
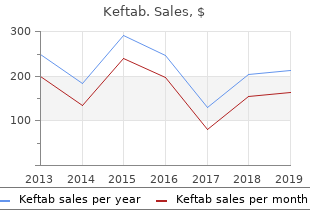
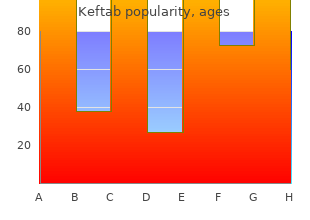
University of Great Falls. E. Potros, MD: "Buy Keftab online no RX - Best Keftab online".
Mechanical circulatory support (see also Chapter 29) or extracorporeal membrane oxygenation may allow a bridge to transplantation or recovery in patients with cardiogenic shock despite optimal medical care order keftab american express antibiotics penicillin allergy. In those patients who recover buy discount keftab online going off antibiotics for acne, the time to recovery in acute myocarditis varies order keftab without a prescription antibiotic uti, ranging from a few weeks to a few months. Transplantation also is an effective therapy for patients with myocarditis who have refractory heart failure despite optimal medical therapy and mechanical circulatory support. Survival rates after transplantation for myocarditis are similar to survival rates for other causes of cardiac transplantation. However, the risk of graft loss may be greater in children who undergo transplantation. Future Perspectives One of the major gaps in the management of myocarditis is the lack of a sensitive and specific noninvasive test. In this regard, diagnostic techniques are evolving to identify novel blood-based biomarkers reflecting cardiac inflammation through microarray and proteomic analysis of tissues from 38 both laboratory models and patient samples. Moreover, with improved understanding of pathophysiologic mechanisms, new therapies also are being developed and evaluated in clinical trials. These new treatments, including cell-based therapies that selectively inhibit T cell responses, induce apoptosis of activated T cells, and increase Treg cells, will be evaluated in planned clinical trials. Such prospective investigations should be designed specifically to establish efficacy in women. Translational studies focused on genomic markers in biopsy samples and peripheral blood should help refine risk assessments and target therapies to the populations at highest need. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. The global burden of myocarditis: part 1: a systematic literature review for the Global Burden of Diseases, Injuries, and Risk Factors 2010 study. Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities: Task Force 3: Hypertrophic Cardiomyopathy, Arrhythmogenic Right Ventricular Cardiomyopathy and Other Cardiomyopathies, and Myocarditis: A Scientific Statement From the American Heart Association and American College of Cardiology. Incidence and Etiology of Sudden Cardiac Arrest and Death in High School Athletes in the United States. Utility of immunofluorescence and electron microscopy in endomyocardial biopsies from patients with unexplained heart failure. Viral endomyocardial infection is an independent predictor and potentially treatable risk factor for graft loss and coronary vasculopathy in pediatric cardiac transplant recipients. A distinct subgroup of cardiomyopathy patients characterized by transcriptionally active cardiotropic erythrovirus and altered cardiac gene expression. Notes from the field: update on Lyme carditis, groups at high risk, and frequency of associated sudden cardiac death—United States. Current epidemiological trends for Chagas disease in Latin America and future challenges in epidemiology, surveillance and health policy. Chagas disease in Latin America: an epidemiological update based on 2010 estimates. A prospective study of the incidence of myocarditis/pericarditis and new onset cardiac symptoms following smallpox and influenza vaccination. Virus-induced Abl and Fyn kinase signals permit coxsackievirus entry through epithelial tight junctions. Cardiac deletion of the Coxsackievirus-adenovirus receptor abolishes Coxsackievirus B3 infection and prevents myocarditis in vivo. Inhibition of Coxsackievirus-associated dystrophin cleavage prevents cardiomyopathy. The tyrosine kinase p56lck is essential in coxsackievirus B3- mediated heart disease. Development of diastolic heart failure in a 6-year follow- up study in patients after acute myocarditis. Cardiac sarcoidosis and giant cell myocarditis as causes of atrioventricular block in young and middle-aged adults. Diagnosis, treatment, and outcome of giant-cell myocarditis in the era of combined immunosuppression. Autoimmunity against M2 muscarinic acetylcholine receptor induces myocarditis and leads to a dilated cardiomyopathy-like phenotype. Consequences of unlocking the cardiac myosin molecule in human myocarditis and cardiomyopathies. Circulating cardiac troponins levels and cardiac dysfunction in children with acute and fulminant viral myocarditis. Cardiac troponins and autoimmunity: their role in the pathogenesis of myocarditis and of heart failure. Cardiac troponin-I as a screening tool for myocarditis in children hospitalized for viral infection. Management and outcomes in pediatric patients presenting with acute fulminant myocarditis. Clinical implications of anti-heart autoantibodies in myocarditis and dilated cardiomyopathy. Prognostic electrocardiographic parameters in patients with suspected myocarditis. Long-term follow-up of biopsy-proven viral myocarditis: predictors of mortality and incomplete recovery. Comprehensive Cardiac Magnetic Resonance Imaging in Patients With Suspected Myocarditis: The MyoRacer-Trial. Cardiac positron emission tomography enhances prognostic assessments of patients with suspected cardiac sarcoidosis. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Complication rate of right ventricular endomyocardial biopsy via the femoral approach: a retrospective and prospective study analyzing 3048 diagnostic procedures over an 11-year period. Comparative evaluation of left and right ventricular endomyocardial biopsy: differences in complication rate and diagnostic performance. Contribution and risks of left ventricular endomyocardial biopsy in patients with cardiomyopathies: a retrospective study over a 28-year period. The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Evaluation of the role of endomyocardial biopsy in 851 patients with unexplained heart failure from 2000-2009. Outcomes and predictors of recovery in acute-onset cardiomyopathy: A single-center experience of patients undergoing endomyocardial biopsy for new heart failure. Good prognosis for pericarditis with and without myocardial involvement: results from a multicenter, prospective cohort study. Ventricular remodeling and survival are more favorable for myocarditis than for idiopathic dilated cardiomyopathy in childhood: an outcomes study from the Pediatric Cardiomyopathy Registry. Competing risks for death and cardiac transplantation in children with dilated cardiomyopathy: results from the pediatric cardiomyopathy registry.
Terlipressin is almost completely syndrome generic keftab 250mg antimicrobial effect of aloe vera, 1 mg every 6 hours cheap 500 mg keftab overnight delivery bacteria use restriction enzymes to, if the metabolised in the kidneys and liver cheap keftab 375mg amex bacteria dichotomous key, with creatinine hasn’t reduced by 30% after less than 1% of terlipressin and less than 0. In ● Manufacturer advises to monitor patients plasma, unchanged thalidomide represents closely due to lack of studies. Talidomide addition to thalidomide, hydrolytic products for the treatment of uraemic pruritis: a N-(o-carboxybenzoyl) glutarimide and crossover randomised double-blind trial. Demethylation ● Calcium-channel blockers: concentration to 3-methylxanthine (and possibly to increased by diltiazem and verapamil and 1-methylxanthine) is catalysed by the possibly other calcium-channel blockers. Molecular weight 412 ● Antipsychotics: anticonvulsant effect (daltons) antagonised. Less than 2% of the dose is excreted unchanged in urine ● Although there is no evidence of and faeces. Te primary route of ticagrelor elimination ● Lipid-regulating drugs: concentration of is via hepatic metabolism. Te primary route simvastatin increased – increased risk of of elimination for the active metabolite is toxicity. Volume of distribution 7–9 ● Oestrogens: possibly reduced (L/kg) contraceptive effects of oestrogens (risk Half-life – normal/ 42/Probably probably small). Up to 90% may occur if treatment exceeds a period of a dose is excreted unchanged in the urine, of 14 days and can present up to 6 weeks mostly within 6 hours after a dose. Is impaired renal function renally excreted and hence accumulate a contraindication to the use of low- in severe renal impairment. If prothrombin time is still tinzaparin can safely be used in elderly raised 2–4 hours later, give 0. Tipranavir is metabolised by the cytochrome ● Beta-blockers: avoid concomitant use with P450 system (mainly the isoenzyme metoprolol for heart failure. Te metabolites (mainly inactive) constitute ● Pharmacokinetic data suggest that renal 70% of the administered dose and are clearance in the elderly may be decreased excreted via the renal route. A case of active rheumatoid arthritis with renal dysfunction treated effectively with tocilizumab monotherapy. Approximately 60% of a dose is excreted in the urine with the remainder appearing in the faeces. Tolfenamic acid is metabolised in the liver; ● Diuretics: increased risk of nephrotoxicity; the metabolites and unchanged drug are antagonism of diuretic effect; conjugated with glucuronic acid. Topotecan: a review of its microsomal enzymes to an active metabolite, efficacy in small cell lung cancer. Te inactive metabolites are if hypokalaemia occurs; enhanced excreted in the urine. An update of its ● In patients with renal failure, the renal pharmacological properties and therapeutic clearance is reduced but total plasma efficacy. Volume of distribution 580 litres ● Cytotoxics: possible increased risk of (L/kg) ventricular arrhythmias with vandetanib Half-life – normal/ 5 days/Unchanged – avoid. Volume of distribution 163–243 litres ● Antipsychotics: enhanced hypotensive (L/kg) and sedative effects; increased risk of Half-life – normal/ 6/11 convulsions. Tramadol is metabolised by N- and ● Sodium oxybate: enhanced effect of O-demethylation via the cytochrome sodium oxybate – avoid concomitant use. Volume of distribution 18 litres ● Potassium salts: increased risk of (L/kg) hyperkalaemia. Trastuzumab is most likely removed by ● Dilute dose in 250 mL sodium chloride opsonisation via the reticuloendothelial 0. Molecular weight 253 ● Antibacterials: avoid concomitant use with (daltons) lymecycline. Volume of distribution 160 ● Antimalarials: avoid concomitant use with (L/kg) artemether/lumefantrine and piperaquine Half-life – normal/ 22/– with artenimol. Trifluoperazine undergoes extensive first- ● Antivirals: concentration possibly pass metabolism. Trimipramine is excreted increased antimuscarinic effects in the urine mainly in the form of its with clozapine and phenothiazines; metabolites. However, in practice this results in severe aciclovir toxicity, especially in patients with poorly functioning grafts. It is excreted in the ● Ulcer-healing drugs: metabolism inhibited urine almost entirely in the form of its by cimetidine, increased concentration. Volume of distribution 17 ● Tacrolimus: increased risk of (L/kg) hyperkalaemia and nephrotoxicity. Volume of distribution 7450 litres ● Antihistamines: possibly increased risk of (L/kg) ventricular arrhythmias with mizolastine Half-life – normal/ 19 days/Increased – avoid. Volume of distribution 91–106 litres ● Antipsychotics: avoid concomitant use (L/kg) with clozapine, risk of agranulocytosis. Volume of distribution 3–6 ● Antibacterials: metabolism increased by (L/kg) rifampicin; metabolism possibly inhibited Half-life – normal/ 4. Of these only norverapamil has imipramine and possibly other tricyclics any significant activity (approximately 20% increased; concentration significantly that of the parent compound). Norverapamil represents about 6% of the ● Anti-epileptics: effect probably reduced dose eliminated in urine and reaches steady- by barbiturates, phenytoin and primidone; state plasma concentrations approximately enhanced effect of carbamazepine. About 70% of a ● Antifungals: negative inotropic effect dose is excreted by the kidneys in the form possibly increased with itraconazole. Monitor carefully ● Beta-blockers: enhanced hypotensive 10–20 Dose as in normal renal function. Molecular weight 923 ● Antimalarials: avoid with piperaquine with (daltons) artenimol. Dose as ● Treatment of advanced breast cancer fl u x in normal renal function and (where other anthracyclines have failed) monitor closely. Volume of distribution ● Antipsychotics: avoid concomitant >40 (L/kg) use with clozapine (increased risk of agranulocytosis). Dose as ● In patients where >75% of the liver in normal renal function and volume has been replaced by metastases, monitor closely. Te S-isomer is metabolised tramadol, trimethoprim, valproate, more rapidly than the R-isomer, mainly by venlafaxine, vitamin E and voriconazole. Pharmacodynamics and pharmacokinetics of xipamide in patients with normal and impaired kidney function. Zafirlukast is extensively metabolised in ● Anticoagulants: may enhance the effects the liver, mainly by the cytochrome P450 of warfarin. Tese amino lower than 5 mcg/mL in an external pump acids are expected to be taken up by cellular and 25 mcg/mL in an internal pump. Due to the wide distribution to lack of studies – start with the lower of these peptidases it is not expected that dose range. Over the especially in patients with pre-existing first 24 hours, 39±16% of the administered renal impairment. Other risk factors dose is recovered in the urine, while the are: increasing age, repeated cycles remainder is principally bound to bone of bisphosphonates, concomitant tissue. Molecular weight 401 (443 as ● Antibacterials: increased risk of (daltons) acetate), (473.
Some degree of paravalvular regurgitation is a common finding after transcatheter aortic valve implantation (see Chapter 72) purchase keftab 250mg mastercard antibiotic resistance can come about by, but moderate or greater degrees appear to be associated with a worse prognosis (Fig buy genuine keftab on-line infections of the skin. Quantitation of prosthetic regurgitation may be challenging because jets frequently are highly eccentric and may be multiple generic keftab 750mg online antibiotic journal pdf, thus limiting the value of approaches based on jet dimensions. Assessment of paravalvular regurgitation in transcatheter or sutureless valves is particularly difficult because 70 multiple pinhole jets may be present. The quantitative Doppler approach using the pulmonic valve as the reference may also be helpful for aortic prostheses. Prosthetic tricuspid and pulmonic valves are much less common than their left-sided counterparts. In general, methods developed for assessment of the mitral and aortic valves are extrapolated to the tricuspid and pulmonic valves, although the evidence base for their use is less robust. Pericardial Disease Echocardiography is the imaging modality of choice for the identification of pericardial effusion and is an important tool in the diagnosis of tamponade and pericardial constriction (see Chapter 83). Pericardial Effusion Identification of pericardial effusion was one of the earliest applications of echocardiography. The diagnosis is made when an echo-free space separates the visceral and parietal pericardial echoes throughout the cardiac cycle, including diastole (Fig. In most cases the diagnosis of pericardial effusion is straightforward because the parietal pericardium is a strong echo reflector and the visceral pericardium is adherent to the epicardial surface of the heart. Although it is typically black, in some cases suboptimal image quality results in both blood pool and pericardial effusion with a grayish or intermediate echotexture. In such cases it may be difficult to differentiate a small pericardial effusion from epicardial fat, although the latter typically has a more reticulated inhomogeneous appearance than a fluid effusion. Note that the descending thoracic aorta (long arrow) is displaced from the heart by the pericardial effusion. With isolated pleural effusion, the descending aorta (Ao) remains immediately posterior to the heart. Differentiating features include displacement of the aorta from the heart by pericardial (but not pleural) fluid and extension of pleural (but not pericardial) fluid behind the left atrium (Fig. Of the two features, the relative position of the aorta is the most definitive because the position of the pericardial reflection is somewhat variable. It is therefore essential that sonographers routinely provide views that demonstrate the descending thoracic aorta and its position relative to the heart. Multiple windows—particularly the subcostal view, because fluid is gravity dependent and thus tends to collect inferiorly—are essential to rule out localized effusions. Sizing of pericardial effusions is typically somewhat subjective, with the terms trace, small, medium, and large being used. For reporting the size of effusions when longitudinal comparison will be important, it is helpful to report the maximal diameter of the effusion while noting the view(s) and time of the cardiac cycle (systole versus diastole) when the measurement is taken. Earlier estimates of the volume of the effusion, calculated using linear measures of pericardial and epicardial diameter, relied on a symmetric distribution of fluid and assumptions on the shape of the pericardial sac and heart. In a small case series, tracing pericardial and epicardial borders at end-diastole, and using the biplane Simpson method of discs instead to calculate the difference between the two volumes, has been shown to correlate much better with volumes drained by pericardiocentesis, underestimating the pericardial effusion by a 71 mean of 9%. Pericardial Hematoma Pericardial hematoma results from bleeding into the pericardial space and may be caused by bleeding along suture lines after open heart surgery, trauma, myocardial rupture, or aortic dissection or may occur as a complication of catheter-based or surgical intervention. Hematomas typically have an echotexture that is more coalescent and echodense than that of free fluid. When images are obtained in the acute setting, there may be evidence of both clot and free fluid (Fig. A subcostal view shows clotted (arrow) and free blood (black echotexture) within the pericardial space. Echocardiographic markers of cardiac tamponade fall into two categories: (1) cardiac chamber invagination reflecting elevated intrapericardial pressure and the resultant pressure gradients across the chamber walls and (2) echocardiographic markers of pulsus paradoxus, which reflect exaggerated respiratory variation in left-sided heart filling and ejection relative to that of the right side of the heart (ventricular interdependence). This sign is highly sensitive (100%) but may be present when hemodynamic disturbances are invasively detectable but fall below the threshold for the clinical diagnosis of tamponade, resulting in a specificity for clinical tamponade of 82%. Left atrial inversion as a marker of tamponade is rare and typically occurs in the setting of loculated effusions or those in which the pericardial reflection is relatively high and the left atrium is exposed to the effects of intrapericardial pressure. In this case, inversion, which is initiated in late ventricular diastole, has persisted well into ventricular systole. With pericardial hematoma in which no free blood is present, dynamic inversion of the chambers will not be observed, but the presence of fixed compression and underfilling of the cardiac chambers may be clues to the presence of tamponade physiology. There is an echocardiographic correlate to the clinical phenomenon of pulsus paradoxus. In the normal state, a slight increase (up to 17%) in flow velocities through the right heart occurs on inspiration, and a reciprocal but smaller decrease (up to 10%) in flow velocities through the left heart occurs during expiration. These tendencies are exaggerated when a tense, fluid-filled pericardium constrains the overall heart size and increases interdependence between the right and left ventricles. The most widely used signs are an exaggerated (>25%, and often >60% in frank tamponade) increase in the tricuspid inflow Doppler E wave peak velocities with a reciprocal decrease (of >30%) in the mitral E wave velocities (Fig. Additional signs of tamponade include the characteristic appearance of the heart oscillating or “swimming” in the pericardial fluid (see Video 14. Echocardiography may also be useful in guiding needle pericardiocentesis, particularly in the setting of loculated effusions. Imaging may help identify the best puncture site and angle of needle introduction, then confirm that the needle has entered the pericardial space. The latter is accomplished by the injection of a small amount of agitated saline, which will opacify the pericardial effusion with proper needle placement, but this will result in intracardiac contrast bubbles if the needle inadvertently penetrates the heart. Echocardiography is used to document the reduction in effusion size that should occur with successful drainage. Constrictive Pericarditis Pericardial constriction occurs when there is thickening, with or without calcification, of the pericardium that results in impaired cardiac diastolic filling, particularly during inspiration (Fig. The clinical features mimic those of biventricular heart failure, although the presence of a pericardial knock and Kussmaul sign (inspiratory increase in jugular venous pressure) should raise suspicion for constriction. When the pericardial space is expanded because of adhesions and fibrous tissue, the visceral and parietal pericardia are separated by tissue of variable echogenicity, unlike the echolucent appearance of pericardial effusion. Also, with effusion the parietal pericardial echo will be relatively stationary, whereas with pericardial thickening, visceral and parietal pericardial echoes will move in tandem. The bright posterior echo (white arrow) representing the parietal pericardium moves in parallel with the visceral pericardial/epicardial echoes (blue arrow), a finding indicative of adhesion between the two layers. If the pericardial space were expanded by free fluid (pericardial effusion), the parietal pericardial echo would be relatively stationary (compare with the M-mode inset of Fig. However, the two may be distinguished by tissue and color Doppler diastolic indices, as well as respirophasic effects on septal motion (interventricular interdependence and septal bounce) that are specific to constriction. Notably, the peak e′ of the lateral site may be smaller than that of the medial annulus, which is the opposite of the normal pattern; this phenomenon is termed annulus reversus and is believed to result from calcification and tethering effects of the pericardium on the lateral heart wall.
The chest radiograph reveals a normal cardiac silhouette until effusions are at least moderate in size order keftab us 027 infection. With larger effusions the anteroposterior cardiac silhouette assumes a rounded buy keftab with american express virus 4 pics 1 word, flask-like appearance (eFig 375 mg keftab amex antibiotics for uti most common. Lateral views may reveal the fat pad sign, a linear lucency between the chest wall and anterior surface of the heart resulting from separation of parietal pericardial fat from epicardium. A significant effusion appears as a lucent separation between the parietal and visceral pericardium for the entire cardiac cycle (Fig. Fluid then spreads anteriorly, laterally, and behind the left atrium, where it is limited by the visceral pericardial reflection. Circumferential effusions are graded as small (echo-free space in 3,4 diastole < 10 mm), moderate (10 to 20 mm), or large (> 20 mm). Because the rapidity of accumulation is critical, the hemodynamic significance of an effusion may not be closely correlated with its size. Frond-like or shaggy- appearing structures in the pericardial space detected by echocardiography suggest clots, chronic inflammation, or neoplastic pericardial processes. The cardiac chambers are small in tamponade and, as noted, the heart may swing anteroposteriorly (see Video 83. Distention of the inferior vena cava that does not diminish with inspiration is an important confirmatory finding. Doppler velocity recordings demonstrate exaggerated respiratory variation in right- and left-sided venous and valvular flow, with inspiratory increases on the right and decreases on the 3,4,36 left. These flow patterns are at least as sensitive for tamponade as M-mode and two-dimensional echocardiographic features. Top, systole; middle, early diastole with indentation indicated by arrow; bottom, late diastole with return of normal configuration. Fluoroscopy is useful in the cardiac catheterization laboratory for detection of procedure-related effusions when they cause damping or abolition of cardiac pulsation. They have a role when hemodynamics are atypical, other conditions complicate interpretation, the severity of tamponade is uncertain, or echocardiography is technically inadequate. Here, coexistent pulmonary hypertension reduces the accuracy of echocardiographic signs of tamponade. Attenuation similar to water suggests a transudative effusion; attenuation denser than water, a malignant effusion or bloody or purulent fluid; and attenuation less dense than water, a chylous effusion. Malignant effusions are associated with a thicker pericardium than benign 40 effusions. Management Management is dictated first and foremost by whether tamponade is already present or has a high chance 1,2,41 of developing (Table 83. Situations where tamponade is a near term threat include suspected bacterial (including tuberculous) pericarditis, hemopericardium, and any moderate to large effusion that is not thought to be chronic and/or is increasing in size. When tamponade is present or threatened, decision making requires urgency and a low threshold for pericardiocentesis (see Table 83. In the absence of actual or threatened tamponade, management can be more deliberative. Some have acute pericarditis with a small to moderate effusion detected as part of routine evaluation. Others do not have symptoms or signs of pericarditis or effusion but undergo echocardiography because of the presence of diseases known to involve the pericardium. The rest are asymptomatic and have effusions detected when tests are performed for reasons other than suspected pericardial disease (e. Determine if tamponade is present or threatened based on history, physical examination, echocardiogram. If tamponade is not present or threatened: If etiology is not apparent, consider diagnostic tests as for acute pericarditis. If tamponade is present or threatened: Urgent or emergent closed pericardiocentesis or careful monitoring if trial of medical treatment to reduce effusion is considered appropriate. In many cases of effusion where tamponade is neither present nor threatened, a cause will be evident or suggested based on the history and/or previous diagnostic tests. When a diagnosis is not clear, an assessment of specific causes should be undertaken, including the diagnostic tests recommended for acute pericarditis and anything else dictated by the clinical picture (e. Thus, a patient with severe heart failure and circulatory congestion with a small effusion does not need such testing, but patients with evidence of a systemic disease deserve very careful attention. In patients without actual or imminent tamponade, pericardiocentesis (closed or open with biopsy) can be undertaken for diagnostic purposes but is not always required. As discussed above, in many cases a diagnosis will either be obvious when the effusion is first noted or become evident as part of the initial investigations. Moreover, in this setting routine analysis of pericardial fluid has a low diagnostic 2,8,41 yield. In situations where pericardiocentesis is felt to be necessary for diagnostic purposes, consideration should be given to open drainage with biopsy. Otherwise healthy patients with large, asymptomatic effusions and no evidence of tamponade or a 2,41 specific cause are a special category. The effusions are by definition chronic and in general stable, but a minority (perhaps 20% to 30%) develop tamponade unpredictably. Moreover, after closed 2,41 pericardiocentesis the effusions may not reaccumulate. Thus, there is a rationale for pericardiocentesis following routine evaluation for specific etiologies as outlined above. Recurrence of this type of effusion after closed pericardiocentesis is considered an indication for 2,41 pericardiectomy or a pericardial window. With the exception of those who do not wish prolongation of life (mainly those with metastatic cancer), hospital admission and careful hemodynamic and echocardiographic monitoring are mandatory. The great majority of patients require pericardiocentesis to treat or prevent tamponade, but there are some exceptions. Patients with known inflammatory/autoimmune diseases can be treated similarly (there is no evidence that corticosteroids increase recurrence in these patients). Patients with suspected bacterial infections or hemopericardium with small effusions (< 10 mm) should be considered to have threatened tamponade because of the cause. These patients may be suitable for initial conservative management and careful monitoring because the risk of closed pericardiocentesis is increased with smaller effusions. Hemodynamic monitoring with a central venous or pulmonary artery catheter is often useful, especially in patients with threatened or mild tamponade in whom a decision is made to defer pericardiocentesis. Monitoring is also helpful after pericardiocentesis to assess reaccumulation and the presence of underlying constriction (see Fig. Insertion of a catheter in the central circulation should not be allowed to delay definitive therapy in critically ill patients. For the majority of patients in this category, urgent or emergent pericardiocentesis is indicated. Volume expansion and positive inotropes are temporizing measures and should not be allowed to substitute for or delay pericardiocentesis.