
University of Michigan-Ann Arbor. H. Owen, MD: "Purchase Clozapine online in USA - Proven Clozapine".
Without aggressive intervention cheap clozapine 50mg without a prescription depression facts, the individual may prog- ress to alcohol withdrawal delirium about the second or third day following cessation of buy clozapine 25mg low cost mood disorder clinic, or reduction in order clozapine uk depression test how depressed am i, prolonged, heavy alcohol use. The use of amphetamines is often initiated for their appetite- suppressant effect in an attempt to lose or control weight. Chronic daily (or almost daily) use usually results in an increase in dosage over time to produce the desired effect. Episodic use often takes the form of binges, followed by an intense and unpleasant “crash” in which the individual experiences anxiety, irritability, and feelings of fatigue and depression. Continued use appears to be related to a “craving” for the substance, rather than to prevention or alleviation of with- drawal symptoms. Substance-Related Disorders ● 81 Amphetamine (or Amphetamine-like) Intoxication 1. Amphetamine withdrawal symptoms occur after cessation of (or reduction in) amphetamine (or a related substance) use that has been heavy and prolonged. Symptoms of amphetamine withdrawal develop within a few hours to several days and include fatigue; vivid, unpleasant dreams; insomnia or hypersomnia; increased appetite; and psychomotor retardation or agitation. It is commonly regarded incorrectly to be a substance with- out potential for dependence. Abuse is evidenced by participation in hazardous activities while motor coordination is impaired from cannabis use. Physical symptoms of cannabis intoxication include conjuncti- val injection, increased appetite, dry mouth, and tachycardia. Chronic daily (or almost daily) use usually results in an increase in dosage over time to produce the desired effect. Episodic use often takes the form of binges, followed by an in- tense and unpleasant “crash” in which the individual experiences anxiety, irritability, and feelings of fatigue and depression. Cocaine abuse and dependence lead to tolerance of the substance and subsequent use of increasing doses. Continued use appears to be related to a “craving” for the substance, rather than to prevention or alleviation of with- drawal symptoms. Symptoms of cocaine intoxication develop during, or shortly after, use of cocaine. Symptoms of cocaine intoxication include euphoria or affective blunting, changes in sociability, hypervigilance, interpersonal sensitivity, anxiety, tension, anger, stereo- typed behaviors, impaired judgment, and impaired social or occupational functioning. Physical symptoms of cocaine intoxication include tachycar- dia or bradycardia, pupillary dilation, elevated or lowered blood pressure, perspiration or chills, nausea or vomiting, psychomotor agitation or retardation, muscular weakness, respiratory depression, chest pain, cardiac arrhythmias, con- fusion, seizures, dyskinesias, dystonias, or coma. Symptoms of withdrawal occur after cessation of, or reduc- tion in, cocaine use that has been heavy and prolonged. Symptoms of cocaine withdrawal include dysphoric mood; fatigue; vivid, unpleasant dreams; insomnia or hypersomnia; increased appetite; psychomotor retardation or agitation. The cognitive and perceptual impairment may last for up to 12 hours, so use is generally episodic, because the individual must organize time during the daily schedule for its use. Dependence is rare, and most people are able to resume their previous lifestyle, following a period of hallucinogen use, without much difficulty. These episodes consist of visual or auditory misperceptions usually lasting only a few seconds but sometimes lasting up to several hours. Hallucinogens are highly unpredictable in the effects they may induce each time they are used. Symptoms include marked anxiety or depression, ideas of reference, fear of losing one’s mind, paranoid ideation, and impaired judgment. Other symptoms include subjective intensification of percep- tions, depersonalization, derealization, illusions, hallucina- tions, and synesthesias. Effects are induced by inhaling the vapors of volatile sub- stances through the nose or mouth. Examples of substances include glue, gasoline, paint, paint thinners, various cleaning chemicals, and typewriter correc- tion fluid. Use of inhalants often begins in childhood, and considerable family dysfunction is characteristic. Tolerance has been reported among individuals with heavy use, but a withdrawal syndrome from these substances has not been well documented. Symptoms of intoxication develop during, or shortly after, use of, or exposure to, volatile inhalants. Symptoms of inhalant intoxication include belligerence, assaultiveness, apathy, impaired judgment, and impaired social or occupational functioning. The effects of nicotine are induced through inhaling the smoke of cigarettes, cigars, or pipe tobacco and orally through the use of snuff or chewing tobacco. Nicotine is commonly used to relieve or to avoid withdrawal symptoms that occur when the individual has been in a situ- ation where use is restricted. Continued use despite knowledge of medical problems related to smoking is a particularly important health problem. Symptoms of withdrawal develop within 24 hours after abrupt cessation of (or reduction in) prolonged nicotine use. Symptoms of nicotine withdrawal include dysphoric or depressed mood, insomnia, irritability, frustration, anger, anxiety, difficulty concentrating, restlessness, decreased heart rate, and increased appetite. Various forms are taken orally, intravenously, by nasal inha- lation, and by smoking. Dependence occurs after recreational use of the substance “on the street” or after prescribed use of the substance for relief of pain or cough. Once abuse or dependence is established, substance procure- ment often comes to dominate the person’s life. Cessation or decreased consumption results in a “craving” for the substance and produces a specific syndrome of withdrawal. Symptoms of opioid intoxication include euphoria (initially) followed by apathy, dysphoria, psychomotor agitation or retardation, impaired judgment, and impaired social or occupational functioning. Symptoms of opioid withdrawal occur after cessation of (or reduction in) heavy and prolonged opioid use. Symptoms of withdrawal can also occur after administration of an opioid antagonist after a period of opioid use. Symptoms of opioid withdrawal can occur within minutes to several days following use (or antagonist), and include dysphoric mood, nausea or vomiting, muscle aches, lacrima- tion or rhinorrhea, pupillary dilation, piloerection, sweating, abdominal cramping, diarrhea, yawning, fever, and insomnia. Use can be on a chronic daily basis but more often is taken episodically in binges that can last several days. Dependence can occur following recreational use of the substance “on the street” or after prescribed use of the substance for relief of anxiety or insomnia. Once dependence develops, there is evidence of strong substance-seeking behaviors (obtaining prescriptions from several physicians or resorting to illegal sources to maintain adequate supplies of the substance). Abrupt cessation of these substances can result in life- threatening withdrawal symptoms. Symptoms of intoxication develop during or shortly after intake of sedatives, hypnotics, or anxiolytics. Symptoms of intoxication include inappropriate sexual or aggressive behavior, mood lability, impaired judgment, and impaired social or occupational functioning. Withdrawal symptoms occur after cessation of (or reduc- tion in) heavy and prolonged use of sedatives, hypnotics, or anxiolytics.
Give recognition and positive reinforcement for client’s volun- tary interactions with others safe clozapine 100 mg depression rage. Positive reinforcement enhances self-esteem and encourages repetition of acceptable behaviors order clozapine with american express kidney depression symptoms. When anxiety is high generic 25 mg clozapine visa depression checklist, client may require simple, concrete demonstrations of activities that would be performed without difficulty under normal conditions. Client may be unable to tolerate large amounts of food at mealtimes and may therefore require additional nourishment at other times during the day to receive adequate nutrition. Assist client to bathroom on hourly or bihourly schedule, as need is determined, until he or she is able to fulfill this need without assistance. Client maintains optimal level of personal hygiene by bathing daily and carrying out essential toileting procedures without assistance. They are classified as mental disorders because patho- physiological processes are not demonstrable or understandable by existing laboratory procedures, and there is either evidence or strong presumption that psychological factors are the major cause of the symptoms. It is now well documented that a large proportion of clients in general medical outpatient clinics and private medical offices do not have organic disease requiring medical treatment. It is likely that many of these clients have somatoform disorders, but they do not perceive themselves as having a psychiatric problem and thus do not seek treat- ment from psychiatrists. Symptoms can represent virtu- ally any organ system but commonly are expressed as neuro- logical, gastrointestinal, psychosexual, or cardiopulmonary dis- orders. Onset of the disorder is usually in adolescence or early adulthood and is more common in women than in men. The disorder usually runs a fluctuating course, with periods of re- mission and exacerbation. This diagnosis is made when psychological factors have been judged to have a major role in the onset, severity, ex- acerbation, or maintenance of the pain, even when the physical examination reveals pathology that is associated with the pain. Hypochondriasis Hypochondriasis is an unrealistic preoccupation with the fear of having a serious illness. Occasionally medical disease may be pres- ent, but in the hypochondriacal individual, the symptoms are grossly disproportionate to the degree of pathology. Individu- als with hypochondriasis often have a long history of “doctor shopping” and are convinced that they are not receiving the proper care. Conversion Disorder Conversion disorder is a loss of or change in body function re- sulting from a psychological conflict, the physical symptoms of which cannot be explained by any known medical disorder or pathophysiological mechanism. The most common conversion symptoms are those that suggest neurological disease such as paralysis, aphonia, seizures, coordination disturbance, akinesia, dyskinesia, blindness, tunnel vision, anosmia, anesthesia, and paresthesia. Body Dysmorphic Disorder This disorder, formerly called dysmorphophobia, is charac- terized by the exaggerated belief that the body is deformed or defective in some specific way. Studies have shown an increased incidence of somatization disorder, conversion disorder, and hypo- chondriasis in first-degree relatives, implying a possible inheritable predisposition (Sadock & Sadock, 2007; Soares & Grossman, 2007; Yutzy, 2003). Decreased levels of serotonin and endor- phins may play a role in the etiology of pain disorder. They hypothesize that physical complaints are the expression of low self- esteem and feelings of worthlessness and that the individual believes it is easier to feel something is wrong with the body than to feel something is wrong with the self. The psychodynamic theory of conversion disorder pro- poses that emotions associated with a traumatic event that the individual cannot express because of moral or ethical unacceptability are “converted” into physical symptoms. The unacceptable emotions are repressed and converted to a somatic hysterical symptom that is symbolic in some way of the original emotional trauma. Some families have difficulty expressing emotions openly and resolving conflicts verbally. When this occurs, the child may become ill, and a shift in focus is made from the open conflict to the child’s illness, leaving unre- solved the underlying issues that the family cannot confront openly. Thus, somatization by the child brings some stabil- ity to the family, as harmony replaces discord and the child’s welfare becomes the common concern. Somatic complaints are often reinforced when the sick role relieves the individual from the need to deal with a stressful situation, whether it be within society or within the family. When the sick per- son is allowed to avoid stressful obligations and postpone unwelcome challenges, is excused from troublesome du- ties, or becomes the prominent focus of attention because of the illness, positive reinforcement virtually guarantees repetition of the response. Personal experi- ence, or the experience of close family members, with seri- ous or life-threatening illness can predispose an individual to hypochondriasis. Once an individual has experienced a threat to biological integrity, he or she may develop a fear of recurrence. The fear of recurring illness generates an exaggerated response to minor physical changes, leading to hypochondriacal behaviors. Some cultures and religions carry implicit sanctions against verbalizing or directly expressing emotional states, thereby indirectly encouraging “more acceptable” somatic behaviors. Cross- cultural studies have shown that the somatization symp- toms associated with depression are relatively similar, but the “cognitive” or emotional symptoms such as guilt Somatoform Disorders ● 179 are predominantly seen in Western societies. In Middle Eastern and Asian cultures, depression is almost exclusively manifested by somatic or vegetative symptoms. Environmental influences may be significant in the predisposition to somatization disorder. Some studies have suggested that a tendency toward somatization appears to be more common in individuals who have low socioeconomic, occupational, and educational status. Any physical symptom for which there is no organic basis but for which evidence exists for the implication of psycho- logical factors. Impairment in social or occupational functioning because of preoccupation with physical complaints 10. Psychosexual dysfunction (impotence, dyspareunia [painful coitus], sexual indifference) 11. Excessive preoccupation with physical defect that is out of proportion to the actual condition Common Nursing Diagnoses and Interventions (Interventions are applicable to various health-care settings, such as inpatient and partial hospitalization, community outpatient clinic, home health, and private practice. Possible Etiologies (“related to”) [Severe level of anxiety, repressed] [Low self-esteem] [Unmet dependency needs] [Secondary gains from the sick role] Defining Characteristics (“evidenced by”) Verbal report of pain [in the absence of pathophysiological evidence] Reduced interaction with people Facial mask [of pain] Guarding behavior [Demanding behaviors] [Refuses to attend therapeutic activities because of pain] [History of seeking assistance from numerous health-care professionals] [Excessive use of analgesics, without relief of pain] Self-focusing Goals/Objectives Short-term Goal Within 2 weeks, client will verbalize understanding of correla- tion between pain and psychological problems. Long-term Goal By time of discharge from treatment, client will verbalize a noticeable, if not complete, relief from pain. Monitor physician’s ongoing assessments and laboratory re- ports to ascertain that organic pathology is clearly ruled out. Recognize and accept that the pain is real to the individual, even though no organic cause can be identified. Denying the client’s feelings is nontherapeutic and hinders the develop- ment of a trusting relationship. Identification of the precipitating stressor is important Somatoform Disorders ● 181 for assessment purposes. This information will be used to develop a plan for assisting the client to cope more adaptively. These distractors serve in a therapeutic man- ner as a transition from focus on self or physical manifes- tations to focus on unresolved psychological issues. Help client connect symptoms of pain to times of increased anxiety and to identify specific situa- tions that cause anxiety to rise. Verbalization of feelings in a nonthreatening environment facilitates expression and resolution of disturbing emotional issues.
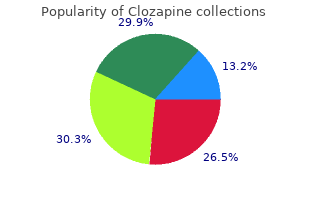
Order clozapine once a day. Bipolar Disorder in Children and Adolescents - Part 5.
The pain is in the centre of the chest and has lasted for 3 h by the time of his arrival in the emergency department buy clozapine without prescription hyperinflationary depression definition. He has been treated with aspirin and with beta-blockers regularly for the last 2 years and has been given a glyceryl trinitrate spray to use as needed discount clozapine online master card depression symptoms essay. His father died of a myocardial infarction aged 66 years and his 65-year-old brother had a coronary artery bypass graft 4 years ago discount 50 mg clozapine otc depression during period. Examination He was sweaty and in pain but had no abnormalities in the cardiovascular or respiratory systems. He was given analgesia and thrombolysis intravenously and his aspirin and beta-blocker were continued. On examination, now his jugular venous pressure is raised to 6 cm above the manubrioster- nal angle. On auscultation of the heart, there is a loud systolic murmur heard all over the praecordium. In the respiratory system, there are late inspiratory crackles at the lung bases and heard up to the mid-zones. The late inspiratory crackles are typical of pulmonary oedema and the chest X-ray confirms this showing hilar flare with some alveo- lar filling, Kerley B lines at the lung bases and blunting of the costophrenic angles with small pleural effusions. The problems likely to occur at this time and produce shortness of breath are a further myocardial infarction, arrhythmias, rupture of the chordae tendinae of the mitral valve, per- foration of the intraventricular septum or even the free wall of the ventricle, and pulmonary emboli. The first four of these could produce pulmonary oedema and a raised jugular venous pressure as in this man. Pulmonary embolism would be compatible with a raised jugular venous pressure but not the findings of pulmonary oedema on examination and X-ray. Acute mitral regurgitation from chordal rupture and ischaemic perforation of the inter- ventricular septum both produce a loud pansystolic murmur. The site of maximum inten- sity of the murmur may differ being apical with chordal rupture and at the lower left sternal edge with ventricular septal defect, but this differentiation may not be possible with a loud murmur. The management of acute ventricular septal defect or chordal rupture would be similar and should involve consultation with the cardiac surgeons. When these lesions produce haemo- dynamic problems, as in this case, surgical repair is needed, either acutely if the problem is very severe, or after stabilization with antifailure treatment or even counterpulsation with an aortic balloon pump. Milder degrees of failure with a pansystolic murmur may occur when there is ischaemia of the papillary muscles of the mitral valve. This is managed with anti- failure treatment, not surgical intervention, and can be differentiated by echocardiography. He has complained of general pains in the muscles and he also has some pains in the joints, particularly the elbows, wrists and knees. Three weeks earlier, he fell and hit his leg and has some local pain related to this. He is a non-smoker who does not drink any alcohol and has not been on any medication. Twelve years ago he had a myocardial infarction and was put on a beta-blocker but he has not had a prescription for this in the last 6 years. Examination He is tender over the muscles around his limb girdles and there is a little tenderness over the elbows, wrists and knees. There are no other abnormalities to find in the cardiovascular, respiratory or alimentary systems. There are some larger areas of bruising on the arms and the legs which he says have not been associated with any trauma. He lives alone on a second-floor flat which may make it difficult for him to get out. He has a petechial rash which could be related to coagulation problems, but the platelet count is normal. It would be important to examine the rash carefully to see if it is distributed around the hair follicles. A number of the features suggest a possible diagnosis of scurvy from vita- min C deficiency. The rash, muscle and joint pains and tenderness, poor wound healing and microcytic anaemia are all features of scurvy. The classic feature of bleeding from the gums would not be present in an edentu- lous patient. Plasma measurements of vitamin C are difficult because of the wide range in normal sub- jects. In this patient, replacement with ascorbic acid orally cleared up the symptoms within 2 weeks. It would be important to look for other nutritional deficiencies in this situation and to make arrangements to ensure that the situation did not recur after his discharge from hospital. A used packet of paracetamol and dihydrocodeine is found in one of his pockets but no illicit drugs and no means of identification. Examination Tendon reflexes are present and equal except the ankle reflexes which are absent. Little history is available, but the tablets in his pocket might suggest that he has a problem with a painful condition. There are a number of possible causes for his unconsciousness including a cere- brovascular problem, deliberate or accidental drug overdose, including alcohol poisoning, metabolic or endocrine disturbance or hypothermia. The slow respiratory rate could be compatible with an opiate excess suppressing ventilation. It would be appropriate to measure the paracetamol level in the blood and it would be worth giving the opiate antagonist naloxone if there remained a likelihood of overdose. Most cerebrovascular problems would be expected to produce some localizing neuro- logical signs on careful examination even in an unconscious patient. He could have hyperosmolar non-ketotic coma detected by a high glucose and evidence of haemoconcentration. Indeed, in this case, repeat of the rectal temperature measurement with a low-reading thermometer showed a tem- perature of 30. No paracetamol was detected in the blood and his alcohol level was low at 11 mg/100 mL. If this is not achieved by covering the patient with blankets, then warmed inspired oxygen, warm intravenous fluids, bladder or peritoneal lavage might be consid- ered. Drugs and physical disturbance should be limited since the myocardium is often irri- table and susceptible to arrhythmias. Her only other symptom is a gradual increase in frequency of bowel movements from once a day in her teens to two to three times daily. She says that the bowel movements can be difficult to flush away on occasions but this is not a consist- ent problem. She thinks that her grandmother, who lived in Ireland, had some bowel problems but she died 3 years ago, aged 68. She is an infant- school teacher and spends a lot of her spare time in keep-fit classes and routines at a local gym. Examination of her abdomen showed no abnormalities and there are no other significant abnormalities to find in any other system.
The purpose of this book is to assist students and staff nurses as they endeavor to provide high-quality nursing care to their psychiatric clients order 100 mg clozapine fast delivery anxiety 1. The following is an example of a nursing his- tory and assessment tool that may be used to gather informa- tion about the client during the assessment phase of the nursing process order genuine clozapine on line bipolar depression lifting. Family configuration (use genograms): Family of origin: Present family: Family dynamics (describe significant relationships between family members): 2 purchase 100 mg clozapine with amex depression of 1929. This might include effects specific to gender, race, appearance, such as genetic physical defects, or any other factor related to genetics that is affecting the client’s adaptation that has not been mentioned elsewhere in this assessment. Environmental factors (family living arrange- ments, type of neighborhood, special working conditions): b. Health beliefs and practices (personal responsibility for health; special self-care practices): Nursing Process: One Step to Professionalism ● 7 c. Precipitating Event Describe the situation or events that precipitated this illness/ hospitalization: V. Anxiety level (circle level, and check the behaviors that apply): Mild Moderate Severe Panic Calm Friendly Passive Alert Perceives environment correctly Cooperative Impaired attention “Jittery” Unable to concentrate Hypervigilant Tremors Rapid speech Withdrawn Confused Disoriented Fearful Hyperventilating Misinterpreting the environment (hallucinations or delusions) Depersonalization Obsessions Compulsions Somatic complaints Excessive hyperactivity Other 2. Mood/affect (circle as many as apply): Happiness Sadness Dejection Despair Elation Euphoria Suspiciousness Apathy (little emotional tone) Anger/hostility 3. Ego defense mechanisms (describe how used by client): Projection Suppression Undoing Displacement Intellectualization Rationalization Denial Repression Nursing Process: One Step to Professionalism ● 9 Isolation Regression Reaction formation Splitting Religiosity Sublimation Compensation 4. Level of self-esteem (circle one): low moderate high Things client likes about self Things client would like to change about self Nurse’s objective assessment of self-esteem: Eye contact General appearance Personal hygiene Participation in group activities and interactions with others 5. Stage and manifestations of grief (circle one): Denial Anger Bargaining Depression Acceptance Describe the client’s behaviors that are associated with this stage of grieving in response to loss or change. Thought processes (circle as many as apply): Clear Logical Easy to follow Relevant Confused Blocking Delusional Rapid flow of thoughts Slowness in thought association Suspicious Recent memory: Loss Intact Remote memory: Loss Intact Other: 7. Interaction patterns (describe client’s pattern of interpersonal interactions with staff and peers on the unit, e. Reality orientation (check those that apply): Oriented to: Time Person Place Situation 10. Psychosomatic manifestations (describe any somatic complaints that may be stress-related): 2. Skin: Warm Dry Moist Cool Clammy Pink Cyanotic Poor turgor Edematous Evidence of: Rash Bruising Needle tracks Hirsutism Loss of hair Other c. Musculoskeletal status: Weakness Tremors Degree of range of motion (describe limitations) Pain (describe) Skeletal deformities (describe) Coordination (describe limitations) d. Neurological status: History of (check all that apply): Seizures (describe method of control) Headaches (describe location and frequency) Fainting spells Dizziness Tingling/numbness (describe location) e. Cardiovascular: B/P Pulse History of (check all that apply): Hypertension Palpitations Heart murmur Chest pain Shortness of breath Pain in legs Phlebitis Ankle/leg edema Numbness/tingling in extremities Varicose veins f. Method of birth control used Females: Date of last menstrual cycle Length of cycle Problems associated with menstruation? Medication side effects: What symptoms is the client experiencing that may be attributed to current medication usage? Activity/rest patterns: Exercise (amount, type, frequency) Leisure time activities: Patterns of sleep: Number of hours per night Use of sleep aids? Personal hygiene/activities of daily living: Patterns of self-care: Independent Requires assistance with: Mobility Hygiene Toileting Feeding Dressing Other Statement describing personal hygiene and general appearance n. Essential fea- tures of many disorders are identical, regardless of the age of the individual. Examples include the following: Cognitive disorders Personality disorders Schizophrenia Substance-related disorders Schizophreniform disorder Mood disorders Adjustment disorder Somatoform disorders Sexual disorders Psychological factors affect- ing medical condition There are, however, several disorders that appear during the early developmental years and are identified according to the child’s ability or inability to perform age-appropriate tasks or intellectual functions. It 14 Disorders Usually First Diagnosed in Infancy, Childhood, or Adolescence ● 15 is essential that the nurse working with these clients understand normal behavior patterns characteristic of the infant, childhood, and adolescent years. About 5% of cases of mental retardation are caused by hereditary factors, such as Tay-Sachs disease, phenylke- tonuria, and hyperglycinemia. Chromosomal disorders, such as Down syndrome and Klinefelter syndrome, have also been implicated. Mental retardation can occur as an outcome of childhood illnesses, such as encephalitis or meningitis, or be the result of poisoning or physical trauma in childhood. The individual may experience some limitation in speech communication and in interactions with others. Systematic habit training may be accomplished, but the individual does not have the ability for academic or vocational training. There is a lack of ability for speech develop- ment, socialization skills, or fine or gross motor movements. Common Nursing Diagnoses and Interventions for the Client with Mental Retardation (Interventions are applicable to various health care settings, such as inpatient and partial hospitalization, community outpatient clinic, home health, and private practice. Remove small items from the area where client will be ambulating and move sharp items out of his or her reach. Prevent physical aggression and acting out behaviors by learning to recognize signs that client is becoming agitated. Because clients’ capabilities vary so widely, it is important to know each client individually and to ensure that no client is set up to fail. Positive reinforcement enhances self-esteem and encourages repetition of desirable behaviors. When one aspect of self-care has been mastered to the best of client’s ability, move on to another. If client cannot speak or communicate by other means, needs are met by caregiver’s anticipation of client’s needs. This facilitates trust and the ability to understand client’s ac- tions and communication. Anticipate and fulfill client’s needs until satisfactory com- munication patterns are established. Learn (from family, if possible) special words client uses that are different from the norm. Identify nonverbal gestures or signals that client may use to convey needs if verbal communication is absent. Some children with mental retardation, particularly at the severe level, can only learn by systematic habit training. Disorders Usually First Diagnosed in Infancy, Childhood, or Adolescence ● 19 Outcome Criteria 1. Long-term Goal Client will be able to interact with others using behaviors that are socially acceptable and appropriate to developmental level. Explain to other clients the meaning of some of client’s nonverbal gestures and signals. Others may be more accepting of client’s differentness if they have a better understanding of his or her behavior. Use simple language to explain to client which behaviors are acceptable and which are not. Establish a procedure for behavior modification that offers rewards for appropriate be- haviors and renders an aversive reinforcement in response to the use of inappropriate behaviors. Positive, negative, and aversive reinforcements can contribute to desired changes in behavior.