
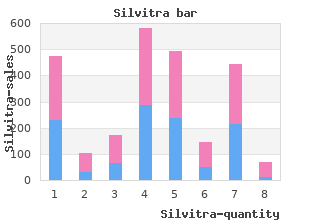
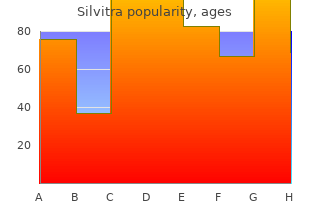
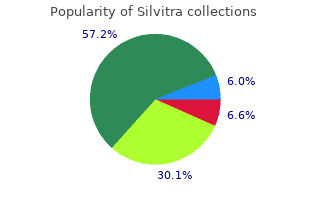
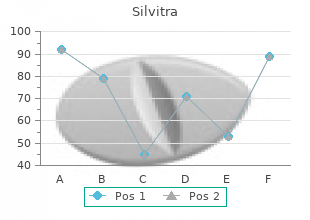
La Salle University. X. Avogadro, MD: "Order cheap Silvitra - Quality Silvitra OTC".
Embolism may result from the pump as a result of inadequate anticoagulation buy silvitra mastercard erectile dysfunction zocor, the cardiac chambers as a result of arrhythmias such as atrial fibrillation cheap silvitra 120 mg with visa impotence herbal remedies, or may arise from the native vasculature as a result of the patients’ preexisting vascular atherosclerosis cheap silvitra 120mg visa doctor's advice on erectile dysfunction. The overall incidence of ischemic stroke varies greatly by type of device; however, with the current generation devices, the rate is 0. An interrogation of device parameters to evaluate for signs of pump thrombosis or malfunction is warranted. This is a level of evidence C recommendation and needs to be individualized to each patient based on their degree of pulsatility. Blood pressure measurement can be challenging because of the markedly low pulse pressure that is often encountered. Doppler probes are the current clinical standard to measure blood pressure, and the opening Doppler pressure has been shown to correlate with the systolic blood pressure of patients with significant pulsatility to allow discrimination between a systolic and mean blood pressure. In other words, the Doppler opening pressure closely approximates the mean arterial pressure for patients with low pulsatility. The acute nature of many patients’ illness often precludes a detailed assessment of such issues, but devoted addressal of these issues in nonemergent situations is vital to achieving both optimal outcomes, clinically and programatically. Physical limitations that may impact the patient’s ability to care for the device such as the manual dexterity to change batteries or auditory acuity to hear alarms are important and practical considerations. Adequate cognitive ability is needed to understand the importance of the device and its components, the ability to troubleshoot problems, and recognize when to ask for assistance. The emotional ability to adapt to the device, its implications, potential limitations, and adverse events is also important for maximizing long-term outcomes and quality of life. Routine cognitive testing may use a screening metric such as the Montreal Cognitive Assessment test [105,106]. If a history of psychiatric illness is present, a thorough evaluation by the psychiatry service should be performed to identify risk factors as well as initiate and/or optimize therapy. Medical compliance and coping capacity must also be assessed, given that poor compliance and coping are associated with adverse outcomes. For those who received an intervention, such as revascularization, waiting to see the impact of this intervention on the patient’s clinical status is reasonable in the absence of further clinical deterioration. Many patients, however, will not have a readily identifiable or treatable proximate cause of their deterioration. Certain patients may be expected to have a short wait for transplantation based on their size, blood type, and level of sensitization, and the disadvantages of waiting for transplantation may be minimized. Today, a wide variety of devices are available for short-, medium-, and long-term support at numerous centers worldwide. Advances of pump technology are moving toward smaller pumps that still allow for full support, pumps that can be either implanted percutaneously or through minimally invasive surgeries, increased durability, totally implantable systems with transcutaneous energy transfer, and an improved device– patient interface. Research is also focused on improving biocompatibility, lowering risk of thrombosis, and better responsiveness to physiologic demands. Though the field is still hindered by adverse events and technological limitations, those too are improving. Further desirable advances include freedom from an external drive line, as well as alternative energy sources, such as transcutaneous energy. Moazami N, Fukamachi K, Kobayashi M, et al: Axial and centrifugal continuous-flow rotary pumps: a translation from pump mechanics to clinical practice. Krishan K, Nair A, Pinney S, et al: Liberal use of tricuspid-valve annuloplasty during left-ventricular assist device implantation. Kukucka M, Stepanenko A, Potapov E, et al: Right-to-left ventricular end-diastolic diameter ratio and prediction of right ventricular failure with continuous-flow left ventricular assist devices. Dandel M, Potapov E, Krabatsch T, et al: Load dependency of right ventricular performance is a major factor to be considered in decision making before ventricular assist device implantation. Vieillard-Baron A, Jardin F: Why protect the right ventricle in patients with acute respiratory distress syndrome? John R, Mantz K, Eckman P, et al: Aortic valve pathophysiology during left ventricular assist device support. Butler J, Geisberg C, Howser R, et al: Relationship between renal function and left ventricular assist device use. Crow S, John R, Boyle A, et al: Gastrointestinal bleeding rates in recipients of nonpulsatile and pulsatile left ventricular assist devices. Geisen U, Heilmann C, Beyersdorf F, et al: Non-surgical bleeding in patients with ventricular assist devices could be explained by acquired von Willebrand disease. Crow S, Chen D, Milano C, et al: Acquired von Willebrand syndrome in continuous-flow ventricular assist device recipients. Mano A, Fujita K, Uenomachi K, et al: Body mass index is a useful predictor of prognosis after left ventricular assist system implantation. Holtz J, Teuteberg J: Management of aortic insufficiency in the continuous flow left ventricular assist device population. A National Heart, Lung, and Blood Institute perspective based on data from the Interagency Registry for Mechanically Assisted Circulatory Support. In comparison, the coexistence of two opposing primary acid–base disturbances, such as a metabolic acidosis as a result of diarrhea with metabolic alkalosis as a result of vomiting, may result in little or no deviation of the blood pH from normal. Inability to accomplish this results in metabolic acidosis (proximal, type 2, renal tubular acidosis) (see text for details). The kidney must also excrete + the 50 to 100 mEq per kg of H generated each day from the metabolism of dietary proteins, particularly sulfur-containing amino acids (i. To offset this limitation, urinary buffers present in the urine maintain the urine pH above this critical value, permitting ongoing excretion of the daily acid load. By comparison, the most important urinary buffer is ammonia, because the abundance of this buffer can be varied according to physiologic needs. Ammonia synthesis occurs in the proximal tubule, derived principally from the breakdown of glutamine to α-ketoglutarate. This process is stimulated by intracellular acidosis and by hypokalemia, both of which act by decreasing the intracellular pH (see the following discussion). The latter is particularly important because acidosis stimulates the breakdown of glutamine to ammonia. By comparison, hyperkalemia impairs the capacity of the proximal tubule to make ammonia, thus contributing to the metabolic acidosis observed in hyperkalemic disorders. These unmeasured anions consist of proteins (primarily albumin), sulfates, phosphates, and circulating organic acids. If, however, there is differential tubular dysfunction, the excretion of acid is diminished, but excretion of sulfate may be maintained owing to reduced reabsorption. Typically, the plasma bicarbonate concentration is greater than 12 mEq per L in patients with uncomplicated chronic kidney disease. Lactic Acidosis Lactic acidosis is the most common cause of severe metabolic acidosis encountered in the intensive care unit. Lactate levels greater than 5 mmol per L are considered diagnostic of lactic acidosis, although levels between 2 and 5 mmol per L may be significant in the appropriate clinical circumstances. D-Lactate, generated by intestinal bacteria, is not detected by the usual lactate assay, and a specific enzymatic assay must be requested to diagnose this disorder. Ketoacidosis Ketoacidosis occurs when acetoacetic acid and β-hydroxybutyric acid are overproduced by the liver (for a complete discussion, see Chapter 137). Sodium-glucose cotransporter-2 inhibitors, used in the treatment of type 2 diabetes, may increase the risk of ketoacidosis.
Treatment is with antidandruff shampoos containing selenium sulfide discount silvitra 120 mg fast delivery erectile dysfunction quran, zinc pyrithione cheap 120 mg silvitra free shipping erectile dysfunction natural cure, ketoconazole order silvitra cheap impotence grounds for annulment philippines, or ciclopirox and topical antifungals (ketoconazole cream, etc. It is caused by blockage of eccrine sweat ducts that occurs in the setting of fever and excessive sweating, often in patients who are largely confined to bed. It occurs in three main forms: miliaria crystallina, which presents as tiny clear asymptomatic superficial vesicles on the trunk, head, and neck; miliaria rubra, which presents as uniform, small pruritic erythematous papules on the trunk, neck, and flexural extremities. It is important to be able to recognize miliaria to distinguish it from more medically significant entities such as disseminated herpes simplex, varicella, or candidiasis. The distribution of miliaria in areas where the skin is occluded and where excessive sweating occurs is helpful for the diagnosis. Some reports state that oral ascorbic acid and topical lanolin can be helpful, but no controlled trials have been done [158]. Tinea corporis is the common, superficial fungal infection found on any area of the skin excluding the palms, soles, scalp, and groin. Trichophyton rubrum is the most common causative organism, although any dermatophyte may be responsible. Tinea corporis presents as one or multiple annular lesions with erythematous scaly borders that exhibit centrifugal spread and leave a central clearing. Other clinical presentations include tinea profunda, which exhibits a granulomatous or verrucous appearance due to an excessive host inflammatory response, and Majocchi’s granuloma, which presents as follicular-based pustules or papules. The differential diagnosis includes nummular eczema, subacute cutaneous lupus erythematosus, and granuloma annulare. Limited disease may be treated with topical agents such as naftifine 1% cream, terbinafine 1% cream, or clotrimazole 1% cream applied twice daily for 2 to 4 weeks in combination with a topical steroid if there is significant local inflammation [159]. More extensive or recalcitrant disease may require systemic treatment such as itraconazole 100 mg daily or terbinafine 250 mg daily for 2 weeks. Prognosis is excellent with 70% to 100% cure after treatment, but recurrence is common [160], especially among the immunosuppressed. Scabies Scabies is a common, extremely pruritic dermatosis caused by infestation with the mite, Sarcoptes scabiei. It spreads from person to person through direct skin contact, although it can rarely spread through fomites such as bedding or towels. Scabies should be considered in the differential diagnosis of any patient with severe generalized itching, especially if they have had contact with residential institutions such as nursing homes, where it may be endemic. Patients with scabies present with severe generalized pruritus, sparing the head and neck, which is worse at night. Papules, pustules, vesicles, and nodules may also occur, the last being especially common in children. Immunocompromised and neurologically impaired patients may present with the crusted or “Norwegian” variant of scabies, in which the skin is markedly thickened and crusted. Definitive diagnosis of scabies is made by observing skin scrapings microscopically for mites, eggs, or mite feces. First-line treatment of scabies is with topical 5% permethrin cream applied from neck down and left on overnight, with special attention to the genitalia, web spaces, and under the fingernails. All household members or suspected contacts over the age of 2 months and nonpregnant individuals should be treated simultaneously. When topical treatment is impractical, oral ivermectin may be given as a single dose of 200 µg per kg of body weight, repeated in 1 week. Patients can be concurrently treated with topical corticosteroids and oral antihistamines to help alleviate itch [161]. Introduction, history, classification, clinical features, systemic manifestations, etiology, and aimmunopathogenesis. Mockenhaupt M, Viboud C, Dunant A, et al: Stevens–Johnson syndrome and toxic epidermal necrolysis: assessment of medication risks with emphasis on recently marketed drugs. Araki Y, Sotozono C, Inatomi T, et al: Successful treatment of Stevens– Johnson syndrome with steroid pulse therapy at disease onset. Walsh S, Diaz-Cano S, Higgins E, et al: Drug reaction with eosinophilia and systemic symptoms: is cutaneous phenotype a prognostic marker for outcome? Leclerc-Mercier S, Bodemer C, Bourdon-Lanoy E, et al: Early skin biopsy is helpful for the diagnosis and management of neonatal and infantile erythrodermas. Friederichs J, Torka S, Militz M, et al: Necrotizing soft tissue infections after injection therapy: higher mortality and worse outcome compared to other entry mechanisms. Su Y, Chen H, Hong U, et al: Laboratory risk indicator for necrotizing fasciitis score and the outcomes. Chams-Davatchi C, Esmaili N, Daneshpahooh M, et al: Randomized controlled open-label trial of four treatment regimens for pemphigus vulgaris. Beissert S, Werfel T, Frieling U, et al: A comparison of oral methylprednisolone plus azathioprine or mycophenolate mofetil for the treatment of pemphigus. Amagai M, Ikeda S, Shimizu H, et al: A randomized double-blind trial of intravenous immunoglobulin for pemphigus. Ingen-Housz-Oro S, Valeyrie-Allanore L, Cosnes A, et al: First-line treatment of pemphigus vulgaris with a combination of rituximab and high-potency topical corticosteroids. Sagi L, Baum S, Agmon-Levin N, et al: Autoimmune bullous diseases the spectrum of infectious agent antibodies and review of the literature. Gast T, Kowal-Vern A, An G, et al: Purpura fulminans in an adult patient with Haemophilus influenzae sepsis: case report and review of the literature. Terrier B, Krastinova E, Marie I, et al: Management of noninfectious mixed cryoglobulinemia vasculitis: data from 242 cases included in the CryoVas survey. Huang J, Pol-Rodriguez M, Silvers D, et al: Acquired ichthyosis as a manifestation of acute cutaneous graft-versus-host disease. A nutritional formula enriched with arginine, zinc, and antioxidants for the healing of pressure ulcers: a randomized trial. Dessinioti C, Katsambas A: Seborrheic dermatitis: etiology, risk factors, and treatments: facts and controversies. Pathophysiology As homeothermic organisms, humans must regulate their temperature to maintain fundamental biologic processes [2]. Fever is the result of an upward adjustment in the thermoregulatory set point involving cytokine-mediated rise in core temperature, generation of acute-phase reactants, and activation of numerous physiologic, endocrinologic, and immunologic systems [5]. In contrast, simple heat illness or malignant hyperthermia is an unregulated rise in body temperature caused by inability to eliminate heat adequately [4]. Physiologically, fever begins with the production of one or more proinflammatory cytokines in response to exogenous pyrogenic substances (such as microorganisms and toxic agents) or immunologic mediators. Measurement the Society of Critical Care Medicine and the Infectious Disease Society of America issued a consensus statement recommending that core temperature of higher than 38. Although the pulmonary artery catheter has been considered the gold standard measurement technique, in most situations, relatively small differences exist between the other commonly used methods [7]. The major causes of abnormally elevated temperatures in critically ill patients can be broadly classified as infectious fevers, noninfectious fevers, and hyperthermia syndromes (Table 71. Fever may appear in the patient in whom the stress of surgery unmasks adrenal insufficiency or following bilateral adrenal hemorrhage in patients with a history of thromboembolic disease, recent surgery, and/or anticoagulant therapy [11].
A single large scale randomized clinical trial of pulmonary artery catheterization in high-risk surgical patients demonstrated no improvement of survival [45] discount silvitra 120mg online erectile dysfunction after zoloft. Practice guidelines for intraoperative hemodynamic monitoring published by the American Society of Anesthesiologists consider the severity of the patient’s underlying cardiovascular disease generic 120mg silvitra visa erectile dysfunction treatment levitra, the type of surgical procedure order 120 mg silvitra with mastercard erectile dysfunction treatment new delhi, and the likelihood of major hemodynamic lability [46]. An intra-aortic balloon pump can increase cardiac output and improve diastolic coronary artery filling. Short-term support is well tolerated with the newer devices, but in-hospital mortality remains high [49]. The potential adverse effects of atrial fibrillation include loss of atrioventricular synchrony, rapid or inappropriately slow ventricular response rates, variable diastolic filling times, and thromboembolic complications. Patients with a known history of chronic atrial fibrillation should have adequate heart rate control and anticoagulation whenever feasible (see below). Uncontrolled, sustained, rapid (>120 beats per minute) atrial fibrillation can result in a reversible dilated cardiomyopathy or, more typically, can worsen preexisting left ventricular systolic dysfunction [50]. A large recent registry analysis found no increase of mortality risk by treating new-onset atrial fibrillation of heart failure patients [50]. For all patients, thyroid function should be assessed to exclude hyperthyroidism as a contributing factor. For patients who experience active angina pectoris or hemodynamic instability during rapid atrial fibrillation, urgent synchronized cardioversion should be performed followed by initiation of an atrial stabilizing agent to prevent recurrence. Amiodarone is particularly well tolerated from a hemodynamic standpoint; the loading dose of amiodarone should be kept below 1,000 mg per day to prevent further exacerbation of heart failure symptoms. Dronedarone, a non- iodinated derivative of amiodarone, has also been shown to be effective for maintenance of sinus rhythm and rate control for rapid atrial fibrillation. It is highly effective for restoring sinus rhythm but has been associated with torsades de pointes in up to 3% of patients [51]. Asymptomatic ventricular ectopy should be viewed as a marker of disease severity rather than a specific marker for sudden cardiac death risk [53]. It should be reactivated and its function checked by an electrophysiologist in the early perioperative period. Anticoagulation Systemic anticoagulation is often a part of a heart failure patient’s outpatient management. Studies have suggested that the risk of thromboembolic complications is lower than previously expected, averaging 1. Current indications for systemic anticoagulation include paroxysmal or chronic atrial fibrillation, a history of thromboembolism, or echocardiographically documented left ventricular thrombus [55,56]. Relative indications include a markedly dilated left ventricle (>75 mm) with severe systolic dysfunction and spontaneous echocardiographic contrast (“smoke”), indicating sluggish intracavitary blood flow. If surgery or central venous catheter placement are required, warfarin can be reversed with vitamin K or fresh frozen plasma, agent specific reversal of selected non–vitamin K antagonist can be accomplished, and transiently substituted with intravenous heparin or subcutaneous low-molecular weight heparin as feasible. Meticulous attention to volume status and maintenance of appropriate vasodilator therapy and β-adrenergic blockade form the cornerstones of acute management. Patients with refractory symptoms or recent decompensation may require hemodynamic monitoring via a pulmonary artery catheter, and initiation of short-term vasoactive therapy including nitroprusside, nitroglycerin, milrinone, or dobutamine. Maintenance of sinus rhythm should be considered, and pharmacological suppression of recurrent ventricular tachyarrhythmias is often necessary. With careful management, hospital morbidity and mortality can be minimized despite the presence of advanced symptomatic heart failure. Kazury A, Elkayam U: Cardiorenal interactions in acute decompensated heart failure: contemporary concepts facing emerging controversies. Aronson D, Darawsha W, Atamna A, et al: Pulmonary hypertension, right ventricular function, and clinical outcome in acute decompensated heart failure. Metra M, Davison B, Bettari L, et al: Is worsening renal function an ominous prognostic sign in patient with acute heart failure? A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Logeart D, Thabut G, Jourdain P, et al: Predischarge B-type natriuretic peptide assay for identifying patients at high risk of re-admission after decompensated heart failure. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Practice Guidelines for Pulmonary Artery Catheterization: An updated report of the American Society of Anesthesiologists Task Force on Pulmonary Artery Catheterization. Seyfarth M, Sibbing D, Bauer I, et al: A randomized clinical trial to evaluate the safety and efficacy of a percutaneous left ventricular assist device versus intra-aortic balloon pumping for treatment of cardiogenic shock caused by myocardial infarction. Similarly, owing to a lack of data, the guidelines do not provide definitive recommendations regarding other hemodynamic measures. Patients were randomized to either cooling to a temperature between 32°C and 34°C over 12 to 24 hours, or no temperature management at all. Both trials demonstrated significantly improved outcomes, with very low numbers needed to treat (roughly 6) for both improved survival and neurologic outcomes [32]. At 6 month follow-up, there was no difference in mortality (50% for the 33°C group versus 48% for the 36°C group, p = 0. The similar outcomes between treatment strategies were observed for all important subgroups of patients (e. As a result, the current guidelines recommend against the routine initiation of prehospital cooling with cold fluids. A subsequent smaller pilot study demonstrated improved outcomes associated with 32°C versus 34°C [38], suggesting that lower temperatures might be better. Although there was no difference in outcomes between these two treatment groups, it is crucial to remember that this was a trial of two active temperature management interventions (33°C versus 36°C). The temperature range in the guideline recognizes uncertainty regarding the hypothesis that some individuals may benefit from greater degrees of hypothermia, whereas others may be at an increased risk of complications at lower temperatures (such as bradycardia), and thus can be effectively treated at a more moderate target temperature. Alternative methods have included surface cooling methods such as blankets and gel pads with circulating cold water. Although there is data demonstrating different rates of achieving and maintaining target temperature, no particular method has been associated with better outcomes than the others. Shivering slows the time to target temperature and increases metabolic activity, so it should be treated aggressively. There are varying approaches to the use of neuromuscular blockade (selective versus continuous), which are currently being evaluated in ongoing clinical trials. If a patient is not cooling at a rate of 1°C per hour, then an empiric bolus of a neuromuscular blockade may help reduce subclinical shivering and achieve the target temperature more quickly. Nonconvulsive status epilepticus is a potential reason for patients not to regain consciousness and can be associated with secondary brain injury. In addition to potentially further injuring the brain, seizure activity also carries a poor prognosis. Ventilation and Oxygenation Management of mechanical ventilation is an important component of post-arrest care. Hypocapnia has been associated with decreased cerebral perfusion [25] and worse outcomes in observational studies [41,42]. Similarly, oxygenation should be targeted within a range to avoid episodes of hypoxia (PaO less than 60 mm Hg)2 as well as hyperoxia (PaO greater than 300 mm Hg), with current2 recommendations to titrate FiO to maintain oxygen saturation greater2 than 94% [3]. Hypergylcemia Hypothermia decreases pancreatic insulin secretion and increases insulin resistance, leading to hyperglycemia [26].
When using a Minnesota tube buy silvitra pills in toronto erectile dysfunction treatment lloyds pharmacy, the esophageal aspiration port should be set to continuous suction and the tube generously lubricated with lidocaine jelly prior to inserting it through the nose or mouth into the stomach discount 120mg silvitra visa impotence vacuum treatment. Auscultation in the epigastrium while air is injected through the gastric lumen verifies the position of the tube buy silvitra 120mg on-line erectile dysfunction walmart, but the position of the gastric balloon must be confirmed at this time radiologically or by ultrasound if it is more expedient [33], because high placement can lead to esophageal rupture and low placement to duodenal rupture [34]. The manometer is then connected to the gastric pressure port and the gastric balloon is inflated with no more than 80 mL of air. A (portable) radiograph or ultrasound must be obtained that includes the upper abdomen and lower chest (s. When it is documented that the gastric balloon is below the diaphragm, it should be further inflated with air in 100 mL aliquots to a volume of 250 to 300 mL. If the change of manometric pressure for an aliquot is more than 15 mm Hg of the preinsertion pressure or if the gastric balloon is underinflated causing upward migration, erroneous esophageal placement should be considered. Hemorrhage is frequently controlled with insufflation of the gastric balloon alone without applying traction, but for patients with torrential hemorrhage, it is necessary to apply traction (vide infra). If the bleeding continues, the manometer attached to the esophageal pressure port is used to inflate the esophageal balloon to a pressure of approximately 45 mm Hg. When there is still bleeding, deflate the esophageal balloon, apply more traction, and reinflate in the event that it is a gastric variceal bleed. Ultrasonography for Tube Insertion Although a confirmatory radiograph is still warranted to document the final position of the inflated gastric balloon, an advantage to ultrasonography is that it can be used real time during insertion at the bedside of the patient [33,36]. If the tube is not easily visible, injection of 50 mL of air into the gastric lumen of the tube will yield a characteristic pattern of air bubbles within the stomach. Once the tube is confirmed to be within the stomach, the operator slowly injects air into the gastric balloon. The inflated gastric balloon is visualized as a distinct structure within the stomach that has an echogenic curvilinear surface and that generates a strong acoustic shadow (Chapter 22 Video 22. Fixation and Traction Techniques Fixation of the tube, and traction on the tube depend on the route of insertion. When the nasal route is used, attachment of a sponge rubber cuff around the tube at the nostril prevents skin and cartilage necrosis. When traction is required, the tube should be attached to a cord that is passed over a catcher’s mask for maximum transportability [37] or a pulley in a bed with an overhead orthopedic frame and aligned directly as it comes out of the nose to avoid contact with the nostril. When the tube is inserted through the mouth, traction is better applied by placing a football or hockey helmet on the patient and attaching the tube to the face mask of the helmet after a similar weight is applied for tension. Pressure sores can occur on the head and forehead if the helmet does not fit properly or if it is used for a prolonged period. To reduce encephalopathy, the gastric aspiration port should be used to thoroughly lavage the stomach before being set to low intermittent suction. The esophageal port may be set to intermittent or continuous suction, depending on the extent of bleeding and drainage [35]. Tautness and inflation should be checked often and at least 1 hour after insertion, allowing for only transient fluctuations of as much as 30 mm Hg with respirations and esophageal spasm. The tube is left in place a minimum of 24 hours with gastric balloon tamponade maintained continuously for up to 48 hours. The esophageal balloon should be deflated for 5 minutes every 6 hours to help prevent mucosal ischemia and esophageal necrosis. Radiographic assurance of correct placement should be obtained every 24 hours and when dislodgement is suspected. A pair of scissors should be kept with the apparatus in case rapid decompression becomes necessary, because balloon migration can acutely obstruct the airway or rupture the esophagus. It is advisable to take care not to utilize bare hemostats and to clamp at the thicker portion of the ports, because it is possible for the lumen to become obliterated and the tube thus impacted [40]. The gastric balloon is left inflated for an additional 24 to 48 hours and may be deflated when there is no evidence of bleeding. Primary therapy and secondary prophylaxis, as described previously, should be considered because balloon tamponade is a bridge intervention and rebleeding occurs in up to two-thirds of patients within 3 months without therapy [3]. Aspiration pneumonia is the most common complication of balloon tamponade with incidence ranging from 0% to 12%. Acute laryngeal obstruction and tracheal rupture are the most severe of all complications, and the worst examples of tube migration or malpositioning. Migration of the tube occurs when the gastric balloon is not inflated properly after adequate positioning in the stomach or when excessive traction (>1. Mucosal ulceration of the gastroesophageal junction is common and is directly related to prolonged traction times (>36 hours). Perforation of the esophagus has been reported as a result of misplacing the gastric balloon above the diaphragm. Zehetner J, Shamiyeh A, Wayand W, et al: Results of a new method to stop acute bleeding from esophageal varices; implantation of a self- expanding stent. El Sayed G, Tarf S, O’Beirne J, et al: Endoscopy management algorithms: role of cyanoacrylate glue injection and self-expanding metal stents in acute variceal haemorrhage. Avgerinos A, Armonis A, Manolakpoulos S, et al: Endoscopic sclerotherapy versus variceal ligation in the long-term management of patients with cirrhosis after variceal bleeding: a prospective randomized study. Kitamoto M, Imamura M, Kamada K, et al: Balloon-occluded retrograde transvenous obliteration of gastric fundal varices with hemorrhage. Shiba M, Higuchi K, Nakamura K, et al: Efficacy and safety of balloon- occluded endoscopic injection sclerotherapy as a prophylactic treatment for high-risk gastric fundal varices: a prospective, randomized, comparative clinical trial. Pohl J, Pollmann K, Sauer P, et al: Antibiotic prophylaxis after variceal hemorrhage reduces incidence of early rebleeding. Bard, Inc: Bard Minnesota four lumen esophagogastric tamponade tube for the control of bleeding from esophageal varices [package insert], 1997. Pinto-Marques P, Romaozinho J, Ferreira M, et al: Esophageal perforation-associated risk with balloon tamponade after endoscopic therapy. Lock G, Reng M, Messman H, et al: Inflation and positioning of the gastric balloon of a Sengstaken-Blakemore tube under ultrasonographic control. Isaacs K, Levinson S: Insertion of the Minnesota tube, in Drossman D (ed): Manual of Gastroenterologic Procedures. Lin A C-M, Hsu Y-H, Wang T-L, et al: Placement confirmation of Sengstaken-Blakemore tube by ultrasound. Kashiwagi H, Shikano S, Yamamoto O, et al: Technique for positioning the Sengstaken-Blakemore tube as comfortably as possible. As a diagnostic intervention, abdominal paracentesis with removal of 20 mL of peritoneal fluid is performed to determine the etiology of the ascites or to ascertain whether infection is present, as in spontaneous bacterial peritonitis [1]. It can also be used in any clinical situation in which the analysis of a sample of peritoneal fluid might be useful in ascertaining a diagnosis or guiding therapy. Ascites is the most common presentation of decompensated cirrhosis, and its development heralds a poor prognosis, with a 50% 2-year survival rate. Refractory ascites occurs in 10% of patients with cirrhosis and is associated with substantial morbidity and a 1-year survival of less than 50% [4,5]. Techniques Before abdominal paracentesis is initiated, a catheter may be inserted to drain the urinary bladder, and correction of any underlying coagulopathy or thrombocytopenia should be considered. A consensus statement from the International Ascites Club states that “there are no data to support the correction of mild coagulopathy with blood products prior to therapeutic paracentesis, but caution is needed when severe thrombocytopenia is present” [3]. But in critically ill patients, there is still uncertainty as to the optimal platelet count and prothrombin time for the safe conduct of paracentesis.
Cryptococcal or Listeria meningitis is the most urgent diagnosis purchase online silvitra sublingual erectile dysfunction pills, and these illnesses require immediate treatment order silvitra with paypal erectile dysfunction doctors minneapolis. An inflamed central line may be treated presumptively for gram-positive infection buy silvitra cheap erectile dysfunction alcohol. If a chest radiograph is abnormal, and if the patient is producing sputum, a sample should be obtained for culture and for Gram, acid-fast, and silver staining. If no sputum is being produced, urgent pulmonary and infectious diseases consultations for a diagnostic evaluation should be requested. Because the number of possible causes of pulmonary infection is so large in this population, empiric therapy is not recommended (unless respiratory failure has begun). If the patient is febrile, but none of the foregoing tests has yielded a diagnosis, an infectious diseases consultation should be sought. The possible entities causing fever in the setting of a negative initial evaluation are so diverse that much time and many resources can easily be wasted. Although the approach outlined above is most applicable to the transplant population, clinicians must not forget that people receiving corticosteroids represent the greatest number of immunosuppressed patients. Much debate has occurred concerning the lowest dosage of corticosteroid that will predispose to infection. A useful general rule is to assume that any dose above physiologic maintenance may be immunosuppressive. Doses as low as 10 mg daily of prednisone have led to invasive pulmonary aspergillosis. Therefore, when faced with a febrile non-transplant patient on corticosteroids for an inflammatory disorder, the diagnostic points discussed in this subsection should be kept in mind. Also, because immunosuppressive agents may blunt an inflammatory response, clinicians should consider that even low-grade fever may indicate the presence of a serious infection. Prevention Given the long-term nature of immunosuppression in graft recipients, preventive measures play a critical role in preventing morbidity and mortality. The recommended preventive measures can be categorized by pathogen type: • Bacteria. In the patient with a documented reduction in IgG level below 400 mg/dL, intravenous IgG may be given to prevent sinus and pulmonary infections resulting from S. If these tests are positive, the patient should be treated with intravenous ganciclovir 5 mg/kg twice daily for 14-21 days or oral valganciclovir 900 mg twice during the first 24 hours for induction, and then 900 mg daily. Antiherpes simplex IgG titers should be measured in all potential recipients before transplantation. Emergent management is required for a) central nervous system symptoms such as headache and confusion— consider Cryptococcus and Listeria. Other transplant patients undergoing high-level immunosuppression should also be considered for prophylaxis. Reactivation of varicella virus can lead to serious morbidity and also requires preventive measures. The recipient and all family members should be vaccinated with the live attenuated vaccine at least 4 weeks before the transplant procedure. Allogeneic bone marrow transplant patients have a high incidence of Candida albicans infection during phase I and should receive oral fluconazole 400 mg daily or posaconazole (200 mg three times daily) for prophylaxis. Throughout the period of immunosuppression, transplant patients are at risk of infection with this organism, and oral trimethoprim–sulfamethoxazole (one double-strength tablet three times weekly, or one single-strength tablet daily) is recommended. Bone marrow recipients with positive IgG titer for herpes simplex virus should receive valacyclovir. Vaccine for varicella virus should be given to patients and household contacts before a transplantation procedure. Allogeneic transplant patients should receive fluconazole or posaconazole to prevent fungal infections. All transplant recipients should receive trimethoprim- sulfamethoxazole to prevent Pneumo-cystis infection. These patients fit into two general categories that predispose them to infections that are usually controlled either by neutrophils or by T cells. Bone marrow or stem cell transplant patients fit into both categories depending on how much time has passed since transplantation. The febrile neutropenic patient can be considered to be a medical emergency requiring empiric antibacterial therapy with one or two broad-spectrum antibiotics. Conversely, the patient with suppression of cell-mediated immunity requires a thorough evaluation, and empiric antibiotic therapy should be avoided unless the cause of the fever is known on presentation. It is advisable that these patients receive care from infectious disease specialists. Outpatient management of these patients can be expected to become increasingly common. Levofloxacin to prevent bacterial infection in patients with cancer and neutropenia. British Society for Medical Mycology proposed standards of care for patients with invasive fungal infections. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis: An official publication of the Infectious Diseases Society of America. Risks and outcomes of invasive fungal infections in recipients of allogeneic hematopoietic stem cell transplants after nonmyeloablative conditioning. Myelosuppression and serotonin syndrome associated with concurrent use of linezolid and selective serotonin reuptake inhibitors in bone marrow transplant recipients. Efficacy and safety of linezolid compared with vancomycin in a randomized, double-blind study of febrile neutropenic patients with cancer. Meta-analysis: the efficacy of strategies to prevent organ disease by cytomegalo-virus in solid organ transplant recipients. Infliximab use in patients with severe graft-versus-host disease and other emerging risk factors of non-Candida invasive fungal infections in allogeneic hematopoietic stem cell transplant recipients: a cohort study. Strategy of following voriconazole versus amphotericin B therapy with other licensed antifungal therapy for primary treatment of invasive aspergillosis: impact of other therapies on outcome. Treatment of febrile neutropenic patients with cancer who require hospitalization: a prospective randomized study comparing imipenem and cefepime. Once daily, oral, outpatient quinolone monotherapy for low-risk cancer patients with fever and neutropenia: a pilot study of 40 patients based on validated risk-prediction rules. Prevention and early treatment of invasive fungal infection in patients with cancer and neutropenia and in stem cell transplant recipients in the era of newer broad-spectrum antifungal agents and diagnostic adjuncts. Role of glycopeptides as part of initial empirical treatment of febrile neutropenic patients: a meta-analysis of randomised controlled trials. Infections in patients with febrile neutropenia: epidemiology, microbiology, and risk stratification. Voriconazole compared with liposomal amphotericin B for empirical antifungal therapy in patients with neutropenia and persistent fever.
Cheap silvitra on line. Come effettuare un corretto lavaggio nasale al vostro Bimbo.