
United States Coast Guard Academy. I. Angar, MD: "Buy Rumalaya forte online - Quality Rumalaya forte online".
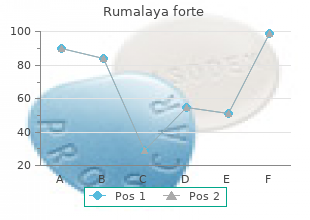
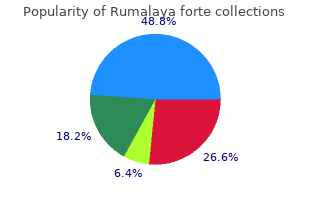
When proptosis develops in a young child purchase rumalaya forte line spasms movie 1983, the clinician must examine its abdomen to exclude neuroblastoma buy cheap rumalaya forte 30pills on-line spasms just before falling asleep. Probably metastasis in the skull from the adrenal occurs through the vertebral system of veins best order rumalaya forte spasms temporal area. So the parents of the children first point out swelling of the head, proptosis with or without ecchymosis of the eyelid. Sometimes this tumour is presented with extensive bony metastasis, pallor and severe anaemia without other findings. As this tumour is more embryonic in nature, it tends to secrete large amounts of dopamine instead of epinephrine or norepinephrine. Widespread necrosis may occur in the tumour which destroys many of the tumour cells. Although mortality of the neuroblastoma is high, there is a better prognosis if the diagnosis is made before 1 year of age. It is a benign tumour and least harmful among the 3 tumours of the adrenal medulla. It sometimes presents as a fusiform radio-opaque lesion in the paravertebral gutters in straight X-ray in the course of routine investigations. If the leftgland is seen to be atrophic, it is highly probable that there is a tumour on the right side, which should be operated on. If the left gland is seen to be hyperplastic or normal subtotal (90%) adrenalectomy should be performed. If after performing left sided adrenalectomy, it is found that the patient will not tolerate a bilateral operation, exploration of the right side should be postponed. When the bilateral adrenalectomy has to be performed, anterior approach should be adopted. If the lesion is localised to one side (aldosteronoma) and has been identified with certainty, thepostero-lateral approach is used. This can also be achieved with the break of the table under the 12th thoracic vertebra. If access is inadequate, the incision is extended laterally through the rectus muscle at the level of the transpyloric plane to the costal margin. A curved transverse incision, convex upwards with its centre 5 cm above the umbilicus, is sometimes preferred. This not only gives a better access, but being transverse, the incision heals rapidly. For postero-lateral approach, an incision is made over the 11th rib from the lateral border of the sacrospinalis to the abdominal wall. A hand is insinuated to push the spleen medially and the posterior layer of the lienorenal ligament is incised. The spleen is further turned medially together with the tail of the pancreas and the splenic vessels. The large adrenal vein is identified, emerging from the inferomedial angle and draining into the renal vein. The gland is gradually mobilised and the fine medial arterial attachments are cauterised with diathermy. The liver is retracted upwards and the hepatic flexure of the colon and duodenum are packed downwards. The posterior parietal peritoneum is incised transversely just above the duodenum to the border of the inferior vena cava. The layers of the posterior parietal peritoneum are reflected upwards and downwards. On the medial side of the gland, one or more adrenal veins will be seen draining to the inferior vena cava. The gland is gradually mobilised and the residual arterial bleeding is stopped by diathermy cauterisation. It is always essential to search for ectopic adrenal tissue before completing the operation. The lumbodorsal fascia is incised and the sacrospinalis muscle is retracted medially. The arteries and vein of the adrenal gland are identified, tied securely and divided. If the pleura has been injured, a small chest tube is put inside the pleural cavity and under-water seal drainage is given. When bilateral adrenalectomy will be required, corticosteroids should be administered preoperatively. This dose is continued till 3rd or 4th postoperative day after which the patient can be given cortisone acetate orally. Only the pectoral portion thickens and takes the appearance of a lens-shaped thickening. Gradually from this thickening on the milk line growth of ectoderm occurs in the form of 15 to 20 solid cords to form the rudimentary mammary gland. These cords show bulbous dilatations at their ends from which alveoli of the gland develop. The solid cords develop in the 5 th month of foetal life and these gradually turn into ducts by hollowing during 7th or 8th month of foetal life. At this period the skin from which the ducts develop show a small depression which corresponds to the nipple and the ducts turn to be milk ducts. Just before or soon afterbirth themasenchym underlying this depression proliferates and makes it everted to form the nipple. The areola is slight thickening in the skin which contains a few glands of Montgomery. The areola, soon after birth, distinguishes itself by slight increase in pigmentation. The 15 to 20 milk ducts and their alveoli ultimately form 15 to 20 lobules at the age of puberty. Soon after birth bilateral or unilateral enlargement of the breast occurs in majority of infants. Transversely it extends from the side of the sternum to near the mid-axillary line. The superolateral part of the breast is prolonged upwards and laterally towards the axilla forming the axillary tail of Spence, which pierces the deep fascia to lie in close relationship with the pectoral group of axillary lymph nodes. Neoplasms or deformities affecting this tail are often confused with the lymph nodes enlargement. The deep surface of the breast is slightly concave and is in direct relation with the deep fascia which separates the breast from the following muscles — Pectoralis major, Serratus anterior, Obliquus extemus abdominis and the aponeurosis of the last muscle as it forms the anterior wall of the sheath of the rectus abdominis. Between the breast and the deep fascia there is a space containing loose areolar tissue which is known as retromammary or submammary space and this allows the breast to be movable on the deep fascia covering Pectoralis major. Only when advanced cancer of the breast has involved the fascia covering pectoralis major the breast becomes fixed to certain extent.
Testing the Patch Confirm the security of the patch closure by injecting air into the nasogastric tube and watching for air bubbles under Fig order rumalaya forte 30 pills on line muscle relaxant education. The endoscope is passed into the duode- that one limb of each staple goes through the omentum and num and the perforation visualized purchase generic rumalaya forte online muscle relaxant safe in breastfeeding. There is danger passed through the perforation and used to stabilize the that the staple does not adequately secure a purchase in the omentum during suturing rumalaya forte 30 pills amex muscle relaxant 1. Close the scope at the end ensures that staples or sutures have not the stapler slowly. Insufflation with the scope replaces slightly to prevent inadvertent injury to the back wall of the injection of the air through the nasogastric tube when the duodenum (Fig. Scott-Conner first postoperative week is dominated by the physiologic response to the perforation and associated peritonitis. The advantages of the laparoscopic approach generally do not become obvious until the second or third week after surgery. Evaluation for and treatment of Helicobacter pylori is cru- cial to prevent recurrent symptoms. Complications Failure to recognize a malignant perforation Inadequate patch closure resulting in continuing sepsis Subphrenic or subhepatic abscess Further Reading Fig. Laparoscopic omental patch repair of perforated duodenal ulcer with an automated stapler. A randomized study compar- ing laparoscopic versus open repair of perforated peptic ulcer using Postoperative care is the same as that required for the open suture or sutureless technique. Generally a day or two of nasogastric suction is Laparoscopic and endoscopic management of perforated duodenal required until the gastric ileus subsides, and it allows addi- ulcers. Laparoscopic repair/perito- treatment is the same as that used for an open procedure. Chassin† Indications Stamm gastrostomy, as the Janeway construction does not require an indwelling tube. Percutaneous endoscopic gas- Gastric decompression without the need for a tube traversing trostomy is an alternative for many patients. A tube across the esophagogastric junction ren- When constructing a tube gastrostomy, the gastrostomy ders the distal esophageal sphincter ineffective. Otherwise, gastric contents may leak out around the tube and Gastric tube feeding with similar constraints as noted above. When the gastrostomy is no longer needed, removal of the tube usually When performed as part of another abdominal procedure, the results in prompt closure of the tract. If necessary, it gastrostomy creates a simple gastrostomy analogous to a Stamm can be extended upward into the epigastrium to expose the but without the inversion of the gastric wall and additional secu- stomach. When gastrostomy is performed as a single proce- rity afforded by suturing the anterior gastric wall to the abdomi- dure, a short upper midline incision generally suffices. Choose a location in the midportion of the stomach, closer For patients who require long-term gastric tube feeding, to the greater curvature than to the lesser curvature the Janeway gastrostomy is more convenient than the usual (Fig. With electrocau- tery make a stab wound in the anterior gastric wall in the mid- dle of the previously placed purse-string suture (Fig. Insert the catheter into the stomach, tighten the purse-string suture, and tie it to invert the gastric serosa (Fig. If a Foley catheter was used, inflate the balloon and draw the stomach toward the anterior abdominal wall. When these four Lembert sutures are tied, the anterior gastric wall is firmly anchored to the abdominal wall (Fig. Janeway Gastrostomy, Stapled Make a 10- to 12-cm midline incision in the midepigastrium. Grasp the gastric nipple and draw it to the outside by curvature; then apply a cutting linear stapling device passing a Babcock clamp into the incision in the rectus mus- (Fig. This brings the gastric wall into contact with the ante- and incise for a distance of about 4 cm between the staples rior abdominal wall, to which it should be fixed with two (Fig. Then transect the tip of the gas- mucosa about 4 cm in length, which is sufficient to pass tric nipple with Mayo scissors, leaving enough gastric tissue through the abdominal wall. Mature the gastrostomy with inter- seromuscular Lembert sutures to invert the staples (Fig. Chassin Close the abdominal incision in the usual fashion and apply a sterile dressing (Fig. After healing has taken place, gastric feeding can be started by inserting a catheter into the stomach while the nutrients are being administered. Utilization and outcomes of surgical gastrostomies and jeju- nostomies in an era of percutaneous endoscopic gastrostomy: a population-based study. Outcomes of surgical, percuta- neous endoscopic, and percutaneous radiologic gastrostomies. Laparoscopic gastrostomy and jejunostomy: safety and cost with local vs general anesthesia. Albumin level and patient age predict outcomes in patients referred for gastrostomy insertion. Laparoscopic Janeway gastrostomy: an alternative to celiotomy for the management of a dislodged percuta- neous gastrostomy. Retrospective analyses of complications associated with transcutaneous replace- ment of percutaneous gastrostomy and jejunostomy feeding devices. Frozen sections are helpful for evaluating proximal and dis- Inadequate resection tal margins. As with many gastrointestinal malignancies, gas- Injury to pancreas, spleen tric cancer may extend submucosally for several centimeters Ischemia of gastric pouch if splenectomy is performed beyond the obvious tumor mass. Perigastric nodal metastases stations are numbered 1 through 6 and regional nodal stations Document frozen sections taken, if any, and results are 7–12. Nodal stations numbered higher than 12 are generally Extent of lymphadenectomy considered “distant” nodal stations and are not dissected for the Type of reconstruction standard D2 nodal dissection. While the classic D1 nodal dissection is defined by complete dissection of the first tier nodal stations which are determined by the location of the primary lesion and is most compatible with current concept of the “D1 nodes, perigastric nodes (station 1–6)” in western literature, current (2010) definition of D1 nodal dis- H. The survival benefit of D2 nodal dissection is still a topic of debate; however, superior locoregional cancer control has been demonstrated in large randomized trial. Generally such extension is obvious on the preop- erative imaging studies, but the surgeon must be prepared to excise any involved adjacent organs in continuity. Posteriorly, the tumor can invade the body or tail of the pancreas, the middle colic artery, or the transverse colon; all of which can be included in the specimen. Extension into the left lobe of the liver is amenable to resection, as is extension into the crus of the diaphragm. Generally, survival is poor when extensive tumor dictates excision of adjacent organs. Pancreatico-Splenectomy, Splenectomy Historically a splenectomy plus distal pancreatectomy have been an integral part of the classic D2 nodal dissection to Fig. Previous randomized trials examining D1–D2 nodal specific group of patients in Japan. Currently splenectomy and distal pancreatectomy are not recommended for nodal clearance in North America Blood Supply to Residual Gastric Pouch and Europe.
The more sophisticated technique is the introduction of magnetic resonance angiography without the need of direct arterial puncture order rumalaya forte 30pills free shipping spasms in 6 month old baby. When this technology will advance generic rumalaya forte 30 pills otc muscle relaxant toxicity, obviously the catheter based contrast studies will be reduced order rumalaya forte visa spasms under xiphoid process. Exercise, if performed within limits, often reduces pain of intermittent claudication and may help in spontaneous cure. Both these diseases play a considerable role in the development of atherosclerosis. This may be performed by reducing walking, stopping cycling and by wearing shoes with high heel to diminish action of calf muscles. So nail cutting should be done cautiously and at the same time any minor trauma should be avoided. A few antihypertensive agents, particularly beta-blockers may reduce claudication distance. Aspirin in the dose of 75 mg to 300 mg daily is quite a good and easily available drug in this group. If there is raised blood lipids, drug treatment should be used to reduce these to normal level. Praxilene (Naftidrofuryl oxalate) may increase the claudicating distance by allowing a greater oxygen debt to be incurred, but the actual ultimate benefit is quite negligible. Trental (oxpentifylline) reduces blood viscosity and thus may be of some benefit, but not quite satisfactory. Intra-arterial administration of vasodilator drugs at the selective site by injection has been successful as a temporary method. Paravertebral injection of local anaesthetics near the sympathetic chain has also improved circulation of the limbs. In case of lower limb, injection is made by the side of the L2, 3 and 4 vertebrae. The procedure is better carried out under X-ray control and a small injection of contrast medium (Hypaque solution) may precede the proper injection of phenol. The main danger is to penetrate the aorta or the vena cava which can be detected by drawing back the piston of the syringe which will show indrawing of blood into the syringe. It is still very doubtful how much muscular blood supply is improved by sympathectomy, but it is almost certain that it increases blood supply to the skin and subcutaneous tissue. Its main indications are — (i) Rest pain and minor ulceration, which are not amenable to direct arterial surgery. This can be achieved by— (i) Division of nerves to the gastrocnemius and soleus in the popliteal fossa. The followings are the different types of surgery which are used for chronic arterial occlusions. In certain cases of arterial spasm adventitial injection of papaverine may cure the condition. In these cases the affected portion is removed and if this segment is small, end-to-end suturing may become possible without any tension to the suture line. If the affected segment is long, a Dacron graft or a reversed long saphenous vein graft may be used to make good the loss of the segment. When the affected segment is small, a longitudinal incision is made over the diseased segment and is made deep till the atheromatous plaque is reached. The diseased intima, atheromatous plaque and the thrombus are removed through a plane of cleavage through the middle of the tunica media. The arteriotomy is then closed with continuous 5/0 polypropylene (prolene) suture with or without a vein patch graft. In case of longer diseased segment, arteriotomies are made only at the upper and lower ends of the diseased segment. An endarterectomy loop is inserted through the lower arteriotomy and is pushed upwards dissecting and separating the atheromatous plaque as far as the upper arteriotomy. Modern knitted prostheses leak even less as they are sealed with gelatin or collagen by the manufacturer. In fact there is probably little to choose between the types of Dacron graft to be used. In aorto-iliac occlusion mostly synthetic grafts are applied, whereas in femoro-popliteal occlusion, autogenous vein graft is mainly used. In case of aorto-iliac occlusion suture material used is monofilament polypropylene — 2/0 or 3/0. In femoropopliteal occlusion at the groin, 4/0 or 5/0 polypropylene is used; whereas in case of further down limb occlusion 7/0 suture material is used. The balloon is inflated with dilute contrast medium to a pressure of 5 to 10 atmospheres for a period of 15 to 30 seconds even upto 1 minute, after which it is deflacted. Expansion of the balloon produces fissures in atheromatous plaques and also ruptures muscle fibres of the tunica media thus widening the lumen and ensuring blood supply to the distal limb. This technique is mainly used in case of arterial occlusions of the iliac artery, superficial femoral or renal artery. Gradually the endothelial lining develops along the fissures in the atheromatous plaque within a few months. The balloon is positioned within the stenosis or occlusion which is confirmed by angiography. The problem is that often the vessel fails to stay adequately dilated after such treatment and in these cases metal stent may be used. In this technique the balloon catheter is introduced through the expanding stent and then the balloon is inflated. There is also a type of self-expanding stent, which is held compressed by a sheath of plastic before application. This procedure is not as good as reconstructive surgery, and is only used when latter type of surgery is not possible. However the advantage of this procedure is that it can be repeated if stenosis recurs. So that blood from the patent femoral artery is carried through the graft to the other femoral artery of the ischaemic side. A Dacron graft connects the common femoral artery to a thromboendarterectomised upper popliteal artery. A vein graft is again connected from this rebored upper popliteal artery to the arteries below the knee. In its upper part it is anastomosed with the axillary artery in an end-to-side fashion. In its lower end it is anastomosed to the femoral artery of the involved limb in the same fashion. By this blood flows sufficiently from the axillary artery to revascularise the lower limb.