
Virginia State University. A. Kerth, MD: "Purchase online Hoodia cheap no RX - Proven online Hoodia no RX".
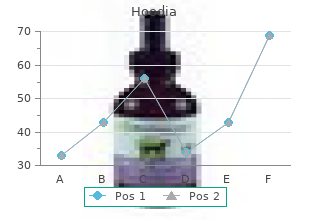
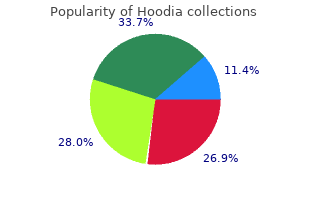
This syndrome may occur from aerosols containing antigens found in small home ultrasonic humidifiers to large industrial units ( 13) order hoodia toronto wicked herbals amped. More recently buy 400 mg hoodia with amex herbals vs pharmaceuticals, respiratory illness related to inhalation of metal working fluids has been reported; this has far-reaching consequences for industry (14 discount 400mg hoodia overnight delivery kisalaya herbals limited,15). Pigeon breeders and bird fanciers have long been recognized to develop hypersensitivity pneumonitis to inhaled antigens in dried avian droppings and feather bloom (6,7). As new cases of hypersensitivity pneumonitis are recognized, measures to identify the antigen and decrease antigen exposure can be implemented. Medications are an important cause of pulmonary disease that resembles hypersensitivity pneumonitis ( 17,18,19 nd 20). Among the implicated medications are nitrofurantoin, amiodarone, minocycline, and sulphasalazine. Specific syndromes of hypersensitivity pneumonitis occur in different parts of the world. Individuals such as stucco makers have developed hypersensitivity pneumonitis to Aspergillus fumigatus contaminated esparto fiber dust in their workplace environments ( 22). Workers in Eastern Canada who are employed in peat moss processing plants are frequently exposed to loose dry material which may contain many microorganisms, of which molds have been implicated in causing hypersensitivity pneumonitis ( 23). Summer-type hypersensitivity pneumonitis due to Trichosporon is an important example of a disease not found in the United States, but is the most prevalent form of hypersensitivity pneumonitis in Japan ( 24). The healthy worker effect and high employee turnover may be partly responsible for the underreporting or underrecognition of work-related cases of hypersensitivity pneumonitis. There is no single confirmatory test for hypersensitivity pneumonitis, not even lung biopsy. The only essential criteria are exposure, sensitization, and clinical response to organic dust or low-molecular-weight compounds. The clinical presentation follows repeat exposure and can vary from sudden and explosive systemic and respiratory symptoms to an insidious, progressive course of dyspnea, fatigue, and weight loss. Based on these clinical presentations, hypersensitivity pneumonitis has been divided into acute, subacute, and chronic forms ( 29). Acute viral or bacterial infections may mimic this presentation, leading to treatment with antibiotics. With avoidance of the allergen, the symptoms spontaneously resolve over 18 hours, with complete resolution within days. The chronic form is characterized by the insidious onset of dyspnea that especially occurs with exertion. Fever is not typical unless there is a high-dose allergen exposure superimposed on the chronic symptoms. The subacute form is characterized by symptoms intermediate to the acute and chronic form with progressive lower respiratory symptoms. The acute and subacute forms may overlap clinically, just as the subacute and chronic forms may. Fine, dry rales may be present, depending on the degree of lung disease present and the timing following the most recent exposure. An acute flare-up of hypersensitivity pneumonitis is associated with an ill-appearing patient in respiratory distress with temperature elevation up to 40 C 6 to 12 hours after antigen exposure. Rash, lymphadenopathy, or rhinitis should prompt investigation for causes other than hypersensitivity pneumonitis. With extensive fibrosis that occurs in the chronic form of the disease, dry rales, and decreased breath sounds predominate. A biphasic obstructive response similar to that seen in asthma has been observed in patients who develop both asthma and hypersensitivity pneumonitis to the same antigen. Although hypoxemia at rest may be observed with severe lung damage, hypoxemia with exercise is common and can be documented by pre- and postexercise arterial blood gas measurements. Bronchial hyperresponsiveness as determined by methacholine challenge is present in a majority of patients with hypersensitivity pneumonitis and is likely due to the inflammatory response of the airways. In subacute and chronic hypersensitivity pneumonitis, there is usually a combination of obstruction and restriction. Transient radiographic changes occur primarily in the acute form with patchy, peripheral, bilateral interstitial infiltrates with a fine, reticulonodular pattern ( 31) as seen in Fig. There may be bilateral ground-glass opacities in the middle to lower lung fields that are indistinguishable from other interstitial lung disorders. These changes usually resolve spontaneously with avoidance or with corticosteroid therapy. In the chronic form, fibrotic changes with honeycombing and areas of emphysema may be seen. In the subacute form, nodular, patchy infiltrates as well as fibrosis may be observed. Chest radiograph of a patient with hypersensitivity pneumonitis demonstrating bilateral lower lobe patchy infiltrates and a reticulonodular pattern. Findings include ground-glass opacification and diffuse consolidation suggestive of alveolar disease. In subacute disease, 1- to 3-mm ill-defined centrilobular nodules with superimposed areas of ground-glass opacity may be seen (33). The role of magnetic resonance imaging has been limited due to respiratory and cardiac motion artifact. Total serum IgE levels are normal unless the patient has coexisting atopic disease (35). Quantitative immunoglobulin measurements are normal, or at times serum IgG may be elevated. The characteristic immunologic feature of hypersensitivity pneumonitis is the presence of high titers of precipitating IgG and other classes of antibodies directed against the offending antigen in the sera of affected patients ( 36). Serum precipitating antibodies, as detected by the Ouchterlony double-gel immunodiffusion technique, indicate antigen exposure, but not necessarily disease. In pigeon breeders, as many as 50% of similarly exposed but asymptomatic individuals may have detectable precipitins ( 37). Enzyme-linked immunosorbent assay and complement fixation techniques for antibody measurements may be too sensitive. If these tests are negative despite a suggestive history, additional testing with antigens specifically prepared from the suspect environment may be necessary. Skin testing with antigens that cause hypersensitivity pneumonitis has been associated with late-onset skin reactions that histologically resemble Arthus-type reactions with mild vasculitis. When differentiating IgE-mediated occupational asthma from hypersensitivity pneumonitis, skin testing can aid in the diagnosis. Both asthma and hypersensitivity pneumonitis may occur in the same individual; in that case, both immediate and delayed reactions to cutaneous testing may occur. Transbronchial biopsy could be attempted, but studies suggest that the sample may not be adequate. Lung biopsy findings depend on the form of the disease and extent of lung damage that has occurred.
Acromegaly causes increased morbidity and r Organomegaly: Thyroid and salivary gland enlarge- mortality mainly due to diabetes and cardiovascular dis- ment order 400 mg hoodia visa lotus herbals, hepatomegaly 400mg hoodia with mastercard herbs de provence substitute. Thyroid axis Macroscopy/microscopy The tumour is solid and trabecular purchase hoodia 400mg without prescription herbals dario bottineau, often 1 cm in diame- terbythe time of diagnosis. Oestrogens conversely increase the sensitivity suppress growth hormone production. Large tumours re-absorption of colloid by the cells and the production may be resected by transfrontal craniotomy. The majority of T is converted from the less active 3 r Octreotide or lanreotide, a long-acting somatostatin T4 by peripheral tissues. Disorders of the thyroid axis are analogue, may be used prior to surgery, following in- shown in Table 11. Fur- Age ther classication is based on whether the patient is hy- Increases with age. Irregularmultinodularenlargementofthethyroidgland, which may be hyperthyroid (toxic) or is commonly eu- thyroid (nontoxic). Clinical features Patients may present for cosmetic reasons, with thyro- Incidence/prevalence toxic symptoms, or because of complications. Multin- 25% of cases of thyrotoxicosis are due to multinodular odular goitre can present with a particularly promi- goitre. Causes include the following: r Benign follicular adenoma: Single lesions with well- Macroscopy/microscopy developed brous capsules. Nodules may be cystic, haemorrhagic and - hormones, which may result in hyperthyroidism. Enlargement of the gland can cause tracheal compres- r Thyroid cyst (15 25%): These may be simple cysts sion leading to shortness of breath and choking. About more common with retrosternal goitre, when the nod- 15% are necrotic papillary tumours. Toxic multinodular goitre has a particularly high incidence of cardiac arrhythmias and other cardiac complications. Clinical features Patients may present with a palpable lump or may be diagnosed on incidental imaging. Ultrasound scanning of the thyroid may be useful r History of neck irradiation exposure. Cystsand r Malignancy is more common in children and patients nodules may be aspirated by ne needle aspiration for over 60 years. Investigations Management r Thyroid function tests are used to determine thyroid Subtotal thyroidectomy may be required for cosmetic status. Isotope scans may also be used to demon- reasons or due to compression symptoms or thyrotoxi- strate either a cold nodule, a hyperactive gland (toxic cosis. Patients must be medically treated and euthyroid multinodular goitre) or a cold gland containing a before surgery. A solitary mass within the thyroid gland that may be r Fine needle aspiration for cytology is used to differen- solid or cystic. Incidence Management 5% of population have a palpable solitary thyroid nod- Benign lesions only require treatment if they cause hy- ule. Up to 50% of population have a solitary nodule at perthyroidism or for cosmetic reasons. Weight loss with increased or normal appetite Graves disease is an autoimmune thyroid disease. Proptosis (exophthalmos) with lid retraction, stare and Sex lid lag are prominent features, and in its most severe F > M form it may cause sight loss due to damage to the optic nerve. Thyroid dermopathy (also called pretibial myxoedema) r Fifteen per cent of patients have a close relative with is a thickening or orange-peel appearance of the skin, Graves, and 50% of relatives have circulating thyroid most often affecting the lower leg. Microscopy The thyroid epithelial cells are increased in number and size with large nuclei. This causes a generalised, uncontrolled stimulation lymphocyte inltration may also be seen. After many years the gland becomes non-functional and Investigations the patient becomes hypothyroid. Other complica- is made by a combination of clinical features and detec- tions of Graves disease may also be due to similar tion of thyroid autoantibodies. Thesecomplicationsdonotresolveontreat- Management ment to reduce the overactivity of the thyroid. Antithyroid drugs (usually carbimazole) are given to r Some symptoms of Graves disease relate to apparent suppress the gland. Graves disease commonly enters catecholamine (noradrenaline and adrenaline) excess, remission after 12 18 months, so a trial of withdrawal for example tachycardia, tremor and sweating. Patients who are severely symptomatic roid hormones induce cardiac catecholamine recep- with hyperthyroidism also benet from -blockers. Subtotal thyroidectomy results in normali- Primary Idiopathic/autoimmune thyroid atrophy sation of thyroid function in 70%. The patient must be made Iatrogenic: radioactive iodine, surgery, drugs euthyroid before surgery with antithyroid drugs and - Iodine deciency (common in Nepal, Bangladesh) blockers (see page 436). Inborn errors of hormone synthesis Secondary Panhypopituitarism due to pituitary adenoma Iatrogenic: pituitary ablative therapy/surgery Prognosis Tertiary Hypothalamic dysfunction (rare) Thirty to fty per cent of patients used to undergo spon- Peripheral resistance to thyroid hormone (rare) taneous remission without treatment. Hypothyroidism (myxoedema) Thyrotoxic crisis (storm) Denition Denition Hypothyroidism is a clinical syndrome resulting from a Arare syndrome of severe acute thyrotoxicosis, which deciency of thyroid hormones. Pathophysiology Congenital hypothyroidism causes permanent develop- Pathophysiology mental retardation. In children it causes reversible de- Levels of thyroid-binding protein in the serum fall and layedgrowthandpuberty,anddevelopmentaldelay. This results in increased cocious puberty may occur in juveniles, due to pituitary free T3 and T4, coupled to increased sensitivity of the hypertrophy. In adults it causes decreased removal of heart and nerves due to the presence of catecholamines. The symptoms include life-threatening coma, heart fail- ure and cardiogenic shock. There is a high fever (38 Clinical features 41C), ushing and sweating, tachycardia, often with Usually insidious onset. Hypercholesterolaemia increases the incidence of tithyroid drugs and corticosteroids. Patients have detectable anti-microsomal antibody and r Gastrointestinal system: Reduced peristalsis, leading antithyroglobulin antibodies in most cases. Although most patients are euthy- puffy face and hands, a hoarse husky voice and slowed roid, thyrotoxicosis can occur and if presentation is late, reexes. The thyroid is diffusely enlarged and has a eshy white cut surface due to lymphocytic inltration, which is seen Investigations on microscopy around the destroyed follicles. Thyroid autoantibodies are High titres of circulating antithyroid antibodies, associ- present in patients with autoimmune disease.
Topical Corticosteroids Cortisone and its derivatives have marked beneficial effects in managing various allergic processes generic hoodia 400mg otc wise woman herbals 1. Corticosteroids are generally considered the most effective medications for the management of the inflammatory component of allergic rhinitis order discount hoodia line herbals dario bottineau. The effectiveness of corticosteroids for the management of allergic rhinitis is most likely related to multiple pharmacologic actions purchase generic hoodia on line equine herbals. Corticosteroids have been demonstrated to have specific effects on the inflammatory cells and chemical mediators involved in the allergic process. Corticosteroids have been considered to increase the synthesis of lipocortin-1, which has an inhibitory effect on phospholipase A 2 and therefore may inhibit the production of lipid mediators ( 91,92 and 93). Corticosteroids reduce seasonally induced increases in nasal mast cells (100) and histamine levels (101), reduce the number of circulating basophils, and inhibit neutrophil influx after allergen challenge ( 102). Studies in patients with allergic rhinitis have demonstrated that these effects of intranasal steroids on rhinitis symptoms are dependent on local activity of the steroids (104,105). When administered topically, the steroid molecule diffuses across the target cell membrane and enters the cytoplasm, where it binds to the glucocorticoid receptor (106). The effect of this interaction is to either induce or suppress gene transcription. After posttranslational processing occurs, the new proteins are either released for extra cellular activity or retained by the cell for intracellular activity ( 107,108 and 109). In addition, the activated glucocorticoid receptors may interact directly with other transcription factors in the cytoplasm and alter the steroid responsiveness of the target cell ( 110). With the exception of beclomethasone dipropionate, these drugs are quickly metabolized to less active metabolites, have minimal systemic absorption, and have been associated with few systemic side effects. The total bioavailability of intranasal budesonide is reported to be 20% (113), and that of flunisolide is reported to be 40% to 50%. There are no reliable data regarding the bioavailability of beclomethasone dipropionate by any route. Intranasal steroids have been helpful in relieving the common allergic symptoms of the upper airway, such as sneezing, congestion, and rhinorrhea. In addition, they may be of value in relieving throat pruritus and cough associated with allergic rhinitis and may also improve concomitant seasonal allergic asthma ( 115). The major side effects of intranasal steroids include local dryness or irritation in the form of stinging, burning, or sneezing ( 116) (Table 9. With prolonged administration of intranasal steroids, periodic examination of the nasal cavity is warranted, especially in patients who experience nasal crusting or bleeding ( 117,118). The incidence of local irritation with intranasal steroids has been reduced by the development of aqueous formulations of these drugs (119,120), and the subsequent reduction in local irritation with these preparations has increased their use in children. Complications of topical steroids sprays Long-term use of intranasal steroids does not appear to cause any significant risk for adverse morphologic effects in the nasal mucosa. In a study of patients with perennial rhinitis treated with mometasone for 12 months, nasal biopsy specimens showed a decrease in focal metaplasia, no change in epithelial thickness, and no sign of atrophy (121). In a study of intranasal steroid treatment in 90 patients with perennial rhinitis, nasal biopsy specimens revealed normalization of the nasal mucosa at the end of the 12-month study period (122). Systemic side effects are generally not considered a serious risk associated with intranasal steroids, although early studies of intranasal dexamethasone administration at dosages used in allergic rhinitis produced mild to moderate adrenal suppression ( 123,124). However, clinical experiences with intranasal fluticasone (125), triamcinolone (126), and mometasone have indicated no reports of systemic side effects. Bilateral posterior subcapsular cataracts have been reported in association with nasal or oral inhalation of beclomethasone dipropionate, although many of these patients had used higher-than-recommended doses or had received concomitant oral steroid therapy ( 127). In a case-control study, nasal steroids were not associated with an increased risk for ocular hypertension or open-angle glaucoma, whereas prolonged administration of high doses of inhaled steroids increased the risk for these adverse effects (128). Initially, some patients may require topical decongestants before administering intranasal steroids. In some patients, the congestion is so severe that a 3- to 5-day course of oral corticosteroids is required to allow delivery of the intranasal steroids. In contrast to decongestant nasal sprays, patients should be informed that intranasal steroids should be used prophylactically and that maximum benefit is not immediate and may take weeks. Although a delayed onset of action with the intranasal steroids may occur in some patients, well-controlled studies ( 129,130,131 and 132) have shown that many patients have a clinically evident onset of effect during the first day of administration. Some studies suggest that intranasal steroids can be used on an as-needed basis by many patients, but for some patients, optimal effectiveness can be achieved only with regular use ( 133,134). Intranasal Corticosteroid Injection Intranasal corticosteroid injections have been used for clinical practice in the management of patients with common allergic and nonallergic nasal conditions such as nasal polyposis. With the advent of newer and safer intranasal steroids, the use of this technique has decreased in recent years. Turbinate injections have two major adverse effects that are not seen with intranasal corticosteroid sprays: (a) adrenal suppression secondary to absorption of the steroid, and (b) absorption of steroid emboli, which may lead to transient or permanent loss of vision ( 135). Systemic Corticosteroids Systemic corticosteroids are regarded by many allergists as inappropriate therapy for patients with mild to moderate allergic rhinitis. Although rhinitis is not a threat to life, it can seriously impair the quality of it, and some patients respond only to corticosteroids. Also, when the topical steroid cannot be adequately distributed in the nose because of marked obstruction, it will not be effective. In such cases, the blocked nose can be opened by giving a systemic corticosteroid for 3 to 7 days, and the improvement can then be maintained by the topical corticosteroid spray. It is essential always to relate the risk for side effects to the dosage given, and especially to the length of the treatment period. When short-term systemic steroid treatment is given for 1 to 2 weeks, it can be a valuable and safe supplement to topical treatments in the management of severe allergic rhinitis or nasal polyposis. As in the use of topical corticosteroids, however, systemic steroids should be reserved for severe cases that cannot be controlled by routine measures and should be used for a limited period and never on a chronic basis. Anticholinergics Ipratropium is an anticholinergic drug that was released in recent years for treatment of chronic bronchitis and chronic obstructive lung disease. It has a quaternary ammonia structure, which gives this medication high topical activity, but because of its structure, there is no appreciable absorption of this medication across mucosal barriers. Therefore, the unpleasant anticholinergic side effects commonly associated with atropine are not experienced with this medication. Because cholinergic mechanisms in the nose may lead to hypersecretion and blood vessel dilation, interest in this medication has increased. Ipratropium decreases the watery rhinorrhea in patients with perennial rhinitis ( 136) and reduces nasal drainage in patients with the common cold or vasomotor rhinitis ( 137). Unfortunately, it has no appreciable effect on obstruction or sneezing in patients with rhinitis. Intranasal Cromolyn Cromolyn sodium is a derivative of the natural product khellin. The proposed mechanism of action of cromolyn in allergic rhinitis is to stabilize mast cell membranes, apparently by inhibiting calcium transmembrane flux and thereby preventing antigen-induced degranulation. It has been reported to be effective in the management of seasonal and perennial allergic rhinitis ( 138,139). Cromolyn can be effective in reducing sneezing, rhinorrhea, and nasal pruritus ( 140,141) but is minimally useful in nonallergic types of rhinitis and nasal polyps ( 142) and has little effect on mucociliary transport.