
Huntingdon College. U. Ballock, MD: "Purchase cheap Metformin - Safe Metformin online".
There are many different varieties best metformin 500 mg diabetic vegetarian, but currently buy discount metformin 500 mg diabetes control questionnaire, the best is mesh-mediated traction system cheap metformin 500mg otc diabetes diet to gain weight, com- bined with negative pressure dressings. Using other such systems, including the Barker dressing, will increase the patient’s mor- tality [17]. Particular attention to sterility is even more important when patients have an aortic graft or retroperitoneal necrosis. At the index operation for the open abdomen, the closure plan should be 24 hours for post-ischemia resection, 48 hours post-trauma packing, and 7 days for pancreatitis. At re-exploration the abdomen needs to be washed out carefully with sequential tightening of the mesh to reduce lateralization, the enemy of fnal closure. Miller in a large series identifed that if the abdomen was not closed within 7 days, the complication rate increased dramatically [18]. There will be a number of patients that you will not be able to close; if you have not closed by day 10, you will need to apply additional cover. Other options include skin coverage, which generally will require a releasing incision or a skin graft. The advantage of grafting is that it will correct the catabolic effect of the open abdomen quickly but will doom the patient to a delayed ventral hernia repair. While Cothren’s group reported up to a 100% fascial closure, a recent large series from Germany of 355 patients showed that even when the data is stratifed by year, patients operated within the last 2 years of the study period (2011–2013) achieved only 49% fascial closure [20, 21]. One of the most promising is peritoneal resuscitation with hyperosmolar renal dialysis fuid [22]. Don’t ask for this in the middle of your operation, as there are over 30 different bags of dialysis fuid; avoid the embarrassment and plan ahead! Hypertonic saline intravenously has been used to increase the fascial closure [10]. When closing, nearly 15% will dehisce, consider a supplemental prophylactic onlay mesh or even the retention sutures. The wound appearance and complication rate will be reduced by the application of a closed incision negative pressure therapy system. Skin closure can be with subcuticular (remember love your tissues), even with existing coloniza- tion. If there is some purulent material in the wound, loose interrupted sutures can be used. If there is frank pus, a negative pressure superfcial wound system will facilitate management, and skin edges will heal by secondary intention. Recently the World Society of Emergency Surgery in conjunction with the Abdominal Compartment Society and Donegal Clinical Research Academy recommended the adoption of new key performance indicators for the open abdomen (Table 18. Is the evolving management of intra-abdominal hypertension and abdominal compartment syndrome improving survival? Use of a pathway quality improvement care bundle to reduce mortality after emergency laparotomy. Damage-control laparotomy in nontrauma patients: review of indications and outcomes. Intra-abdominal compartment syndrome as a complica- tion of ruptured abdominal aortic aneurysm repair. Hold the pendulum: rates of acute kidney injury are increased in patients who receive resuscitation volumes less than predicted by the Parkland equation. Institutional practice guidelines on management of pelvic fracture-related hemodynamic instability: do they make a difference? Chasing 100%: the use of hypertonic saline to improve early, primary fascial closure after damage control laparotomy. Intra-abdominal hypertension after life-threatening pen- etrating abdominal trauma: prophylaxis, incidence, and clinical relevance to gastric mucosal pH and abdominal compartment syndrome. Abdominal compartment syndrome and intra-abdominal ischaemia in patients with severe acute pancreatitis. Surgical decom- pression for abdominal compartment syndrome in severe acute pancreatitis. Prospective study examining clinical outcomes associated with a negative pressure wound therapy system and Barker’s vacuum packing tech- nique. Vacuum-assisted wound closure and mesh-mediated fascial traction-a novel technique for late closure of the open abdomen. Prospective evaluation of vacuum-assisted fascial clo- sure after open abdomen: planned ventral hernia rate is substantially reduced. Systematic review and meta-analysis of the open abdo- men and temporary abdominal closure techniques in non-trauma patients. One hundred percent fascial approximation with sequen- tial abdominal closure of the open abdomen. Fascial closure after open abdomen: initial indication and early revisions are decisive factors- a retrospective cohort study. Adjunctive treatment of abdominal catastrophes and sepsis with direct peritoneal resuscitation: indications for use in acute care surgery. Emergency surgery performance, quality and outcome consensus summit-resource for optimal care of emergency surgery. Definitive Closure, Long-Term Results, 19 and Management of Ventral Hernia Leonard Frederik Kroese, Johannes Jeekel, and Johan Frederik Lange Key Points • Open abdomen often leads to giant abdominal wall defects. The sur- vival of conditions requiring open abdomen has greatly increased over the years. In most cases, the frst abdominal wall closure is temporary abdominal wall closure. However, in many cases, open abdomen treatment results in a remaining large ven- tral hernia. These large hernias are associated with complaints of severe back pain, ventilator function disturbances, and chronic wounds or enterocutaneous fstulae, resulting in a great decrease in quality of life [1–3]. The repair of large ventral hernias is technically challenging, and it is associated with long hospital stay, high rates of reoperations and readmissions, impaired wound healing, and high recurrence rates [4–8]. This chapter will describe the basic principles of ventral hernia repair after open abdomen treatment, the different treatment modalities, and future directions. After open abdomen treatment, muscle tension and chronic lateral muscle retraction cause reduction of the intra-abdominal volume (loss of domain). This can cause problems after closure like severe postoperative pain, abdominal hyper- tension, wound dehiscence, ventilatory and/or pulmonary problems, and higher risk of recurrence. After open abdomen, the loss of domain is often seen, increasing the chance of complications after closure surgery. With higher complexity, the number of perioperative measures, risk of complications, and costs rise. Because of the abovementioned reasons, patients with a history of open abdo- men are almost always defned as complex ventral hernia patients.
Syndromes
Newly positive blood culture broths with Gram’s stains consistent with gram-positive cocci in clusters were tested order metformin cheap online diabetes symptoms vs. pregnancy symptoms. Inhibition was seen with only one sample purchase 500 mg metformin visa managing diabetes then told of cancer, and the issue was resolved upon retesting cheap metformin 500 mg otc juvenile diabetes mellitus in dogs. New Methods with Potential for Future Impact The future of clinical diagnostics is anticipated to include a variety of rapid and multiplex methods. It is known that blood culture bottles, positive for bacteria, do not always support cultivation of the pathogen to agar [33, 86]; therefore new molecular methods may allow micro- biology laboratories to identify fastidious pathogens or those damaged by antibiotics. More detailed information about the following techniques may be found in other reviews [87, 88 ]. With accuracy listed as 91 % for the genus level, there is room for improvement; however, the approach shows promise as a rapid method for identification of hematopathogens. Unlike nucleic acid probe assays or microarrays, mass spectrometry does not require prior knowledge of products ana- lyzed, but simply measures the masses of the nucleic acids present in the sample. The platform is significantly different from previous technologies in its ability to detect virtually all microbes from a family and even microbes that have mutated 44 Molecular Niches for the Laboratory Diagnosis of Sepsis 861 significantly. This technology has the potential for identification of all known human microbial pathogens in 4–6 h from blood or sterile body fluids. While the SeptiFast assay may lead to a more rapid and targeted antibiotic therapy early after the onset of fever, the results for sensitivity are low and the cost benefit has yet to be determined. Blood samples for traditional and molecular methods were obtained at the onset of fever, before the implementation of empirical antimi- crobial therapy. The overall agreement between the SeptiFast test and blood culture was 69 % (k= 0. Low sensitivity discour- ages routine use of the test in its present form for the detection of community-onset bloodstream infections [101]. The SeptiFast test was less sensitive than blood cultures; however, some gains were observed for patients treated with antibiotics on admission; three isolates were identified that were not able to be cultivated [98]. Relative to the use of SeptiFast for identification of pathogens in blood culture bottles, Dierks et al. In three samples a treatment adjustment would have been made earlier resulting in a total of eight adjustments in all 101 samples (8 %) [97 ]. The SepsiTest was evaluated in a prospective, multicenter study of 342 blood samples from 187 patients with systemic inflammatory response syndrome, sepsis, or neutropenic fever. The diagnostic sensitivity of the molecular test was 85 % and that of blood culture only 45 %, remaining negative in many cases as a result of antibiotic treatment. These methods’ advantages include speed and ease of use in comparison to traditional 44 Molecular Niches for the Laboratory Diagnosis of Sepsis 863 sequencing technology; disadvantages include the short lengths of sequences that can be currently analyzed. It is ideally suited for applied genomics research including molecular applications for disease diagnosis, clinical prognosis and pharmacogenomics testing. The same group evaluated specimens from iso- lates from neonatal sepsis events, to support species identification that could lead to rapid de-escalation or targeting of antibiotic therapy. Numerous “very major” errors were observed for several of the drug-resistance genes, but demonstrated 100 % sensitivity and specificity, ranging from 95. Molecular Testing for Drug Resistance Rapid and accurate determination of microbial drug susceptibility is actually the most critical challenge; it is essential to facilitate successful antimicrobial therapy of any person, and particularly useful for those with immune function impairment. Rapid testing for genetic resistance markers is an emerging clinical practice that can- not only identify the potential for drug resistance, but also help distinguish ambigu- ous breakpoints associated with susceptibility testing. The application of molecular diagnostic methods to detect drug resistance is evolving. Future methods should facilitate educated choices for therapy, which can be initiated early in diagnosis to impact patient outcomes. Evidence-based studies will be key to the adoption of these new testing antimicrobial testing paradigms. Targets for genetic testing require relative genetic stability of the target sequence, a requirement that demands national and international efforts for monitoring genetic mutations in these target regions. Among bacteria, other useful antimicrobial resistance targets include resistance genes for b-lactams, aminoglycosides, chloramphenicol, fluoroquinolones, glycopeptides, isoniazids, macrolides, mupicurin, rifampin, sulfonamids, tetracyclines, and trimethaprim [110–112]. For fungi, rapid detection of antifungal resistance is useful, primarily due to the increase in fungal infections among immunocompromised patients. Current antifungal assays rely on fungal susceptibility testing which is dependent on growth. The practical application of antifungal molecular testing is yet to be seen, as there is still much to learn about the genetic markers, which mediate resistance. The genetic information needed to examine fungal resistance at the molecular level is complex; a review of molecular mechanisms of antifungal resistance has been published [113]. The full potential of molecular diagnostics for drug resistance testing in microbi- ology has not reached its full potential—its application is still in its infancy. As the molecular mechanisms of antimicrobial resistance are described, newer tech nologies may enhance the utility of such an approach. Furthermore, microarray technology has the promise to impact the rapid and accurate detection of multiple 44 Molecular Niches for the Laboratory Diagnosis of Sepsis 865 mutations associated with resistant bacteria, mycobacterium, viruses, and fungi. Until the full potential of drug resistant markers is understood, rapid molecular anti- microbial testing must still be combined with traditional microbial cultivation [109]. Summary Bacteremia and sepsis are critically important syndromes with high mortality and associated costs. Many septic patients are treated in Emergency Medicine Departments or Critical Care Units, settings in which rapid administration of targeted antibiotic therapy drastically reduces mortality. Unfortunately, routine blood cultures are too slow to support rapid therapeutic inter- ventions. As a result, empiric, broad-spectrum treatment is common—a costly approach that may fail to effectively target the correct microbe, may inadvertently harm patients via antimicrobial toxicity, and may contribute to the evolution of drug- resistant microbes. Several methods for rapid molecular identification of pathogens from blood cul- ture bottles are available. Laboratories can integrate with overall care to support local Surviving Sepsis Campaigns by providing rapid testing to facilitate targeted therapeutic interventions for infections with common hematopathogens. As a result, empiric, broad-spectrum, antibiotic therapy can be shortened to improve survival, reduce health care costs, and decrease antibiotic resistance. More evidence and clinical utility studies are needed to justify the added expense of molecular meth- ods, to determine an appropriate niche in patient populations for which the cost benefit would be favorable. The development of molecular diagnostic assays for detection of single patho- gens from blood culture bottles has already shown to have impact on reducing mor- tality and costs. In the future, tests for multiple pathogens that could characterize gram positive, gram negative, and fungal infections would enable more rapid and targeted antimicrobial interventions for those with severe disease. Targeted drug- resistance genes testing of blood culture bottles will enable risk assessment and guide treatment options for sepsis. Ultimately, early intervention by molecular detection of bacteria and fungi directly from whole blood would provide the most patient benefit and contribute to a tailored antibiotic coverage of the patient early on in the course of the disease, allowing for more effective treatment and better out- comes of patients with sepsis and septic shock.
Denial of hospital privileges as a result of the existence of an exclusive contract with the anesthesiologists in place at the facility has been the source of many lawsuits buy 500mg metformin fast delivery diabetes diet low income, including the well-known Louisiana case of Jefferson Parish Hospital District v Hyde discount 500 mg metformin visa diabetes insipidus word meaning. Thus generic metformin 500mg online diabetes mellitus research paper, existence of an exclusive contract only in the rare setting where anticompetitive effects on patients can be proved might lead to a legitimate antitrust claim by a physician denied privileges. This was proven true in the Kessel v Monongahela County General Hospital case in West Virginia in which an exclusive anesthesiology contract was held illegal. Therefore, again, these arrangements are by definition complex and fraught with hazard. Hospital Subsidies Modern economic realities have forced a great number of anesthesiology practice groups (in both private and academic settings) to recognize that their patient care revenue, after overhead is paid, does not provide sufficient compensation to attract and retain the number and quality of staff necessary to provide the expected clinical service (and fulfill any other group/department missions). Attempting to do the same (or more) work with fewer staff may temporarily provide increased financial compensation. Cutting benefits (discretionary personal professional expenses, retirement contributions, or even insurance coverage) may also be a component of a response to inadequate practice revenue. However, the resulting decrements in personal security, in convenience, and in quality of life as far as acute and chronic fatigue, decreased family and recreation time, and tension among colleagues fearful that someone else is getting a “better deal” will quickly 180 overcome any brief advantage of a somewhat higher income. Therefore, many practice groups in such situations are requesting their hospital (or other health-care facility where they practice) pay them a direct cash subsidy that is used to augment practice revenue in order to maintain benefits and amenities while maintaining or even increasing the direct compensation to staff members, hopefully to a market-competitive level that will promote recruitment and retention of group members. Obviously, requests by a practice group for a direct subsidy must be thoroughly justified to the facility administration receiving the petition. The group’s business operation should already have been examined carefully for any possible defects or means to enhance revenue generation. Explanation of the general trend of declining reimbursements for anesthesia services should be carefully documented. Demand for anesthesia coverage for the surgical schedule is a key component of this proposal. Unfavorable payer mix, impact of contracts, and programs initiated by the hospital are also often major factors in situations of inadequate practice revenue. Always, the group’s good will with the surgeons and the community in general should be emphasized, as well as of the indirect or “behind the scenes” services and benefits the anesthesiology group provides to the hospital. Note that the necessity for such a subsidy request is precisely the time when the anesthesia professionals will benefit from being perceived as “good citizens” of the health-care facility. An overly aggressive effort beyond the bounds of logic could provoke the facility to consider alternative arrangements, even up to the point of putting out a request for proposal from other anesthesiology practice groups. Therefore, thoughtful calculations are required and a careful balance must be sought, seeking enough financial support to supplement practice revenues so that members’ compensation is competitive but not so much as to be excessive. Supporting statements and documents about offers and potential earnings elsewhere must be completely honest and not exaggerated or credibility and good faith will be lost. Further, part of any agreement will be the full sharing of the group’s detailed financial information with the facility administration, both at the time of the request and on an ongoing basis if the payment is more than a one-time “bail out. There may be concern about malpractice liability implications for the hospital even though the 181 practice group stays an independent entity as before. There may be “inurement” or “private benefit” concerns that could be perceived as a threat to the tax-exempt status of a nonprofit hospital. As is almost always the case, expert outside professional consultant advice, usually from an attorney who specializes exclusively in health-care finance contracting, is mandatory in such circumstances. There are other features intermittently along the way, such as the bundled payment models described above. This is a clever and powerful incentive to providers to reduce health-care expenses. It is valuable for anesthesiologists to understand one of the main models advocated by so-called reformers. The most unusual circumstances involve “carve-out” arrangements in which specific very costly and unusual conditions or procedures (such as the birth of a child with disastrous multiple congenital anomalies) are covered separately on a discounted fee-for-service basis. If there were to ever be full capitation, the entire financial underpinning of American medical care would do a complete about-face from the traditional rewards for giving more care and doing more procedures to new rewards for giving and doing less. The provisions setting the boundaries are called risk corridors, and the “stop-loss clauses” add some discounted fee-for-service payment for the excess care beyond the risk corridor (capitated contract limit). Providers who were used to getting paid more for doing more can suddenly find themselves getting paid a fixed amount no matter how much or how little they do with regard to a specified population—hence, the perceived incentive to do, and consequently spend, less. If the providers render too much care within the defined boundary of the contract, they essentially will be working for free, the ultimate in risk- sharing. There are clearly potential internal conflicts in such a system, and how patients reacted initially to this radical change in attitude on the part of physicians where it was actually implemented demonstrated that this overall mechanism is unlikely to be readily embraced by the general public. Physician–hospital organizations are similar entities but involve understandings between groups of physicians and a hospital so that a large package or bundle of services can be constructed as essentially one-stop points of care. Independent practice associations are like preferred provider organizations but are specifically oriented toward capitated contracts for covered lives with significant risk-sharing by the providers. Further, smaller private practice groups of anesthesiologists may find themselves at a competitive disadvantage unless they become part79 of a vertically integrated (multispecialty) or horizontally integrated (with other anesthesiologists) organization. The projected health-care utilization pattern of a large group of white-collar workers (and their families) from major upscale employers in an urban area will be quite different from that of a relatively rural Medicaid population. Specific demographics and past utilization histories are absolutely mandatory for each proposed population to be covered, and this information should go directly to the advising experts for evaluation, whether the proposed negotiation is for discounted fee-for-service, a fee schedule, global bundled fees, or full capitation. Significant questions were pointedly raised about the reimbursement implications for anesthesiologists of the putative managed care/practice 184 reorganization revolution. Much of that discussion has been rendered moot by the failure of the pure prospective capitated payment model to gain widespread adoption. However, if an anesthesia practice or its parent financial entity is ever asked to enter negotiation for a “per member per month” payment for anesthesia services, immediate consultation with independent experts should occur. Discounted fee-for-service arrangements are easier for anesthesiologists to understand because these are directly referable to existing traditional fee structures. Although groups of primary care physicians may view this as somewhat reasonable and, thus, they sign such contracts, anesthesiologists face unique challenges in this regard. Many leaders among anesthesia professionals believe that the Medicare reimbursement rate is unfairly low for the work involved in providing anesthesia care. The Medicare rate likely would remain less than half the per unit “conversion factor” that the large indemnity carriers traditionally have paid for anesthesia care in recent years. Therefore, 125% of what many anesthesia professionals consider woefully inadequate would still be inadequate. Thus, in spite of sometimes intense pressure, anesthesia professionals in many markets have been reluctant to accept indemnity insurance contract rates tied to Medicare rates. As always, anesthesia professionals faced with complex reimbursement situations and decisions should seek expert advice from the national offices of their professional practice organizations and from knowledgeable paid consultants and attorneys. This80 “pay-for-performance” movement began with the federal Tax Relief and Healthcare Act of 2006 and continued with the Physician Quality Reporting Initiative in 2008.
The procedure detailed in this chapter has been used in several approaches during the last years with consistent results and repro- ducibility and has a relatively affordable cost 500mg metformin sale blood sugar by pendulum. Modular incubator chamber (a set of two chambers is neces- sary for simultaneous induction of normoxia order metformin 500mg on line diabete x quiabo, hypoxia buy cheap metformin 500 mg diabetes symptoms yellow tongue, and H/R). Attach a hose (5) with a clamp (6) to the gas cylinder (7) (see Chamber Assembling Note 1). Insert the 1 μm pore size flter (3) between the hose attached to and a Cylinder of Gas the cylinder (5a) and the inlet hose (5b) of the fow meter (2). Connect the outlet hose (5c) of the fow meter to the inlet port of the hypoxia chamber (1). Inside a laminar fow hood, open the chamber and place a petri Chamber Operation dish with sterile water to avoid dehumidifcation. Place the plates or cell culture fasks previously prepared on the superior levels of the chamber. Hypoxia chamber and gas cylinder assembling: (1) modular incubator chamber; (2) fow meter; (3) inlet flter; (4) gas regulator; (5a) cylinder gas hose; (5b) inlet hose; (5c) outlet hose; (6) gas hose clamp; (7) gas cylinder (Modifed from Sagrillo-Fagundes et al. Outside the hood, attach the chamber (inlet port) by the gas hose (5c) to the set of source of gas (7) as described in Subheading 3. The fow meter (2) will indicate the amount of air (L/min) that is accessing the chamber. A fush of 4 min with an amount of 25 L/min is necessary to completely change the gas inside the chamber. After the intended time of air fow, close the gas regulator (4) and then close the inlet and outlet ports of the chamber. The purpose of this last purge is to remove the air presumably pres- ent in the plates, fasks, and dissolved in the culture medium. To confrm the concentration of oxygen in the cell medium Oxygen Measurement kept inside the chamber, it is necessary to use an oxygen elec- (Fig. To create a calibration curve, expose cell media to a range of gas mixtures containing known concentrations of oxygen (e. After acquiring a stable value at each point of the curve, the electrode is ready to be introduced in the medium exposed in the chamber. As the concentration of oxygen is dependent upon the depth within the medium, all the measurements must be held at the same depth [11, 12]. After seeding placental cell lines, primary culture of tropho- of Normoxia, Hypoxia, blasts or explants in appropriate fasks, plates, or petri dish, or H/R: Placental inductions can be performed as necessary (see Note 3), and Studies every 24 h cells are reexposed to the desired gas mixture to reproduce a specifc condition (Fig. Caution is advised for injecting gas inside the chambers due to their relative small size. However, every time that a chamber is opened to treat or change the medium of cells, the gas mixture must be refushed as described in Subheading 3. Jauniaux E, Biernaux V, Gerlo E, Gulbis B trophoblast maintained in organ culture. Soleymanlou N, Jurisica I, Nevo O, Ietta F, phoblast homeostasis against hypoxia/reoxy- Zhang X, Zamudio S, Post M, Caniggia I genation-induced oxidative stress and (2005) Molecular evidence of placental hypoxia apoptosis. Mol Asp Med Pericellular oxygen concentration of cultured 34:981–1023 primary human trophoblasts. Tarrade A, Lai Kuen R, Malassine A, Tricottet 47:104–111 V, Blain P, Vidaud M, Evain-Brion D (2001) 8. Lab Investig 81:1199–1211 Chapter 22 Measurement of Oxidative Stress: Mitochondrial Function Using the Seahorse System Dilys T. These features make a powerful experimental tool to assess cellular respira- tion in various disorders of energy metabolism and mitochondrial function. One disorder in which disruption of mitochondrial metabolism has been implicated is preeclampsia. Proteomic analysis of isolated placental mitochondria identifed altered expression of Padma Murthi and Cathy Vaillancourt (eds. Leung and Simon Chu proteins involved in the regulation of oxidative stress and the respi- ratory chain. Each of these analyzers can be paired with various kits (see Notes 1–4) that the manufacturer (Agilent Technologies) supplies to study specifc aspects of cellular energetics. While these kits provide a standard method for the measure- ment of mitochondrial respiration in live cells, it is possible to design user-defned experiments that utilize alternative stressors, and these as well as the order of injections must be optimized as required by the experiment. However, the basic steps including preparation and cell seeding are applicable to other tests. Refer to the specifc protocol regarding constitution of the compounds for respective kits. Lift sensory cartridge from the utility plate and place it upside Cartridge for Assay down on the bench—avoid contact of the sensors (Fig. Place the sensor cartridge (lid) back onto the utility plate so that the sensors are now submerged in the calibrant. Seed adherent cells at the desired density in 80 μL of cell growth medium into each of wells B to G the day prior to assay (see Note 5). Determine the optimal cell seeding densities from the litera- ture or consult the Seahorse Bioscience Cell Reference Database (http://www. Aspirate 60 μL of cell growth medium (with 20 μL remaining) Culture for Assay and replace with 60 μL of assay medium. Remove 60 μL of medium and fll well with assay medium to a fnal volume of 180 μL per well. Harvest, count, and seed cells at the desired cell density in for Suspension Cells 50 μL of assay medium in wells B to G. Optimization is required should the concentration of the compounds and order of injections be adjusted. If using kits other than the Cell Energy Phenotype Test, load stressor mix in order according to the number of injection included in the protocol. To initiate calibration, select Cell Energy Phenotype Test on the Templates window and make the following adjustments to the protocol. Remove the lid of the utility plate and place the assembly on the instrument tray with the correct orientation as instructed on the screen. Inability of cells to respond to stress may imply underlying mitochon- drial dysfunction. Baseline phenotype refers to the preferred pathway of metabo- lism of the cells in the non-stressed situation or in the presence of non-limiting quantity of substrates. The metabolic potential of the cells refers to the cells’ ability to utilize respiration and/or glycolysis to meet an increased energy demand. Cells can be characterized into four energy phenotypes depend- ing on the pathway(s) they utilize to meet energy demand (Fig.
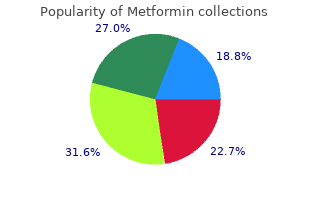
Discount 500mg metformin with visa. Diabetes Deluxe Supply Case featuring the Brooklyn.