
Louisiana State University at Shreveport. Q. Achmed, MD: "Buy online Sildalis no RX - Proven Sildalis".
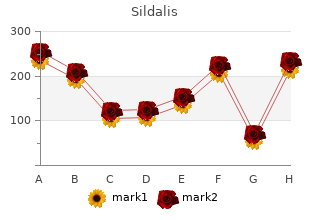
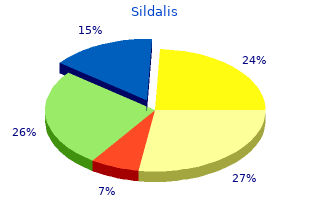
So the hernia stops at the top of the testis and is known as a congenital funicular hernia buy sildalis us erectile dysfunction japan. It must be remembered that congenital hernia buy 120mg sildalis amex erectile dysfunction premature ejaculation treatment, though so named generic sildalis 120mg fast delivery erectile dysfunction doctor tampa, is usually seen in adults. Clinically it can be differentiated from a congenital hernia by the fact that it does not become complete at once. It is frequently incomplete, but it may descend into the scrotum if remains untreated for years. The hernia comes out as soon as the patient stands and disappears immediately when he lies down. In case of invagination test the finger goes directly backwards instead of upwards, backwards and laterally (in case of indirect hernia). When the patient is asked to cough after occluding the deep inguinal ring the hernia comes out medial to the occluding finger. Direct hernia does not come out through the deep inguinal ring but a little medial to the ring. Enterocele is elastic in consistency, resonant on percussion and slips back into the abdomen with a distinct gurgle. It is suspected when the patient gives the history that the hernia gets enlarged just before micturition and smaller after micturition. Pressure on the hernia induces a desire for micturition particularly when it is distended. That means its contents can be returned into the abdominal cavity, but the sac remains in its position. Various causes of irreducibility are :— (i) adhesion of its contents to each other, (ii) adhesion of its contents with the sac, (iii) adhesion of one part of the sac to the other part, (iv) sliding hernia and (v) very large scrotal hernia (scrotal abdomen). Clinically a strangulated hernia is also irreducible, but it is extremely tender and tense and the overlying skin may be red. It must be remembered that there is no interference with the blood supply to the intestine in this hernia. One must be very careful to make this diagnosis, as strangulated hernia also possesses two of its features i. Of course the third and most important feature of a strangulated hernia is missing in this hernia i. Strangulated hernia (irreducibility+obstruction+arrest of blood supply to the contents). Diagnosis of strangulation is made when a hernia is irreducible, without any impulse on coughing, extremely tense and tender. Diagnosis is made by the presence of constitutional disturbances associated with local signs of inflammation — overlying skin becomes red and oedematous and the swelling becomes painful, tender and swollen. The only differentiating feature from a strangulated hernia is that this hernia is not tense and is not associated with intestinal obstruction. A large globular hernia when descends well into the scrotum this condition is suspected. This condition may be associated with strangulated small intestine within its sac or a strangulated large intestine outside the sac. The loop in the circumference of the bowel becomes The thick line represents abdomen is always found strangulated. This condition often the peritoneum, Note that at a more advanced stage complicates a femoral hernia and the colon forms the wall of strangulation than the rarely an obturator hernia. The patient may or may not vomit, intestinal colic is present but the bowels are opened normally. The loop within the abdomen becomes first strangulated and can only be suspected when tenderness is elicited above the inguinal ligament along with presence of intestinal obstruction. The hernia actually comes out superficially through the saphenous opening situated Wi inches below and lateral to the pubic tubercle. When the hernia is within the femoral canal it remains narrow, but once it escapes through the saphenous opening into the loose areolar tissues, it expands considerably. Femoral Femoral Nerve Femoral Artery Femoral Vein hernia is commoner in FttiMraiRing women (2 : 1). But the Lacunar ligament students must remember that even in women the Superficial commonest hernia in the Inguinal Ring groin is the inguinal! The right side is affected twice as common as the left side and in 20 per cent of cases the condition is bilateral. One thing must be borne in mind that the femoral canal being a rigid opening this hernia becomes strangulated very often. Similarly a Inferior Epigastric Vessels Femoral Nerve femoral hernia can be prevented from coming out by Femoral Ring through which Femoral pressure applied over the Hernia Comes out femoral canal or the saphenous Obturator Nerve External Iliac Vessels opening. The so called impulse on coughing is present in this condition as well, but it is actually a fluid thrill and not an expansile impulse to the examining fingers. The track of the psoas abscess from the caries spine upwards to the saphena varix felt by the fingers is shown in the figure. Sometimes that femoral hernia lies on the medial side of a venous hum can be heard when the the femoral vessels. The gland of Cloquet lying within the femoral canal may be enlarged and simulates exactly an irreducible femoral hernia. If any focus cannot be Pectineus Muscle found out or any cause of Superior Ramus of Pubis enlargement of lymph nodes cannot be detected, the Fig. It is a painless swelling and if the pulsation of the femoral artery can be palpated it will be appreciated that the swelling is lateral to the artery. Sometimes there is an iliac part of the abscess which is determined by cross-fluctuation. Examinations of the back and corresponding iliac fossa including X-rays clarify the diagnosis. Presence of osteoarthritis in the hip joint, a cystic swelling, absence of impulse on coughing and that the swelling diminishes in size during flexion of the hip joint are the diagnostic points in favour of this condition. The neck of the hernia is generally wide and hardly gives rise to intestinal obstruction or strangulation. The main diagnostic features are — (i) Bulge through the centre of the umbilical scar everting the whole umbilicus; (ii) Age of the patient; (iii) The swelling is easily reducible (spontaneously reduced when the child lies down) and there is definite impulse on crying; (iv) The size of the hernia varies — it may be a small defect admitting the tip of the little finger alone to quite a large opening admitting two or three fingers; (v) The content is usually small intestine, so resonant to percussion; (vi) About 90% of these herniae disappear spontaneously during the first 5 years of life as the umbilical scar thickens and contracts. It is very rare in comparison to the para-umbilical hernia which is described below. Almost invariably it is due to raised intra-abdominal pressure which has forced the hernia through the umbilical scar. One must try to find out the cause of raised intra-abdominal pressure in these cases. Common causes are — pregnancy, ascites, bowel distension, ovarian cyst and fibroid. The usual site is just above the umbilicus between the two recti, in fact lower half of the fundus of the sac is covered by the umbilicus. The diagnostic features are as follows : (i) Para-umbilical hernia develops in the middle and old age; (ii) Obese women are more commonly affected; (iii) Usual symptoms are pain and swelling. If the swelling is very small, it may not be noticed by the patient and the pain and discomfort become the main symptoms; (iv) The surface is smooth and the edge is distinct except when the patient is very fat; (v) It contains omentum or bowel.
Voiding cystourethrogram is the diagnostic test purchase 120 mg sildalis with visa erectile dysfunction dr mercola, and endoscopic fulguration or resection will get rid of them cheap sildalis 120 mg online erectile dysfunction doctor specialty. The urethral opening is on the ventral side of the penis best 120mg sildalis osbon erectile dysfunction pump, somewhere between the tip and the base of the shaft. Circumcision should never be done on such a child, inasmuch as the skin of the prepuce will be needed for the plastic reconstruction that will eventually be done. Vesicoureteral reflux and infection produce burning on urination, frequency, low abdominal and perineal pain, flank pain, and fever and chills in a child. The patient feels normally the need to void, and voids normally at appropriate intervals (urine deposited into the bladder by the normal ureter); but is also wet with urine all the time (urine that drips into the vagina from the low implanted ureter). Thus the classic presentation is an adolescent who goes on a beer- drinking binge for the first time in his life and develops colicky flank pain. Most cases of hematuria are caused by benign disease, but any patient presenting with this condition should get a work-up to rule out cancer (the one exception is the adult who has a trace of urine after significant trauma who needs a work-up but not to identify cancer). Renal cell carcinoma in its full-blown picture produces hematuria, flank pain, and a flank mass. That full-blown picture is rarely seen today, since most patients are worked up as soon as they have hematuria. Surgery is the only effective therapy and may include partial nephrectomy, radical nephrectomy, or even inferior vena cava resection. Cancer of the bladder (transitional cell cancer in most cases) has a very close correlation with smoking (even more so than cancer of the lung), and usually presents with hematuria. Surveillance frequently stops at age 75, beyond which survival is not affected by treatment. Widespread bone metastases respond for a few years to androgen ablation, surgical (orchiectomy) or medical (luteinizing hormone-releasing hormone agonists or antiandrogens like flutamide). Testicular cancer affects young men, in whom it presents as a painless testicular mass. Because benign testicular tumors are virtually nonexistent, biopsy is not done, and a radical orchiectomy is performed by the inguinal route. Most testicular cancers are exquisitely radiosensitive and chemosensitive (platinum-based chemotherapy), offering many options for successful treatment even in cases of clinically advanced, metastatic disease. It is often precipitated during a cold, by the use of antihistamines and nasal drops, and abundant fluid intake. The patient wants to void but cannot, and the markedly distended bladder is palpable. An indwelling bladder catheter needs to be placed and left in for at least 3 days. Postoperative urinary retention is also very common, and sometimes it masquerades as incontinence. The patient may not feel the need to void because of post-op pain, medications, etc. A huge distended bladder will be palpable, confirming that the problem is overflow incontinence from retention. Stress incontinence is also very common in middle-aged women who have had many pregnancies and vaginal deliveries. They leak small amounts of urine whenever intra-abdominal pressure suddenly increases. This includes sneezing, laughing, getting out of a chair, or lifting a heavy object. Examination will show a weak pelvic floor, with the prolapsed bladder neck outside of the “high-pressure” abdominal area. For advanced cases with large cystoceles, surgical repair of the pelvic floor is indicated. Although there are a variety of endoscopic and other modalities to address retained urinary stones, intervention is not always needed. Small stones (≤3 mm) at the ureterovesical junction have a 70% chance of passing spontaneously. Such cases can be handled with analgesics, plenty of fluids, and watchful waiting. Other options include basket extraction, sonic probes, laser beams, and open surgery. Although there is specific therapy for the prevention of recurrences in defined types of stones, abundant water intake is universally applicable. Psychogenic impotence has sudden onset, is partner- or situation-specific, and usually does not interfere with nocturnal erections (which can be tested with a roll of postage stamps). Psycho- or behavioral therapy may be beneficial, or the condition may be self-limited. Organic impotence, if caused by trauma, will also have sudden onset, specifically related to the traumatic event (after pelvic surgery, because of nerve damage, or after trauma to the perineum, which involves arterial disruption). Because of chronic disease (arteriosclerosis, diabetes), organic impotence has very gradual onset, going from erections not lasting long enough, to being of poor quality, to not happening at all (including absence of nocturnal erections). Sildenafil, tadalafil, and vardenafil have become first choice therapy in many cases but there are many other options, including vascular surgery (well-suited for those with arterial injury), suction devices (can be used on almost everybody), and prosthetic implants. Even donors with metastatic cancer can donate corneas, because the cornea does not have a blood supply. After an organ has been transplanted, rejection can develop despite immunosuppressive medications. Tissue typing and a close tissue match may minimize that risk, but it is an ever-present concern for most patients. Transplant rejection can happen in 3 ways: hyperacute, acute, and chronic rejection. Hyperacute rejection is a vascular thrombosis that occurs within minutes of reestablishing blood supply to the organ. Acute rejection (most common) occurs after the first 5 days, and usually within the first 3 months. In the case of the liver, technical problems are more commonly encountered than immunologic rejection. In the case of the heart, signs of functional deterioration occur too late to allow effective therapy, thus routine ventricular biopsies (by way of the jugular, superior vena cava, and right atrium) are done at set intervals. Chronic rejection is seen years after the transplant, with gradual, insidious loss of organ function. Although we have no treatment for it, patients suspected of having it have the transplant biopsied in the hope that it may be a delayed (and treatable) case of acute rejection. Orotracheal intubation with rapid-sequence anesthetic induction and pulse oximetry (or topical anesthesia) is preferred in the setting of a trauma center. The patient with subcutaneous emphysema requires fiberoptic bronchoscopy (more details follow). A patient involved in a severe car accident has multiple injuries and is unconscious. Altered mental status is the most common indication for intubation in the trauma patient. Unconscious patients with Glasgow coma scale ≤8 may not be able to maintain or protect their airway.
Higher power and greater compression Following the curve of the needle requires a different set produce a cutting effect buy sildalis 120 mg free shipping erectile dysfunction treatment san diego. The cutting speed is inversely of motions than the simple supination used during open proportional to the effectiveness of hemostasis 120mg sildalis for sale erectile dysfunction medication levitra. Watch the needle pass through the tissue and instrument greatly facilitates advanced procedures such adjust your hand motions to pass it in a smooth order sildalis uk erectile dysfunction pills online, atrau- as Nissen fundoplication where sizable vessels (the short matic fashion. Laparoscopic Suturing Intracorporeal knots are placed and tied by the familiar “instrument-tying” method used during open surgery. The Laparoscopic procedures that require suturing are con- sequence of movements to create the first throw of a square sidered advanced procedures; yet, the ability to place one knot is shown in Fig. The second throw is shown in or two sutures may enable the laparoscopic surgeon to Fig. New York: Springer-Verlag, 1999, with permission) Using a Pretied Suture Ligature absorbs water, rendering the knot even more secure. Pretied ligatures are best used to secure the stump of a structure that Pretied endoscopic suture ligatures are available and useful has already been divided or to ligate the base of an appendix. They are commonly loaded with continuity because you must be able to pass the loop over the chromic catgut because this material swells slightly as it structure to be ligated. As the loop comes into contact with tissue, it absorbs water and softens, becoming limp and therefore much more difficult to handle. Avoid this problem by keeping the loop away from tissue until you are ready to close it. Pass a grasper through another port and pass it through the loop of the pretied ligature (Fig. The loop is quite large, and drawing up on the tail to make the loop slightly smaller may facilitate this maneuver. Once the stump is surrounded, place the tip of the knot pusher against the base exactly where you want the knot to sit. Slowly tighten the loop while maintaining slight tension on the stump with the grasper (Fig. Withdraw the knot pusher through the trocar and pass endoscopic scissors down to cut the ligature. Scott-Conner Laparoscopic Stapling Avoiding Complications Laparoscopic stapling may be performed intra- or extracor- Although each procedure has its unique complications, there poreally with the same staplers used during open surgery. Purely intracorporeal stapling is possible using an endo- They are briefly considered here. This stapler may be used to secure the base of an appen- hyperventilation and vigilance on the part of the anesthesi- dix; then, loaded with smaller staples, it may be fired across ologist. It fires two triple rows of staples and cuts logic stress of pneumoperitoneum, and conversion to open between them. Special suture passers are avail- Bleeding from the abdominal wall is a common, annoying able to facilitate passing a suture through the skin incision at complication of trocar site placement. Blood may run down the trocar site and thence through all the layers of the abdom- the instruments or laparoscope to obscure the view during inal wall and back out under direct vision. The suture is then surgery or cause hematoma or hemoperitoneum after surgery tied at the level of the fascia to close the trocar site securely. Avoid this situation by making the lower abdom- These sutures are especially useful in obese patients. Many hours of frustration can be avoided if laparoscopic sur- Generally such bleeding can be controlled by sutures through geons take the time to become thoroughly familiar with the the abdominal wall. Visceral or vascular injury during Veress needle or trocar Adopt a standardized terminology for all the individual placement is avoided by following the guidelines for Veress instruments you use so it is easy for the scrub person to pass needle placement outlined in the previous sections. This may tamponade any bleeding and greatly facilitates finding the site of injury. Loss of Working Space Further Reading If visualization is difficult and the working space seems to be collapsing, feel the abdominal wall and check the pressure Cuschieri A, Szabo Z. In: Laparoscopic flat and the insufflator pressure readings are normal or high, surgery. Complications of endoscopic and laparoscopic surgery: pre- Instruct the anesthesiologist to correct the situation. This is a completely passive drain, and fluid exits around the drain by capillary Drains permit purulent material, blood, serum, lymph, bile, action and gravity. Ideally, the drain is placed to create a pancreatic juice, and intestinal contents to escape from the dependent tract through which fluid escape may be aided by body. If the surgeon does not take pains to bring the drain source of infection or fluid buildup to the outside. This pas- out in a straight line, without wrinkles, stagnant pools of sageway, or tract, must persist for a period long enough to serum accumulate around the wrinkled areas of the drain. More fundamen- In the presence of a discrete abscess, the need for and tally, the passive latex drain does not empty a cavity; it sim- purpose of a drain is obvious and not controversial, as its ply permits secretions to overflow from the abdomen to the therapeutic benefits are clear. It is not particularly effective in evacuating oozing drain acts as a prophylactic instrument to prevent accumula- blood before a clot forms. Because it is a foreign body, the depth of the wound can be irrigated with this type of drain as drain also has the paradoxical effect of potentiating infec- there is when a tube or sump type is used. When and how a drain should be used for prophylactic Finally, the most important objection to the latex drain purposes has long been a source of controversy. Controlled arises from the fact that it requires a 1- to 2-cm stab wound trials have significantly decreased the indications for “pro- in the abdominal wall, which permits retrograde passage of phylactic” drainage; some are cited in the references at the pathogenic bacteria down into the drain tract. Penrose drains are also used for retraction, for example, Various Drains and Their Pros and Cons when the esophagus is retracted during hiatal hernia repair. Latex (Penrose) Drain Polyethylene or Rubber Tube Drain The Penrose drain is a soft latex drain of various dimensions. It has the shape of a flattened cylinder and is made of a thin, These are also passive drains, but are tubular and more rigid radiopaque sheet of rubber. It is also successful in encouraging fibrosis, so drains establish tracts to the outside, as they are mildly irri- it forms a well-established tract within 8–10 days. Patient mobility is unimpaired, as the able for placement deep in the abdominal cavity for a period plastic container is easily attached to the patient’s attire. The of more than a few days, as there is considerable danger of depths of the wound can be irrigated with an antibiotic solu- erosion through an adjacent segment of intestine, resulting in tion by disconnecting the catheter from the suction device an intestinal fistula. These drains are, therefore, primarily and instilling the medication with a sterile syringe. In time, tissues are sucked into the fenestrations, and tissue Silicone or Silastic tubes are less reactive than are other ingrowth may even occur. They are less prone to become plugged as a (occasionally to the point of requiring relaparotomy), and result of clotting serum. Because of the soft texture of sili- most surgeons are reluctant to leave a fenestrated closed suc- cone, erosion into the intestine is uncommon. Fluted A disadvantage of silicone drains is their lack of reactiv- (channel-type) suction drains are also available and avoid ity; hence, there is minimal fibrous tract formation. When a gauze pack is inserted into an abscess cavity and is brought to the outside, the gauze, in effect, serves as a drain.
A major disad- or eliminate the to-and-fro motion that encourages bacteria to vantage of sump drains is the requirement that the patient be migrate down the drain tract sildalis 120 mg free shipping erectile dysfunction statistics race. On the other hand order sildalis in india impotence ginseng, when a latex attached permanently to a suction device order cheap sildalis erectile dysfunction vacuum pump india, thereby impairing drain is brought out through a 1- to 2-cm stab wound in the mobility. These drains are predominately used for very diffi- abdominal wall, there is no possibility of eliminating the to- cult abscesses, such as those associated with peripancreatic and-fro motion of the drain or retrograde passage of bacteria sepsis, where other drains tend to stop working. Consequently, when latex or gauze drains are required for an established abscess, the surgeon must accept the added risk of retrograde contamination with Closed Suction Drain bacteria despite sterile technique when dressings are changed. The closed suction drain consists of one or two multiperfo- Management of Intraperitoneal Sepsis rated silicone or polyethylene catheters attached to a sterile plastic container, the source of continuous suction. It is a When managing intraperitoneal sepsis, a distinction must be closed system; and the catheters are brought out through made between an isolated abscess (e. These drains have replaced other drains dix) and multiple abscesses involving the intestines 10 Rational Use of Drains 71 accompanied by generalized peritonitis. With the latter type Blood and Serum of sepsis, the presence of fibrin and necrotic tissue prevents adequate phagocytosis and perpetuates sepsis. The presence of blood, serum, or fibrin in a perfectly sterile When an abscess has developed rigid walls that do not area is not dangerous to the patient, although the operative collapse after evacuation of pus , large drains must be field is never completely sterile following any major opera- inserted to establish a reliable tract to the outside. For this reason, postoperative puddles of blood or serum Sometimes a rigid abscess cavity requires 2–5 weeks to in combination with even a small number of bacteria can fill with granulation tissue. It is not safe to remove the result in abscess formation because the red blood cell impairs drains until injecting the abscess with an aqueous iodin- antibacterial defenses. With the low colorectal anastomosis, ated contrast medium has produced a radiograph demon- accumulated serum or blood in the presacral space, together strating that the cavity is no longer significantly larger in with secondary infection and abscess formation, may result diameter than the drainage tract. For rigid-walled abscesses of efforts should be exerted to eliminate bleeding during any this type, several large latex drains should be inserted abdominal operation. Some surgeons by some type of drainage, the ideal method is to insert one or place an additional straight 10F catheter for intermittent two multiperforated Silastic drains, which are brought out instillation of dilute antibiotic solution. At least one drain through puncture wounds in the abdominal wall and attached is left in place until the sinogram shows that the abscess to a closed suction system. Care should be taken Closed suction drainage is extremely effective following that none of the rigid drains comes into contact with the radical mastectomy or regional lymph node dissections of intestine or stomach, as intestinal fistulas can be a serious the neck, axilla, or groin. This technique has also been employed successfully following abdominoperineal proctectomy with primary clo- sure of the perineal floor and skin. Percutaneous Drainage of Abdominal Abscesses with Computed Tomography or Ultrasound Guidance Bile Treatment of abdominal abscesses underwent a revolution- Because bile has an extremely low surface tension, it tends to ary change during the 1990s owing to the demonstrated effi- leak through tiny defects in anastomoses or through needle cacy of percutaneous drainage by the interventional holes. A sump drain or closed suction system skilled radiologist can find a safe route along which to insert works well for this purpose. Silastic tubes are contraindi- a drainage catheter that evacuates the pus without a need to cated whenever formation of a fibrous tract to the outside for perform laparotomy for drainage. This technology is espe- the bile is desirable, especially with use of a T-tube in the cially welcome in the critically ill patient who may not toler- common bile duct, as previously noted. Pancreatic Secretions Other Indications and Methods of Drainage It is not dangerous for pure pancreatic juice to drain into the Abscess abdominal cavity, as is evident in patients who have pancre- atic ascites or a fistula. If the pancreatic secretion is activated For abscesses of the extremities, trunk, or perirectal area, by the presence of bile, duodenal contents, or pus, however, the important step is to unroof the abscess by making a cru- trypsinogen is converted to trypsin and the adjacent tissues ciate incision so the tract does not close before all the pus are subjected to a raging inflammatory reaction. An unroofing procedure is adequate constructed adjacent anastomoses may be digested and for superficial abscesses, and any type of temporary drain destroyed. The packing atic secretions completely, especially after pancreaticoduo- is then changed often enough to keep it from blocking the denectomy. Chassin catheter is brought through the segment of jejunum to which from drainage. Unless the tube If complete hemostasis cannot be achieved in the vicinity is accidentally displaced, it conveys all pancreatic secretions of an anastomosis, there may be some merit to inserting a from the abdominal cavity. In addition, a suction catheter is silicone closed suction drain for a few days to prevent pool- inserted in the vicinity of the anastomosis, between the tail of ing of blood next to the anastomosis, provided the drain does the pancreas and the jejunum. Adverse reac- nal anastomosis simply because the surgeon has some doubt tions following T-tube removal. Risk-benefit assessment of closed intra-abdominal presence of a drain may not prevent generalized peritonitis. Langenbecks failure, the anastomosis should be taken apart and done over, Arch Surg. A prospective, con- trap of fuzzy thinking, which would permit acceptance of an trolled study of prophylactic drainage after colonic anastomoses. Practical experience of a no abdominal drainage policy in patients undergoing liver resection. The uses and abuses cellulitis, some surgeons believe the inflamed areas should of drains in abdominal surgery. This chapter provides an illustrated glossary of com- mon instruments and their names. Use this as a general guide and then learn the terms used in your own institutions. Instruments used during open surgery are shown first, followed by instruments used during laparoscopic surgery. The important characteristics are the length, the delicacy of the tips, curved versus straight (curved is more versatile), and whether the serrations extend all the way down to the hinge of the clamp Fig. This is a port designed to allow the surgeon to perform laparoscopic procedure through a single incision. It gives the surgeon the ability to use multiple instruments with maximal maneu- verability through adjustable cannulas all within a low-profile mallea- ble port Fig. This device seals vessels by a combination of pressure and monopolar elec- trocautery. It is also crucial to know if the This cannot be more true than in healthcare—no surgical surgeon was able to place the aortic clamp in the usual intervention can be considered completed until the operative infrarenal position or whether suprarenal clamping was note is done. The operative note is an essential part of the necessary to allow for the construction of the proximal patient’s medical care and records. Such details are essential for the proper standard of care in all hospitals accredited by The Joint planning and selection of the most appropriate treatment Commission or other international hospital accreditation option in the typically challenging reoperative situation. Most hospitals delineate in their bylaws or Trying to tackle this problem without knowing such details policies and procedure manuals their expectations for prompt can further complicate the management of such patient and accurate documentation of operative procedures. Not ful- Similarly consider a patient with Crohn’s disease requir- filling such documentation represents a deviation from the ing a second or third operation to manage yet another com- standards of care. It is very important to provided to the patient and reflects the quality of care deliv- know what was done or resected in the prior procedures and ered. Its value may not be immediately apparent, particularly the length of the remaining small bowel to select the most to the harried surgical resident.