
Christian Brothers University. B. Trano, MD: "Order Risperidone no RX - Cheap Risperidone online no RX".
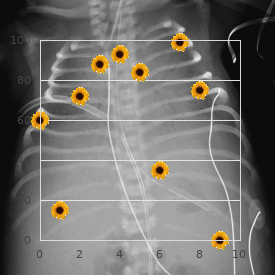
The breast is rotated medially order 2 mg risperidone with mastercard medicine 801, and a the inframammary fold on the anterior surface of the breast buy discount risperidone 3mg on line symptoms 2 months pregnant, as 6–7 cm line is drawn from the inferior portion of the circumfer- shown in Fig buy cheap risperidone 2mg medicine abuse. The nipple can be at a different height accord- ence along the line passing through the central point of the infra- ing to the patient’s characteristics (height, characteristics of the mammary fold as for reaching the breast meridian. The ideal position should be pillars of the breast will represent the portion of scar that F i g. Line A is the superior portion of the new nipple/areola com- to draw the lines of the lateral pillars. Such lines should be the ideal plex, Lines B-D and C-E represent the portion of scar from the inferior continuation of the breast meridian. The neo-areola is drawn by hand or by using a template while the assistant keeps the skin of the breast moderately stretched. The diameter of the neo-areola, as pre- viously mentioned, should not measure more than 4–4. At this point, we can draw the nipple-carrying pedicle that can be superior, superomedial, or superolateral according to the surgeon’s preference. We will describe the superior pedicle technique although goes from the inferior margin of the areola to the central the same procedures can be performed for the other two ped- point of the inframammary fold and should have a 5–7 cm icles (superomedial and superolateral) as well. The angle between these two lines can be increased or reduced according to the size of the areola and to the quantity of tissue to be removed. With following step consists of drawing the pedicle and the por- this last position, the tension on breast tissues is reduced and tion of the areola and nipple to be transposed. Some that undergo a reduction mammoplasty have an enlarged and authors prefer to inject the local anesthetic with epinephrine sometimes asymmetrical areola. During the operation, the before starting the operation in order to reduce the intraop- areola is not entirely transposed but only a part of it with the erative bleeding. In order to improve the final aesthetic ing that can occur at the end of the operation with the risk of outcome, it is therefore preferred to draw around the nipple a postoperative hematoma formation [28 – 30]. In fact, under tension the epithelialization of the nipple-carrying pedicle that is per- de-epithelialization of the pedicle is extremely easy. It is useful to leaving a 1–2 cm ring of tissue around the areola in order to remark that the tissue removal should be slightly bigger on assure an adequate blood supply. The width of the base of the the lateral side and slightly smaller on the medial one in order pedicle should be at least 5–6 cm in order to assure an ade- to maintain an adequate breast volume medially and as a con- quate blood flow and an appropriate venous drainage. In this step, it is very important not to damage the surrounding skin in order to avoid the sufferance of the tissues and an impaired healing with unpleasant cica- tricial outcomes. After incising the pedicle along the borders following a vertical line, we proceed to the sculpting of the flap in its inferior portion (Fig. The thickness of the flap can be reduced when the tissue is particularly dense and does not allow the folding of the pedicle on itself to fix the areola to the point A Fig. At this point, in case it is necessary to reposition tive view of the shape and projection of the breast. Another the breast tissue at a higher position, it is possible to dissect suture is placed to join the cranial portion of the pillars with along the fascia of the pectoralis major muscle up to the sec- the lower pole of the areola. The next suture in a 2/0 resorbable stitch, is placed to Some authors maintain that the tubes reduce the risk of hema- join the base of the pillars with the central point of the infra- toma; however, this has not been demonstrated [31, 32]. In this way, we have a sugges- The drainage tube can come out from: • The axilla • The lateral part of the surgical wound without performing other incisions • The lateral part of the breast along the line of the bra in order to disguise the scar with the underwear The suture of the breast can be performed with single stitches on the subcutis and completed with an intradermal suture in resorbable thread (Figs. In our opinion, the dressing is of utmost importance as it helps modeling the breast and preventing hematomas and seromas during the first stages of healing [16]. The inverted-T design of the final scar is evident (b) Inverted-T Scar Reduction Mammoplasty 205 Fig. The lines must be traced with permanent markers that are not erased during the preparation of the surgical field by alcoholic disinfectants. In case a line is traced in a wrong position, it is advisable to erase it accu- rately in order not to mix up the lines during surgery. The procedure consists of dipping a 22-gauge needle into a container with Pearls and Pitfalls methylene blue and driving it into the skin in cor- The authors maintain that some simple expedients, respondence of: mentioned below, can prevent or at least reduce the – Point A of the keyhole complications, contribute to obtain optimal results, – Point of conjunction of future pillars and prevent possible medicolegal sequelae: – Central point of the inframammary fold In this way we will create a temporary tattoo that • The authors suggest that patients undergo a mam- enables us to easily identify the reference points mography or at least a breast ultrasound before for the anchoring of tissues. Less expert sur- surgery in order to identify possible cancer tissue geons may find it difficult to recognize the key that could change the kind of operation to points and could accidentally create breast perform. This allows to obtain an accept- be compromised by a rough manipulation of the tis- able shape since the very beginning and a stable sues that determines alterations of the vasculariza- result and to avoid possible visible or palpable tion along the skin margins of the removed areas. Also the skin This will reflect on the quality of the scars that suture should be very accurate in order to avoid a could become diastatic and dyschromic. The anesthetist should be adipose and cutaneous tissue in excess in a gradual able to reduce the blood pressure during the initial manner. It is always possible to remove an addi- phases of surgery in order to reduce useless bleed- tional quantity of tissue in a later phase of surgery. In some before the definite closure, possible vessels to coag- cases, it can occur that the plane is erroneously mis- ulate or ligate [33]. If bigger diameters are used, a few the assistant to keep the hypertrophic breast in a months after surgery, the areola will be stretched by Inverted-T Scar Reduction Mammoplasty 207 tissue is distributed in a homogeneous manner in the entire the traction operated by the surrounding tissues, breast. In elderly patients, the breast is usually ptotic, flat- and it appears distorted, excessively big, and with tened, and with an enlarged areola. In these cases, the authors suggest to remove inverted-T scar appears ideal in order to correct this type of additional periareolar tissue in order to immediately alterations in both medium-sized breasts than in gigantomas- obtain a satisfying shape. The most frequent risk, in tia of young and elderly patients; in fact, the transverse com- case these defects are not corrected, is that the distor- ponent of the “T” mammoplasty allows to resect all the tissue tion of the areola becomes permanent. Therefore, we suggest to wake the choice of an inferior pedicle reduction mammoplasty: the patient only after completing the dressing. In teenagers, the hypertrophic • Breasts with a completely depleted upper pole b Fig. Wise pattern (a) preoperative photograph; (b) 2-year postoperative photograph 208 M. Moreover, in smokers, the risk of skin necrosis or contractility liponecrosis is increased. The only difference is the drawing of The disadvantages of the inferior pedicle reduction mam- the pedicle (Figs. The drawing of the pedicle will have as axis the breast merid- • Tendency of the breast to descent downward (“bottoming ian, and it should comprise a portion of tissue of at least 2 cm out”). Such proce- The indications for the inferior pedicle reduction mammo- dure can be eased by the use of a Mammostat or a gauze tight plasty are common to the other reduction mammoplasties at the base of the breast. This expedient allows to distend at and have been previously described in the section relative most the skin of the breast so that it can be easily de- to the superior pedicle reduction mammoplasty with epithelialized with a surgical blade or Mayo scissors. Upon completion of the de-epithelialization, the Mammostat or the gauze is removed and the incision is performed along the drawing previously made (keyhole 10. The sculpting of the pedi- plasty are mainly related to the presence of scars from previ- cle is performed along the borders with a surgical blade or ous surgeries that can interfere with the vascularization of an electrosurgical pencil, according to the surgeon’s the pedicle by interrupting or reducing the blood flow to the preference. Relative contraindications are the transposition of the At this point, the nipple-carrying flap is sculpted along nipple of more than 20–25 cm. In this transpositions over 30 cm; however, in this case the risk of phase, it is very easy to perform an excessive resection of Inverted-T Scar Reduction Mammoplasty 209 b Fig.
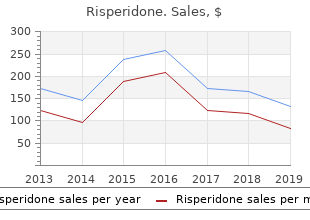
Surveys sent to physicians cheap risperidone 4 mg amex medications online, residents order line risperidone medications dispensed in original container, and medical students in the Northeast buy discount risperidone online symptoms hypoglycemia, Mid-Atlantic, and Midwest of the United States revealed that 97% of responders would disclose a hypothetical error resulting in minor harm and 93% would disclose a hypothetical error resulting in major harm to patients. However, 41% of responders had disclosed an actual error involving minor harm, and only 5% had disclosed an actual medical error involving major harm/death or disability to a patient. These results indicated a discrepancy between the willingness to disclose medical errors and the actual disclosure of errors by physicians. They reported that physicians experienced anxiety about future errors, loss of confidence, difficulties sleeping, and some feared damage to their reputation. Barriers to disclosure include psychological issues such as the fear of retribution from the patient and colleagues; fear that conversations won’t go well; fear of the emotional impact to the patient and self; and beliefs that disclosure is unnecessary, that the unanticipated outcome would have happened anyway, and that the outcome is not directly related to the clinician’s actions. Legal barriers to disclosure include lack of legal protection about the information conveyed, lack of clarity about what needs to be disclosed and when, and belief that disclosing will not be beneficial if case becomes a malpractice claim. However, from the ethical perspective, patients have a right to know about what happened. Disclosure of unanticipated outcomes, adverse events, or near misses is the ethical imperative. Furthermore, Leape stresses the therapeutic aspects of disclosure, stating that full disclosure is essential for healing for the patient, the patient–doctor relationship, and the clinician involved [170]. Surgeons face unique challenges to providing full, appropriate disclosure of surgical adverse events to patients due to the high frequency of such events, current structure of the medicolegal system and variability in legal protections, team structure of surgical care, and lack of clear, reasonable, and specialty-specific standards for guiding disclosure in surgery [171]. Strategies for improvement include training and coaching for disclosure conversations, providing organizational peer support programs and resources for clinicians, improving clinicians’ understanding of the relationship between disclosure and litigation, and establishing organizational programs for communication and resolution, coupled with patient compensation when indicated. Additional strategies offered by Lipira and Gallagher [171] include facilitating collective accountability for individuals and systems in taking responsibility for disclosure conversations, participating in measures to understand why the adverse event happened and how to prevent its recurrence, and establishing standards for disclosure by surgical specialty and subspecialty professional organizations. Much progress has been made over the past two decades toward better understanding the need for transparency with patients about medical errors and adverse events, yet challenges remain in putting policies and procedures into practice [166]. Even countries known for having supported disclosure on a national level are still challenged by (1) putting policy effectively into large-scale practice, (2) managing conflicts between patient expectations and patient safety theory, (3) resolving conflicts between open disclosure and legal privilege and protections, (4) aligning open disclosure with compensation, and (5) effectively measuring the occurrence of disclosure and its quality. Much remains to be done to overcome these challenges and advance the patient safety agenda. Apology is the expression of regret or remorse for the unanticipated outcome, adverse event, or near 158 miss. Apology shows the humanity and fallibility of clinicians, a therapeutic necessity for healing and making amends [170]. Lazare [172] in 2006 stated that an effective apology should (1) acknowledge the offense, (2) explain the commitment of the offense, (3) express remorse, and (4) offer reparation for the offense. Properly conveyed, the apology should touch on all these elements and be relayed with sincerity, preserving the patient’s dignity and providing reassurance that the clinician cares about the patient’s well-being. Cravens and Earp [173] in 2009 highlighted the following “five R’s” and “five A’s” for guiding effective disclosure and apology (see Table 10. Responsibility Take responsibility for what happened and disclose all the details that led to the outcome. Remedy Make clear to the patient what is being done to remedy the situation, including financial costs or compensation if appropriate. Remain Continue to provide care for your patient after the outcome, reassuring them you will remain engaged and engaged available. Five “A’s” of making amends Accurate Truthfully and accurately tell the patient that an error has occurred. Answers Anticipate the patient’s needs for answers about the error and what impact it may have on their clinical situation. Accountable Explain what is known about how the error occurred and accountable about future actions taken to prevent similar errors from occurring. Acknowledge Acknowledge the patient’s responses about the error and its occurrence, addressing their concerns as they arise. A genuine apology can go a long way toward defusing a patient’s anger, showing them respect and empathy, and further facilitate the healing process for all involved. Legislative initiatives that provide legal protection for disclosure and an expression of sympathy or full apology have been drafted or passed, varying in scope and breadth from region to region worldwide [166]. Pelt and Faldmo [174] reported in 2008 that 35 states within the United States had enacted apology statutes and 3 had legislation pending. They regarded such statutes as still in their infancy and unclear as to how well they would stand up in court. Since then, Saitta and Hodge [175] published in 2012 that 34 states and the District of Columbia had enacted laws prohibiting a physician’s apology with disclosure from being admissible evidence in legal proceedings. They highlighted emerging evidence from Michigan [176], Colorado [177], and Kentucky [178] that apologies have reduced the cost of litigation per claim since the implementation of an apology and disclosure program. They emphasized the importance of being aware of the statutes applying to a specific jurisdiction and practice location because the laws of each state have their own nuances. One’s own institutional risk managers can provide guidance and help clarify what to say and when and how best to proceed. Achieving a balance of expert knowledge, technical skills, sound decision-making, and optimal teamwork behaviors offers the best approach toward assuring reliably safe, high-quality care of our surgical patients. As surgeons, we aspire to provide the safest, highest-quality health-care services. The literature reviewed here underscores the importance of a patient safety culture and supports surgical teamwork training and simulation for practicing routine and critical procedures and events, improving technical proficiency 159 and team interactions, and error reduction, recognition, and management. The paradigm of surgical education has indeed shifted from the apprenticeship style of learning. More research is needed to advance our understanding of what environments best facilitate excellence in training and proficiency in technical and teamwork skills, skills that are translatable to the surgical arena. Sound educational objectives serve as the best guide for the ongoing development of simulator technology and the extent of its realism and fidelity. This chapter identified several ways by which to prevent medical errors or mitigate their effects given that all human beings are subject to making errors. A thorough understanding of where surgical practice is vulnerable to error best informs design of systems-based approaches to mitigate the clinical demands that weaken our defenses and facilitate provision of the safest, highest-quality surgical care for our patients. An estimation of the global volume of surgery: A modeling strategy based on available data. Trends in stress urinary incontinence inpatient procedures in the United States, 1979–2004. The role of surgery in global health: Analysis of united states inpatient procedure frequency by condition using the global burden of disease 2010 framework. Incidence of adverse events and negligence in hospitalized patients: Results of the Harvard Medical Practice Study I. Incidence and types of adverse events and negligent care in Utah and Colorado in 1992.
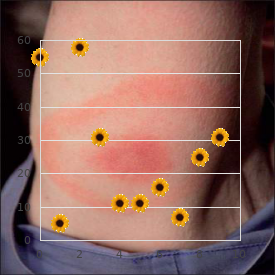
Te term order risperidone 2mg line symptoms right after conception, quadriplegia or tetraplegia buy risperidone cheap online medicine website, Diagnosis implies involvement of all the four limbs order risperidone with a visa symptoms 37 weeks pregnant. Te term, A detailed history and physical examination assist in arriv- monoplegia, refers to involvement of only one limb. A spinal swelling/tenderness, dim- Etiopathogenesis ple, tuft of hair or lipoma over the back should be specially Box 28. Intercostals, rectus abdominalis (both upper and lower), T6 oblique abdominalis Spastic paraplegia; upper abdominals absent Lower half of rectus abdominalis T9, T10 Spastic paraplegia; lower abdominals absent Lower fbers of oblique abdominalis and transversalis T12 L1 iliopsoas Spastic paraplegia; knee jerk lost, ankle jerk present Quadricepts, abductors of hip L3, L4 All movements in lower limbs weak, except fexion of hip, Gluteals, calves, anterior tibials, peroneals, small muscles S1, S2 adduction of thigh, extension of knee and dorsifexion of of foot foot; knee jerk, ankle jerk, plantars absent Anesthesia below folds of groin (including genitalia), Paralysis of lower limbs Whole cauda bladder and rectal control lost; deep refexes absent equina Sensory loss over front, lateral and posterior aspect of Paralysis of gluteal, hamstrings and all muscles below knee Upper sacral L5 thighs, knee jerk and ankle jerk absent Saddle-shaped area of anesthesia, urinary incontinence, No lower limb paralysis Below S2 fecal incontinence; no refex in lower limb afected Anesthesia of anus and rectum Paralysis of levator ani S4, S5 Management 515 Box 28. Paraplegia secondary to a spinal growth too is an indication for a surgical intervention. Acute cerebellar ataxia, usually occurring at 1–5 years of Physiotherapy involves emptying the urinary bladder age, follows a viral infection such as chickenpox, poliovirus by compression or catheterization so that it does not type I, infuenza A and B, echo virus and coxsackie type become distended, atonic, and even spastic with frequent B, or results from an autoimmune response to a variety but only incomplete refex emptying. Te manifestations are noticed from the age of 4–12 Ataxia may be cerebellar or sensory due to involvement of months; always disappear spontaneously by the age of 3–4 posterior column. Inadequate lighting and absence of visual stimuli Incerebellar ataxia, Romberg sign (failure to maintain have been incriminated as the etiologic factors, but standing attitude while standing on tiptoes and knees without sufcient evidence. On the contrary, his (Intellectual Disability) movements become slow, awkward and incomplete. In sensory ataxia due to posterior column lesion, Mental retardation is defned as subaverage intelligence, Romberg sign is positive and there may be other evidence low learning capacity, poor maturation and inadequate of sensory loss. Infections: Encephalitis, meningitis Trauma: Head injury, subdural hematoma Encephalopathy: Whooping cough, toxic. It is customary to designate children with mild mental retardation as educable and moderate mental retardation as trainable. Nevertheless, some degree of education and training is possible even in the severe and profoundly retarded children. A vast majority of them (80–90%) is only mildly retarded; only 5% is with severe to profound impairment. Etiology Mental retardation may be as a result of prenatal, perinatal or postnatal causes (Box 28. Quite a proportion of chil- dren sufering from mental retardation may not ft into any of the known causes mentioned above. Cause is maternal the potential contributory factors), there are at least four rubella. Poor socioeconomic status bromatosis, galactosemia, gargoylism, and Leisch-Nyhan Low birthweight syndrome. Preventable mental retardation embraces Advanced maternal age such causative/contributory conditions as are vulnerable Consanguinity. All these predisposing factors render a subject, pre- Clinical Features natally, or postnatally, vulnerable to the etiologic or con- tributory infuences. Hyperactivity, poor memory, poor attention, poor For children under 5 years, Denver or Gessel develop- concentration, distractibility, emotional instability, mental system may be employed for rough estimate of sleep problems, impulsiveness and awkward (clumsy) the developmental age. Tereafter, mental age may be movements and seizures are usually present in some approximately evaluated as per Box 28. Investigations In certain conditions such as Down syndrome, primary Over and above routine investigations, such special inves- microcephaly, mucopolysaccharidosis, congenital tigations as urine chromatography, urine tests for meta- hypothyroidism, etc. Differential Diagnosis Diagnosis Diferential diagnosis is from the so-called pseudomental Clinical diagnosis is made from the pointers in the retardation which may be secondary to: history and physical examination, including fundoscopy Psychiatric problems like autism and developmental assessment. Te commonly employed methods include: Management Stanford-Binet scale Multidisciplinary approach with a spotlight on special- Wechsler scale ized educational and therapeutic services forms the back- Bhatia-scale bone of management of child with mental retardation. Te family needs not only to be fully informed about Atypical features associated with mental Box 28. Te trend now is to develop z External genitalia: Large testicles, micropenis, ambiguous community-based service system, e. Te goal is to normalize the life of the child and his family rather than to pass the buck by putting the child away as was the practice in the past. Prevention Te crux of all endeavors aimed at preventing mental retardation is promotion of healthy brain, intellectual development and provision of a nurturing and growth- promoting environment. Te following measures may be of special help: Emphasis on the overall welfare of the girl child, the future mother, ensuring that her nutritional status is good and that she is safeguarded against teenage pregnancy as also that she has been adequately vaccinated against rubella. Risk of metabolic disorders of recessive inheritance appearing in homozygous form is high in such unions. Unlike a cretin, he is afectionate, as hyperbilirubinemia, meningitis, congenital friendly, fond of music and has grossly delayed milestones, hypothyroidism, galactosemia and phenylketonuria both physical and mental. Te maximum mental age is must be promptly identifed and managed adequately seldom beyond 8 years. Head is Prevention and management of low birth weight infants microcephalic with fattening of the occiput. Incidence of late-onset (Mongolism) Down syndrome is perhaps the most common among the cataract is high. Trisomy 21 (95% cases) which results from the presence of an extra choromosome 21. In this type the total number remains the normal 46 though one chromosome is large and atypical. Its opposite, “antimongoloid slant” is usually encountered in Apert syndrome, Treacher-Collins syndrome, cerebral gigantism and de Lange syndrome. Newborns with mongolism are more likely to develop distance remains normal (pseudohypertelorism). Likewise, are low-set* and often deformed; ear lobes may be Hirschsprung disease occurs more often in them than in absent or small. Feet show wide gap between the big and second toes Clinical and, at times, a deep crease starting between them and Clinical picture is invariably so characteristic that the extending on the sole (Fig. Te diference between Down Hands are short and broad; little fnger is short and syndrome and congenital hypothyroidism are presented in incurved due to rudimentary middle phalanx. As the child Down syndrome Congenital hypothyroidism grows, hypotonia gradually diminishes. Cheerful Repulsive Tese children are highly susceptible to recurrent Active Lethargic respiratory infections (Box 28. Poor development Microcephaly with fattening of Generally absent of the paranasal sinuses is responsible for recurrent occiput upper airway infection. For Coxa valga details, See Chapter 6 (Developmental, Behavioral and Bony pelvis: Ilia are broad and fared; acetabular and Psychiatric Disorders). Cerebral palsy is a form of chronic motor disability which Predominance of ulnar loops on the digits and radial results from damage to the growing brain before or during loops on 4th and 5th fngers. Te other handicaps that the take care of their person but also to carry occupations patient may have are epilepsy, orthopedic deformities, not requiring much sophistication. Te useful impact of institution- According to conservative estimates, prevalence rate alization for older child is well-recognized.

A slight clockwise torque helps to keep the electrodes in contact with the septum until a His bundle potential is recorded purchase risperidone with visa medications that cause weight loss. It is often advantageous to attempt to record the His bundle potential between several lead pairs during this maneuver (e purchase risperidone mastercard symptoms 3 days dpo. Initially purchase genuine risperidone on line treatment yeast infection child, a large ventricular potential can be observed, and as the catheter is withdrawn, a narrow spike representing a right bundle branch potential may appear just before (less than 30 msec before) the ventricular electrogram. When the catheter is further withdrawn, an atrial potential appears and becomes larger. Where atrial and ventricular potentials are approximately equal in size, a biphasic or triphasic deflection P. The most proximal pair of electrodes displaying the His bundle electrograms should be chosen; it cannot be overemphasized that a large atrial electrogram should accompany the recording of the proximal His bundle potential. The initial portion of the His bundle originates in the membranous atrial septum, and recordings that do not display a prominent atrial electrogram may be recording more distal His bundle or bundle branch potentials and therefore miss important intra-His bundle disease. The use of a standard Bard Electrophysiology Josephson quadripolar multipolar catheter for His bundle recording allows recording of three simultaneous bipolar pairs that can help evaluate intra-His conduction (Fig. Distal and proximal His potentials can often be recorded and intra-His conduction evaluated. A 2-mm decapolar catheter can occasionally be used to record from the proximal His bundle to the right bundle branch. If after several attempts a His bundle electrogram cannot be obtained, the catheter should be withdrawn and reshaped, or it should be exchanged for a catheter with a deflectable tip. Once the catheter is in place, stable recording can usually be obtained for several hours with no further manipulation. Occasionally, continued torque on the catheter shaft is required to obtain a stable recording. This can be accomplished by making a loop in the catheter shaft remaining outside the body, torquing it as necessary, and placing one or two towels on it to hold it; it is rarely necessary for the operator to hold the catheter continuously during the procedure. When the approach just described is used, satisfactory tracing can be obtained in less than 10 minutes in more than 95% of patients. Both the upper extremity approach and the retrograde arterial approach can be used for recording the His bundle electrogram when the femoral vein cannot be used. The quadripolar catheter allows for recording three bipolar signals (distal, mid, and proximal) from which His bundle electrograms can be recorded. The natural course of a catheter passed from the upper extremity generally does not permit the recording of a His P. One technique involves the use of a deflectable catheter with a torque control knob that allows the distal tip to be altered from a straight to a J-shaped configuration once it has been passed to the heart. The tip is then “hooked” across the tricuspid annulus to obtain a His bundle recording. The second technique and its variations are performed with a standard electrode catheter (Fig. The catheter is then gently withdrawn so that the loop opens in the right ventricle with the tip resting in a position to record the His bundle electrogram. Recordings obtained in this fashion are comparable to those obtained by the standard femoral route (Fig. As an alternative to any venous route, the His bundle electrogram may be recorded by a retrograde arterial catheter passed through the noncoronary (posterior) sinus of Valsalva, just above the aortic valve or just below the valve along the intraventricular septum (Fig. Risks and Complications In electrophysiologic studies, even the most sophisticated ones requiring the use of multiple catheters, left ventricular mapping and cardioversion should be associated with a low morbidity. We have performed approximately 12,000 procedures in our electrophysiology laboratories with a single death (a women with acute myocardial infarction, cardiogenic shock, and ventricular tachycardia) and with an overall complication rate of less than 2%. Complications that may arise from the catheterization procedure itself or from the consequences of electrical stimulation are discussed in the following sections. In general, the complication rates are higher in elderly patients and those undergoing catheter ablation than in patients less than 20-years old undergoing diagnostic procedures alone. Complications in diagnostic studies were approximately 1% and in ablation studies were approximately 2. The danger of hemorrhage is greater when the femoral artery is used, particularly in the obese patient. The danger can be minimized by: (a) maintaining firm manual pressure on puncture sites for 10 to 20 minutes after the catheters are withdrawn; (b) having the patient rest in bed with minimal motion of the legs for 12 to 24 hours after the study; (c) having a 5-pound sandbag placed on the affected femoral region for approximately 4 hours after manual compression is discontinued; and (d) careful nursing observation of the patient after the study. Thromboembolism In situ thrombosis at the catheter entry sites or thromboembolism from the catheter is a possibility. We do, as noted previously, however, recommend systemic heparinization for all procedures, particularly those in which a catheter is used in left-sided studies and in right-sided studies of very long duration, especially in a patient with a history of or high risk for thromboembolism. Note that the electrograms obtained from the His bundle catheters placed from the upper and lower extremities are nearly identical. Phlebitis Significant deep vein phlebitis, either sterile or septic, has not been a serious problem in our practice (it has occurred in 0. We do not routinely use antibiotics prophylactically, although in certain selected patients (e. Arrhythmias Arrhythmias induced during electrophysiologic stimulation are common; indeed, induction of spontaneous arrhythmias is often the purpose of the study. A wide variety of reentrant tachycardias may be induced by atrial and/or ventricular stimulation; these often can be terminated by stimulation as well. The risk of ventricular fibrillation can be minimized by stimulating the ventricle at twice the threshold using pulse widths of ≤2 msec. Complications of Left Ventricular Studies Left ventricular studies have additional complications, including strokes, systemic emboli, and protamine reactions during reversal of heparinization. Loss of pulse and arterial fistulas may also occur, but with care and attention, the total complication rate should 18 be less than 1%. No death occurred in their series due to intravascular catheterization, including thromboembolism, local or systemic infections, and pneumothorax. Tamponade Perforation of the ventricle or atrium resulting in tamponade is a possibility and has occurred clinically in <0. All required pericardiocentesis; one required an intraoperative repair of a torn coronary sinus. The right ventricle is more likely to perforate than the left ventricle because it is thinner. Perforation of the atrium or coronary sinus is more likely to occur as the result of ablation procedures in these structures for atrial arrhythmias and bypass tracts (see Chapter 14). Perforation with or without tamponade is more frequent during procedures involving ablation (approximately 0. The safety of electrophysiologic studies has been confirmed in other laboratories and in published reviews of this 17 18 type.