sternum. One rescuer, positioned at the patient’s side, performs sternal compressions, while the other, positioned at the patient’s head, maintains an open airway and performs ventilation. Lay people have not been routinely taught this method in the interest of improving retention of basic skills. When the rescuer performing compressions is tired, the two rescuers should switch responsibilities with the minimum possible delay. Awareness of these potential complications is important to the postresuscitative care of the arrest patient. Gastric distention and regurgitation are common complications of artificial ventilation without endotracheal intubation. These complications are more likely to occur when ventilation pressures exceed the opening pressure of the lower esophageal sphincter. Although an esophageal obturator airway may decrease the threat of distention and regurgitation during its use, the risk is increased at the time of its removal. To obviate this risk, the trachea should be intubated and protected with an inflated cuff before the esophageal cuff is deflated and the esophageal obturator removed. Complications of sternal compression and manual thrusts include rib and sternal fractures, costochondral separation, flail chest, pneumothorax, hemothorax, hemopericardium, subcutaneous emphysema, mediastinal emphysema, pulmonary contusions, bone marrow and fat embolism, and lacerations of the esophagus, stomach, inferior vena cava, liver, or spleen [46].
Order 20 mg female cialis with visa. WATCH | Child ripped from woman's arms by police as refugees removed from UNHCR offices.
This rhythm strip should reveal1 the conduction pattern between atria and ventricles as antegrade generic female cialis 10mg online pregnancy after vasectomy, simultaneous order female cialis with visa womens health boulder, retrograde discount 10mg female cialis free shipping menstrual cycle 8 days apart, or dissociated. Bradyarrhythmias unresponsive to medical treatment that result in hemodynamic compromise or symptoms require urgent treatment. Action: There are four possible actions, or therapeutic options, listed and classified for each bradyarrhythmia or conduction problem: 1. In general, because the increase in sinus rate with atropine is unpredictable, this is to be avoided unless there is symptomatic bradycardia that will likely respond to a vagolytic agent, such as sinus bradycardia or Mobitz I, as denoted by the asterisk, above. It is assumed, but not specified in the table, that at the discretion of the clinician, transcutaneous pads will be applied and standby transcutaneous pacing will be in effect as the patient is transferred to the fluoroscopy unit for temporary transvenous pacing. Level of Evidence: This table was developed from published observational case reports and case series, published summaries, not meta-analyses, of these data; and expert opinion, largely from the prereperfusion era. The left anterior descending artery is the major blood supply to the His bundle and the bundle branches, and an anterior wall infarction with new bundle branch block represents extensive myocardial damage and confers an increased risk of heart failure and mortality. Thrombolytic therapy or percutaneous coronary intervention takes precedence over placement of prophylactic cardiac pacing, because prophylactic pacing has not been shown to improve mortality. Transthoracic (transcutaneous) cardiac pacing is safe and usually effective [10], and would be a reasonable alternative to prophylactic transvenous cardiac pacing, particularly soon after the administration of thrombolytic therapy. Transvenous pacing of the right ventricle or right atrium with a pacing catheter or modified pulmonary artery catheter is the most widely used technique; intraesophageal, transcutaneous, and epicardial pacing techniques are also available. Transvenous Pacing Catheters Some of the many transvenous pacing catheters available for use in the critical care setting are illustrated in ure 18. In urgent situations, or where fluoroscopy is unavailable, a flow-directed flexible balloon-tipped catheter. After gaining access to the central venous circulation (Chapter 6), the catheter is passed into the vein and the balloon inflated. After advancing the catheter into the right ventricle, the balloon can be deflated and the catheter tip advanced to the right ventricular apex. Although the balloon-tipped catheter may avoid the need for fluoroscopy, placement may be ineffective in the setting of low blood flow during cardiac arrest or in the presence of severe tricuspid regurgitation. This lead is positioned by “hooking” it in the right atrial appendage under fluoroscopic guidance, providing stable contact with the atrial endocardium. Utility of Ultrasonography for Transvenous Pacemaker Insertion Ultrasonography has useful applications related to transvenous pacemaker insertion. Real-time guidance of pacemaker insertion with ultrasonography is a safe, effective, and fast way to perform the procedure. It has advantage over fluoroscopic guidance, because it requires no patient transport or complex equipment and can be performed at the bedside of the critically patient. Ultrasonography guided insertion is performed more rapidly and with fewer complications than with fluoroscopic control [13,16]. If a femoral approach is used, the longitudinal view of inferior vena cava permits visualization of the pacer wire (Chapter 18 Video 18. In intubated patients with inadequate image quality from transthoracic images, transesophageal echocardiography is an effective alternative. Esophageal Electrode An esophageal “pill” electrode allows atrial pacing and recording of atrial depolarizations without requiring central venous cannulation. Because the electrode can be uncomfortable and may not give consistent, stable capture, the esophageal electrode is typically limited to short-term use for diagnosis of arrhythmias in pediatric patients. Transcutaneous External Pacemakers Transcutaneous external pacemakers have external patch electrodes that deliver a higher current (up to 200 mA) and longer pulse duration (20 to 40 ms) than transvenous pacemakers. Transcutaneous external pacemakers have been used to treat bradyasystolic cardiac arrest, symptomatic bradyarrhythmias, and overdrive pacing of tachyarrhythmias and prophylactically for conduction abnormalities during myocardial infarction. They may be particularly useful when transvenous pacing is unavailable, as in the prehospital setting, or relatively contraindicated, as during thrombolytic therapy for acute myocardial infarction [17]. These electrodes are routinely placed electively during cardiac surgical procedures for use during the postoperative period. Because ventricular capture is not always reliable, in patients with underlying asystole or an unstable escape rhythm additional prophylactic transvenous pacing should be considered. Because these generators have atrial sensing/inhibiting capability, they are also set with an upper rate limit (to avoid rapid ventricular pacing while “tracking” an atrial tachycardia); in addition, an atrial pacing refractory period may be programmed (to avoid pacemaker-mediated/endless loop tachyarrhythmias). In patients with noncompliant ventricles (ischemic heart disease, left ventricular hypertrophy, aortic stenosis, and right ventricular infarction), loss of the atrial contribution to ventricular stroke volume (the atrial “kick”) during ventricular pacing may result in increased atrial pressure;and intermittent mitral and tricuspid regurgitation with reduced cardiac output and blood pressure. The balloon is inflated in the superior vena cava, and the catheter is advanced while observing the recorded intracardiac electrogram. When the tip of the catheter reaches the right ventricle, the balloon is deflated and the catheter advanced to the right ventricular apex. With the ventricular electrode appropriately positioned at or near the apex of the right ventricle, a pacing threshold of less than 0. Possible causes of a high pacing threshold include relatively refractory endomyocardial tissue (fibrosis) or, most commonly, unsatisfactory positioning of the pacing electrode. The tip of the pacing electrode should be repositioned in the region of the ventricular apex until satisfactory ventricular capture at a current of less than 1. The ventricular output is set to exceed the threshold current at least threefold to guarantee uninterrupted ventricular capture despite any modest increase in the pacing threshold. The sensitivity is then set at a level slightly below the determined threshold and the pacing rate reset to the minimum desired ventricular rate. The atrial current is set to 20 mA and the atrial pacing rate adjusted to at least 10 beats per minute greater than the intrinsic atrial rate. As long as the atrial pacing rate continually exceeds the intrinsic sinus rate, the atrial P wave activity should track with the atrial pacing spike. Appropriate selection of the optimal route requires an understanding of the results and complications of each technique. Complications of temporary pacing from any venous access route include pericardial friction rub, arrhythmia, right ventricular perforation, cardiac tamponade, infection, unintentional arterial injury, diaphragmatic stimulation, phlebitis, and pneumothorax. The Mayo Clinic experience revealed that percutaneous cannulation of the right internal jugular vein provided the simplest, most direct route to the right- sided cardiac chambers [25]. Complications of internal jugular venous cannulation may include pneumothorax, carotid arterial injury, venous thrombosis, and pulmonary embolism (Chapter 6) [26]. These risks are minimized by use of ultrasound, knowledge of anatomic landmarks adherence to proved techniques, and use of a small-caliber needle to localize the vein before insertion of the large-caliber needle (for a full discussion, see Chapter 6). Full-dose systemic anticoagulation, thrombolytic therapy, and prior neck surgical procedures are relative contraindications to routine internal jugular vein cannulation. Percutaneous subclavian venipuncture is also frequently used for insertion of temporary pacemakers [27]. This approach should be avoided in patients with severe obstructive lung disease or a bleeding diathesis (including thrombolytic therapy), in whom the risk of pneumothorax or bleeding is increased. The femoral venous approach is used for electrophysiologic studies or during cardiac catheterization when the catheter is left in place for only a few hours. This approach is less desirable when long-term cardiac pacing is required, because there is a risk of deep venous thrombosis or infection.
This is particularly pertinent considering the the main histological subtypes are shown in Table 62 discount female cialis 20mg line women's health center greensburg pa. In particular purchase generic female cialis on-line menstruation spotting, the use of adjuvant tamoxifen in breast cancer has been proposed to be associated with some Endometrial hyperplasia of the rarer tumours such as mixed Müllerian tumours order female cialis in united states online menstrual mood swings, Hyperplasia is defined as excessive proliferation of normal now called carcinosarcomas. There are no specific indi- cells, and atypical hyperplasia is associated with a high risk cators regarding the other subtypes. In a number of series, the risk of are usually an unexpected finding following removal of underlying malignancy has been shown to be higher than a fibroid uterus. Thus it may be preferable to consider these patients as having endometrial cancer and expedite surgery. Type I Clinical presentation Premenopausal and perimenopausal women History of unopposed oestrogen exposure Endometrial hyperplasia Postmenopausal bleeding is the commonest presentation Minimally invasive, low‐grade endometrioid type in endometrial cancer, and up to 10% of these women Good prognosis will have a diagnosis confirmed. However, many use a cut‐off of 4mm, based on cost‐efficacy and detection Table 62. Sampling can be undertaken in three ways: Pipelle, outpatient hysteroscopy or hysteroscopy and curettage Endometrioid adenocarcinoma, 50–60% under a general anaesthetic. All methods of sampling Adenosquamous, 6–8% will miss some cancers but the rate of failure is not sig- Serous papillary, 18% nificantly different between outpatient sampling and Sarcomas/leiomyosarcomas, 3–5% hysteroscopy. Naturally, avoiding a general anaesthetic is Carcinosarcomas, 2–3% preferable where possible and only patients in whom an Clear cell, 1–6% endometrial sample cannot be obtained in outpatients Endometrial Cancer 879 field is associated with a worse prognosis. Other sub- Besides these investigations, cystoscopy, sigmoidos- types recognized as more aggressive include papillary copy and an examination under anaesthetic are all part serous and clear cell tumours, accounting for 10–15% of of the staging procedure. In most cases adjuvant therapies (after can be staged both clinically and surgically, with surgical surgery) would be considered. In some rare cases of sarcomas, preoperative diagnosis may be suspected when the endometrial sampling indi- Surgical interventions cates this diagnosis histologically, or when a preopera- tive chest X‐ray shows evidence of metastatic disease, Surgery remains the primary intervention for endome- normally called ‘cannon‐ball’ metastases. Whilst radiotherapy is an alternative, from ation of the disease is also important, as the grade in retrospective case–control studies it would seem that association with other factors will influence the recom- surgery affords a better survival outcome. The removal of the uterus and (normally) the ovaries Management is the recommended basic surgical procedure. This may be performed by open laparotomy or by a laparoscopic Preoperative investigations approach. As part of stag- become part of the surgical approach, but the consensus ing, there are agreed preoperative investigations which is that where possible the minimally invasive approach can be performed. Also, clamping/ligating the fallopian tubes at com- disease exists, which may influence the role of surgery. However, a vagina‐only approach will not permit access to the pelvic lymphatics, Table 62. The combination of chemoradiotherapy There has only been one prospective randomized trial increases morbidity, and in endometrial cancer this poses reported on lymphadenectomy in endometrial cancer. The study included two parts: (i) ovarian cancer for some decades, has been reported in patients randomized to pelvic lymhadenectomy or not, some small series in endometrial cancer, with a sugges- and (ii) patients randomized to adjuvant pelvic radio- tion that a smaller residual tumour load correlated with therapy or not in high‐risk cases. The patient cohort receiving radiotherapy were not this should be considered accepted therapy for endo- necessarily those recruited to the surgical aspects of the metrial cancer at present. The conclusions were interesting in that the use of disease, removal of the uterus may yield immediate alle- lymphadenectomy did not alter survival rates, and viation of symptoms such as persistent vaginal bleeding, indeed it was suggested that it may have a negative which could justify the intervention. Also, the number of lymph nodes retrieved did not influence Fertility‐sparing surgery outcome. Although the study was confined to patients As women are increasingly delaying having children, with disease localized to the uterus (based on clinical the issue of fertility‐sparing options has become more examination and imaging in some cases), it does indicate common, and this is relevant to many other malignan- that lymphadenectomy should not be undertaken in this cies. Longer‐term outcomes Lymphadenectomy and non‐randomized studies are equally lacking and therefore before embarking on There are many non‐randomized reports on the role of this therapeutic option, it is imperative to provide the lymphadenectomy of pelvic and para‐aortic nodes in patient with advice based on current information and endometrial cancer. All these studies naturally suffer the ‘unknown’ risks, particularly as this is a deviation from the fact that there are no randomized controlled from the normal recommended intervention that could trials. Some groups suggest that, in particular, para‐ potentially exclude the patient from a recommended aortic nodal excision has a therapeutic effect, based on curative therapy. Women were tion either permits the avoidance of adjuvant radiother- then exposed to various progestagenic agents, with care- apy in some cases, or identifies those where the ful evaluation of response by curettage at 6 weeks, 3 radiotherapy field can be extended to incorporate months and 6 months from commencement of therapy the para‐aortic region. Evidence of non‐response resulted in immediate debates is the lack of appropriate high‐level evidence surgery and in those with response some pregnancies that lymphadenectomy has a real therapeutic effect on are reported. A hysterectomy was normally performed survival and indeed that extension of the field of radio- following a successful pregnancy. There is an urgent need Radiotherapy to address this issue and ensure patients are been man- aged in a manner whereby the morbidity of the inter- Primary vention can be justified by the improved patient Radiotherapy can be used either as a primary or adjuvant outcome. It is not considered superior to surgical intervention, Debulking in advanced disease with an estimated reduction in 5‐year survival of about When the disease has obvious macroscopic spread 5% when compared with surgery in early‐stage disease, beyond the uterus or indeed the pelvis, then multi- though this is based on retrospective series. Endometrial Cancer 881 Adjuvant Many smaller series have suggested that the com- the use of radiotherapy in an adjuvant setting continues bination of radiotherapy with chemotherapy may to be modified. Original studies indicated that the use of improve outcome, by reducing local pelvic recurrences brachytherapy with external‐beam pelvic radiotherapy and also extra‐pelvic disease relapse. This been proven in chemoradiotherapy as used in cervical original study from the 1980s by Aalders et al. Further analysis suggested that patients with grade 3 tumours infiltrating greater Relapsed endometrial cancer than 50% of the myometrium might benefit from the addition of pelvic radiotherapy. The 5‐year sur- the staging system, though where available positron vival rates were 81 and 85%, respectively. Analysis showed and if the disease is localized and the area radiother- that radiotherapy was not necessary in women with apy‐naive, radiation is the first course of intervention. All had undergone surgery, consisting chemotherapy or hormonal therapies can be used. The conclusions were that the routine and the effect is poorer for disease relapsed within a use of external beam with brachytherapy reduced the field of radiotherapy. The authors also suggested that there selected patients, and may be occasionally justifiable as a may be a possible survival benefit in those with high‐ palliative procedure. Chemotherapy When distant metastatic disease is present, systemic treatments are required. For endometrial cancer, chem- Conclusion otherapeutic agents or hormonal therapies are used. Cisplatin and doxorubicin are the commonest cytotox- Endometrial cancer is a disease increasing in inci- ics used, with medroxyprogesterons the most used hor- dence though retains a relatively good prognosis. Advances in surgi- response rates range from 7 to 69% depending on the cal techniques continue to reduce surgically associated study. As previously stated, the comorbidities within this morbidity, though in a population with rising obesity, patient cohort often means that hormonal therapy is the maintaining morbidity rates is challenging. In some best option due to its ease of administration and lack of early‐stage disease lymphadenectomy is unnecessary, adverse side effects. Randomized trials are redefining the role of adjuvant therapies; in particular the role of chemo- ● Endometrial cancer is now the commonest gynaeco- therapy in high‐risk patients is awaited.