
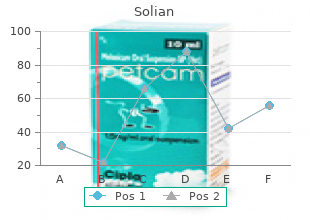
University of Southern California. O. Marlo, MD: "Buy online Solian - Discount Solian OTC".
Neither medicine nor anything else can take death buy generic solian canada symptoms heart attack, disease and suffering away from individuals and therefore from the species generic solian 100 mg with amex medications zopiclone; perhaps it is time to acknowl- edge the fact discount solian 50 mg without prescription 4 medications at walmart. Medical sociologists have observed the medical profession from the outside for a long time, and their commentaries have been so uncomplimentary that none of them is likely to appear in the curricula of medical schools. In the Old Testament, physicians are mentioned twice: once as servants good at embalming (Genesis 50. The noble aspirations of medicine have for ever been hampered by impotence and ignorance. Leaving aside some useful surgical techniques developed centuries ago, only at the beginning of this century was the balance of benefit versus harm tipped in favour of attending a doctor. He feared them, because in his experience people were more likely to get worse after the doctor called. He also noticed that doctors were neither happier nor lived longer than their patients. And to tell the truth, of all this diversity and confusion of prescriptions, what other purpose and effect is there after all than to empty the bowels, which a thousand domestic 20 simples can do? Nicocles, an ancient Greek poet, called physicians a happy 24 Healthism race, because the sun shone on their successes and the earth hid all their failures. They made the terrible mistake of not being even more secretive and not keeping a unified front, For the result of this mistake is that when their irresolution, the weakness of their arguments, divinations and grounds, the bitterness of their contestations, full of hatred, jeal- ousy, and self-consideration, come to be revealed to every- one, a man would have to be preternaturally blind not to feel that he runs a great risk in their hands. But to the credit of the medical profession there were always renegades and traitors within the ranks. The editor of The Lancet, Thomas Wakley, in 1825, freely admitted that If patients are content with the medical treatment, what- ever it may be, it is a proof of their ignorance, and nothing more. That some patients in hospital may properly be treated we do not deny, but that others are killed, we as 24 positively assert. For this he blamed human nature: man is a most gullible animal and the temptation is too great not to make capital out of it. Jokes about the follies of medicine have a different func- tion when uttered by a layman rather than by a professional. In the first case their purpose is to cut doctors down to size and demystify their art. In the second case, the levity is part of private medical humour, a sort of cynical defence mechanism enabling the doctor to cope with the stress of his task. When in 1889, the President of the British Medical Association washed medical dirty linen in public, he was reprimanded by 21 the editor of the Provincial Medical Journal. In the same editorial, however, an account was given of a private medical function of the British Medical Association, at which the speaker related an anecdote greatly appreciated by the com- pany. Shaw compared doctors to tradesmen and shopkeepers,with a pecuniary interest in people being ill. Sir Clifford Allbutt, one of the most prominent representatives of the profession at that time, said: I think we shall all agree that Mr Bernard Shaw when he takes up his sword certainly slashes down to the quick, and I think that we must admit at that quick there is a great deal of truth to be found, and expressed with a great deal of gentleness towards our profession. Compare the politeness and gentility of that generation of physicians with the hysterical outbursts of our contempor- aries when a layman, such as Illich, dares to raise a question or two about the direction of medicine today. Shaw elabor- ated on his views on medicine in his Preface on Doctors, published with The Doctors Dilemma in 1911. His own health philosophy was summed up in these sentences: - Do not try to live for ever. When comparing medicine then and now, the main differ- ence is between a profession and a trade, between a vocation which grew up in the humanist tradition and the medico- industrial complex governed by monetary gain and political 28 Healthism interests. The change was so slow that only a few shrewd observers, such as Illich, noticed it. Then economists came up with a bizarre theory, which has become widely accepted, according to which the basis of a sound economy is a continual increase in the con- sumption (that is, waste) of goods. To arouse an interest in new goods, it is important to adver- tise and to convince potential customers that they could not possibly be without them, even though they may not have realised it up until now. Once the need becomes universal, production can be defended by pointing out that it meets a need. As health services become increasingly complex, a third party interposes between the doctor and the patient - the health manager. Managers control the purchase of technol- ogy, its marketing and advertising, so that new markets can be created. Some $10 billion a year is spent on slimming (pills, books, clubs, 30 Healthism special diets). The healthy must be persuaded that feeling healthy is not the same as being healthy, otherwise they could go through their whole life without noticing how bad they were. Once healthy, but scared, health consumers start queu- ing outside, demanding their right to be let in (since health, as they were told and now believe, is their inalienable right), health producers can claim, with some justification, that they are doing their best to meet the demand, though the shortage of the demanded commodity (health, in this case) will, regret- tably, lead to some increase in price. It would seem that the two approaches are not antagonistic, since curative and preventive medicine have always been part and parcel of medical practice. However, anticipatory medicine is not the same as traditional preventive medicine which was limited mainly to vaccination against specific diseases, and the reduction of the spread of infection by maintaining a clean water supply, abattoir inspection, control of the food chain, etc. The transition from preventive to anticipatory medicine is a leap from an empirical, pragmatic approach to a theoretical and visionary one. One general practitioner, shared his unease about the new fashion of anticipatory care with the readers of the British 33 Medical Journal. There are no indi- viduals any more but an army which must be fit to discharge its military task. He believed that this kind of medicine required a completely different frame of mind from that of a traditional doctor, who listens to the patient and tries to makes sense of complex messages of fear and reported symp- toms. As an economist, Tussing naively believed that in this way diseases would be 34 prevented and health expenditure greatly reduced. As Richard Asher used to say, the only similarity between the car and the human body is that if something is seriously wrong with the design of the former you can send it back to its maker. What anticipatory care means in practice can be seen, for example, in the official guidelines on preventive care for a low-risk, healthy woman between the ages of 20 and 70. According to the American College of Physicians, she should visit her doctors annually and have 278 examinations, tests and counselling sessions. Note that this is recommended for a healthy woman, and does not include anticipatory care before the age of 20 and after the age of 70. It accepts evidence not according to its quality but according to its conformity with a foregone conclusion. The authors concluded: Any form of screening, including multiphasic, must be judged on the basis of its demonstrable health benefits. Since these control trial results have failed to demonstrate any beneficial effect on either mortality or morbidity, we believe that the use of general practice-based multiphasic screening in the middle-aged can no longer be advocated on scientific, ethical or economic grounds as a desirable public health measure.

During the internal medicine core clerkship order solian australia medications held for dialysis, the student can put into practice some of the ethical principles learned in the preclinical years order online solian treatment effect, especially by participating in discussions of informed consent and advance directives generic solian 50 mg with mastercard symptoms you have cancer. Additionally, the student learns to recognize ethical dilemmas and respect different perceptions of health, illness, and health care held by patients of various religious and cultural backgrounds. Basic ethical principles (autonomy, beneficence, nonmaleficence, truth- telling, confidentiality, and autonomy). The role of the physician in making decisions about the use of expensive or controversial tests and treatments. Circumstances when it may be unavoidable or acceptable to breach the basic ethical principles. Participating in a preceptor’s discussion with a patient about a requested treatment that may not be considered appropriate (e. Participating in family and interdisciplinary team conferences discussing end- of-life care and incorporating the patient’s wishes in that discussion. Recognize the importance of patient preferences, perspectives, and perceptions regarding health and illness. Demonstrate a commitment to caring for all patients, regardless of the medical diagnosis, gender, race, socioeconomic status, intellect/level of education, religion, political affiliation, sexual orientation, ability to pay, or cultural background. Recognize the importance of allowing terminally ill patients to die with comfort and dignity when that is consistent with the wishes of the patient and/or the patient’s family. Recognize the potential conflicts between patient expectations and medically appropriate care. Therefore, they must master and practice self- directed life-long learning, including the ability to access and utilize information systems and resources efficiently. Key sources for obtaining updated information on issues relevant to the medical management of adult patients. Key questions to ask when critically appraising articles on diagnostic tests: • Was there an independent, blind comparison with a reference (“gold”) standard? Key questions to ask when critically appraising articles on medical therapeutics: • Was the assignment of patients to treatments randomized? Performing a computerized literature search to find articles pertinent to a focused clinical question. Summarizing and presenting to colleagues what was learned from consulting the medical literature. Recognize the value and limitations of other health care professionals when confronted with a knowledge gap. Appropriate care by internists includes not only recognition and treatment of disease but also the routine incorporation of the principles of preventive health care into clinical practice. All physicians should be familiar with the principles of preventive health care to ensure their patients receive appropriate preventive services. Criteria for determining whether or not a screening test should be incorporated into the periodic health assessment of adults. General types of preventive health care issues that should be addressed on a routine basis in adult patients (i. Methods for counseling patients about risk-factor modification, including the “stages of change” approach to helping patients change behavior. General categories of high-risk patients in whom routine preventative health care must be modified or enhanced (e. The potential roles and limitations of genetic testing in disease prevention/early detection. Obtaining a patient history, including a detailed family history, vaccination history, travel history, sexual history, and occupational exposures. Counseling patients about safe-sex practices, smoking cessation, alcohol abuse, weight loss, healthy diet, exercise, and seat belt use. Locating recently published recommendations as well as original data regarding measures that should be incorporated into the periodic health assessment of adults. Address preventive health care issues as a routine part of their assessment of patients. Encourage patients to share responsibility for health promotion and disease prevention. Recognize the importance of patient preferences when recommending preventive health measures. Demonstrate commitment to using risk-benefit, cost-benefit, and evidence- based considerations in the selection preventive health measures. Demonstrate ongoing commitment to self-directed learning regarding preventive health measures. Prevention for the 21st century: setting the context through undergraduate medical education. It is essential for the student to learn that the physician’s responsibility toward the patient does not stop at the end of the office visit or hospitalization but continues in collaboration with other professionals to ensure that the patient receives optimal care. Key personnel and programs in and out of the hospital that may be able to contribute to the ongoing care of an individual patient for whom the student has responsibility (e. The role of the primary care physician in coordinating the comprehensive and longitudinal patient care plan, including communicating with the patient and family (directly, telephone, or email) and evaluating patient well-being through home health and other care providers. The role of the primary care physician in the coordination of care during key transitions (e. The role of clinical nurse specialists, nurse practitioners, physicians assistants, and other allied health professionals in co-managing patients in the outpatient and inpatient setting. The importance of reconciliation of medications at all transition points of patient care. Discussing with the patient and their family ongoing health care needs; using appropriate language, avoiding jargon, and medical terminology. Participating in requesting a consultation and identifying the specific question to be addressed. Obtaining a social history that identifies potential limitations in the home setting which may require an alteration in the medical care plan to protect the patient’s welfare. Participate, whenever possible, in coordination of care and in the provision of continuity. Coordinating care across diseases, settings, and clinicians: a key role for the generalist in practice. Quality indicators of continuity and coordination of care for vulnerable elder persons. Management strategies need to take into account the effects of aging on multiple organ systems and socioeconomic factors faced by our elderly society. As the number of geriatrics patients steadily rises, the internist will devote more time to the care of these patients.
His mother’s maternal uncle and her brother died before the age of 30 years of massive cerebral hemorrhages cheap solian 50mg without a prescription symptoms anxiety. Physical examination shows deep ecchymoses over the buttocks and severe swelling of the left knee buy discount solian doctor of medicine. The most likely explanation for these findings is a deficiency of which of the following? A 56-year-old man has had a small solian 50 mg online medicine numbers, slowly growing nodule on his chin during the past 3 years. Examination of tissue obtained on excision of the lesion is most likely to show which of the following? A 23-year-old woman comes to the physician because of a 5-month history of intermittent discharge from both breasts. Physical examination shows scant white fluid expressible from the breasts bilaterally. Serum studies are most likely to show an increase in which of the following hormone concentrations? A 39-year-old man has the acute onset of pain, corneal clouding, and diffuse redness in the left eye. During sleep evaluation, he is noted to snore loudly and stop breathing for prolonged periods of 30 to 40 seconds. Toward the end of one of these apneic periods, arterial blood gas analysis is done. A 65-year-old woman comes to the physician because of a 2-day history of a high temperature, chills, and headache. Examination shows lethargy and severe neck rigidity; no other abnormalities are noted. Which of the following organisms is most likely to be found on Gram stain of cerebrospinal fluid? A 55-year-old man who is a farmer is brought to the emergency department 30 minutes after his wife found him unresponsive in their barn. She reports that he was foaming at the mouth and had evidence of tearing of the eyes, vomiting, and diarrhea. She often has episodes of dropping her head, slurred speech, and suddenly dropping things from her hands, all lasting for seconds to minutes. In addition, she frequently has vivid, colorful dreams just before falling asleep. Occasionally, when in certain emotionally charged situations, she feels like her whole body goes limp; however, she remembers everything. A 15-year-old girl is brought to the physician by her mother for a follow-up examination. Her mother says, “I am worried because she’s refused to take her medication since she started dating this new guy. After the mother is asked to leave the room, which of the following is the most appropriate statement by the physician to begin a discussion of this patient’s lack of adherence to her medication regimen? A 78-year-old woman is brought to the physician because of a headache and visual problems for 4 days. The headache is more severe on the left side, in the area above and in front of her ear. A 65-year-old man comes to the physician because of a 6-week history of fatigue and difficulty swallowing; he also has had a 6. Ten years ago, he underwent operative resection of squamous cell carcinoma of the floor of the mouth. He has smoked 2 packs of cigarettes daily for 40 years and drinks 60 oz of alcohol weekly. A 35-year-old woman comes to the physician because of abdominal pain for 6 months. Physical examination shows ecchymoses in various stages of healing over the upper and lower extremities. It is most appropriate for the physician to ask which of the following questions to begin a discussion with this patient about the possibility of physical abuse? A 22-year-old football player is brought to the emergency department 1 hour after he sustained a left leg injury during a tackle. Physical examination shows mild tenderness and anterior instability of the tibia with the knee in 90 degrees of flexion (positive drawer sign). A postmenopausal 60-year-old woman comes to the physician because of a 2-year history of vaginal dryness, intermittent vaginal pain, and decreased pleasure with sexual intercourse. A 73-year-old woman is brought to the emergency department because of severe back pain for 1 day. Which of the following is the most likely underlying cause of this patient’s condition? An 18-year-old man comes to the physician because of nausea, headache, blood in his urine, and malaise for 2 days. Three weeks ago, he had severe pharyngitis that resolved spontaneously after several days without antibiotic therapy. A 60-year-old woman comes to the physician because of a 3-month history of abdominal fullness and increasing abdominal girth with vague lower quadrant pain. Which of the following is the most appropriate statement by the physician at this time? A 26-year-old woman comes to the emergency department because of a 12-hour history of lower abdominal pain and vaginal bleeding. Measurement of which of the following is the most appropriate next step in management of this patient? A 25-year-old woman with stable cystic fibrosis meets inclusion criteria for a placebo-controlled industry-sponsored research study on a new treatment. The primary care physician is not part of the research team, but he is familiar with the research and considers it to be scientifically sound. The research protocol provides medication and medical care limited to assessing medication effects and adverse effects for 6 months. Which of the following is the most appropriate initial response by the primary care physician? The members of the committee responsible for the report were chosen for their special competences and with regard for appropriate balance. Department of Health and Human Services Office of Disease Prevention and Health Promotion, Contract No. Food and Drug Administration; the National Institutes of Health; the Centers for Disease Control and Prevention; the U. Department of Agriculture; the Department of Defense; the Institute of Medicine; the Dietary Reference Intakes Private Foundation Fund, including the Dannon Institute and the International Life Sciences Institute, North America; and the Dietary Reference Intakes Corporate Donors’ Fund. Contributors to the Fund in- clude Roche Vitamins Inc, Mead Johnson Nutrition Group, and M&M Mars.
Records of the specifics of therapy with unsealed radionuclides should be maintained at the hospital and given to the patient along with written precautionary instructions purchase solian overnight medicine effects. In the case of death of a patient who has had radiotherapy with unsealed radionuclides in the last few months discount solian line treatment centers for depression, special precautions may be required solian 100 mg with amex medications 2 times a day. Primum non nocere, the old Latin motto meaning ‘first, do no harm’ should be prevalent in the medical uses of radiation. Deriving from the maxim, one of the principal precepts of radio-diagnostic and radio-therapeutic practitioners should be non-maleficence or mischief, namely that given a medical problem, it may be better not to do something, or even to do nothing, than to risk causing more harm than good. It reminds the practitioner that other diagnostic or therapeutic procedures may be available and that they must be taken into consideration when debating the use of any procedure that carries an obvious risk of harm but a less certain chance of benefit. Prevention of accidents to patients undergoing radiation therapy Many accidents and mis-administrations have occurred involving patients undergoing treatment from external beam or solid brachytherapy sources. Therapy involving unsealed sources is also a cause of mishaps, but affects a different kind of professional and should be treated separately. An effective approach for preventing such situations is to study illustrative severe accidents, discuss the causes of these events and contributory factors, summarize the sometimes devastating consequences of these events, and provide recommendations on their prevention. Challenges include institutional arrangements, staff training, quality assurance programmes, adequate supervision, a clear definition of responsibilities and prompt reporting. It addresses a diverse audience of professionals directly involved in radiotherapy procedures, hospital administrators, and health and regulatory authorities. In many of the accidental exposures that have occurred, a single cause cannot be identified. Usually, there was a combination of factors contributing to the accident, for example, deficient staff training, lack of independent checks, lack of quality control procedures and absence of overall supervision. Such combinations often point to an overall deficiency in management, allowing patient treatment in the absence of a comprehensive quality assurance programme. The use of radiation therapy in the treatment of cancer patients has grown considerably and is likely to continue to increase. Major accidents are rare, but are likely to continue to happen unless awareness is increased. Explicit requirements on measures to prevent radiotherapy accidents are needed with respect to regulations, education and quality assurance. Preventing accidental exposures from new external beam radiation therapy technologies New external beam radiation therapy technologies are becoming increasingly used. These new technologies are meant to bring substantial improvement to radiation therapy. However, this is often achieved with a considerable increase in complexity, which, in turn, brings with it opportunities for new types of human error and problems with equipment. It is based on lessons learned from accidental exposures, which are an invaluable resource for revealing vulnerable aspects of the practice of radiotherapy, and for providing guidance for the prevention of future occurrences. Dissemination of information on errors or mistakes as soon as they become available is crucial in radiation therapy with new technologies. In addition, information on circumstances that almost resulted in serious consequences (near misses) is also important, as the same type of event may occur elsewhere. Sharing information about near misses is, thus, a complementary and important aspect of prevention. Disseminating the knowledge and lessons learned from accidental exposures is crucial in preventing recurrence. This is particularly important in radiation therapy; the only application of radiation in which very high radiation doses are deliberately given to patients to achieve cure or palliation of disease. Notwithstanding the above, disseminating lessons learned from serious incidents is necessary but not sufficient when dealing with new technologies. It is of the utmost importance to be proactive and continually strive to answer questions such as: ‘What else can go wrong? While the recommendations specifically apply to new external beam therapies, the general principles for prevention are applicable to the broad range of radiotherapy practices in which mistakes could result in serious consequences for the patient and practitioner. The recommendations provide elements for mobilizing for future effective work as outlined below. Independent verification should be performed of beam calibration in beam radiation therapy. Independent calculation should be performed of the treatment times and monitor units for external beam radiotherapy. Prospective safety assessments should be undertaken for preventing accidental exposures from new external beam radiation therapy technologies, including failure modes and effects analysis, probabilistic safety assessment, and risk matrix, in order to develop risk informed and cost effective quality assurance programmes. Moderated electronic networks and panels of experts supported by professional bodies should be established in order to expedite the sharing of knowledge in the early phase of introducing new external beam radiation therapy technologies. A collaborating team of specifically trained personnel following quality assurance procedures is necessary to prevent accidents. Maintenance is an indispensable component of quality assurance; external audits of procedures reinforce good and safe practice, and identify potential causes of accidents. Accidents and incidents should be reported and the lessons learned should be shared with other users to prevent similar mistakes. The available data on doses received by people approaching patients after implantation show that, in the vast majority of cases, the dose to comforters and carers remains well below 1 mSv/a. Moreover, due to the low activity of an isolated seed and its low photon energy, no incident/accident linked to seed loss has ever been recorded. A review of available data shows that cremation can be allowed if 12 months have elapsed since 125 103 implantation with I (3 months for Pd). If the patient dies before this time has elapsed, specific measures must be undertaken. However, although the therapy related modifications of the semen reduce fertility, patients must be aware of the possibility of fathering children after such a permanent implantation, with a limited risk of genetic effects for the child. Patients with permanent implants must be aware of the possibility of triggering certain types of security radiation monitor. Considering the available experience after brachytherapy and external irradiation of prostate cancer, the risk of radio-induced secondary tumours appears to be extremely low, but further investigation might be helpful. Only the (rare) case where the patient’s partner is pregnant at the time of implantation may need specific precautions. Specific recommendations should be given to patients to allow them to deal adequately with this event. As far as cremation of bodies is concerned, consideration should be given to the activity that remains in the patient’s ashes and the airborne dose, potentially inhaled by crematorium staff or members of the public. Specific recommendations have to be given to the patient to warn the surgeon in case of subsequent pelvic or abdominal surgery. The wallet card including the main information about the implant (see above) may prove to be helpful in such a case of triggering certain types of security radiation monitor. The risk of radio-induced secondary tumours following brachytherapy should be further investigated. Avoidance of radiation injuries from medical interventional procedures Interventional radiology (fluoroscopically guided) techniques are being used by an increasing number of clinicians not adequately trained in radiation safety or radiobiology. Many of these interventionists are not aware of the potential for injury from these procedures or the simple methods for decreasing their incidence.
Order 100mg solian. How I found out I was pregnant | DPO symptoms day by day.