
Cogswell Polytechnical College. T. Basir, MD: "Buy Kamagra Chewable online - Discount Kamagra Chewable online".
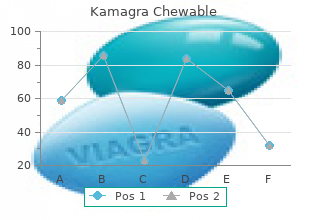
The intermediary In thio compounds buy kamagra chewable 100 mg on line erectile dysfunction and diabetes type 2, desulfuration results products are labile and break up into the from substitution of sulfur by oxygen (e kamagra chewable 100mg low cost impotence and diabetes 2. O-dealkylation and S-dear- that biotransformation is not always to be ylationproceed viaananalogousmechanism equated with bioinactivation order kamagra chewable line erectile dysfunction treatment with injection. Accordingly, pharmaceuticals of levels of ciclosporin below the therapeutic diverse chemical structure can be metabo- range (C). When sev- inadequate, the risk of transplant rejection eral drugs are metabolized by the same iso- will be enhanced. The antifungal agent keto- concentration usually leads to accelerated conazole enhances the nephrotoxicity of ci- drug metabolism. Obviously, Luellmann, Color Atlas of Pharmacology © 2005 Thieme Drug Metabolism by Cytochrome P450 39 A. With few exceptions, therapeuti- 50% of the amine will be present in the pro- cally used drugs and their metabolites have tonated, hydrophilic, membrane-imperme- much smaller molecular weights and can ant form (blue dots), whereas the other half, therefore undergo glomerular filtration, representing the uncharged amine (red i. Sep- dots), can leave the tubular lumen in accord- arating the capillary endothelium from the ance with the resulting concentration gra- tubular epithelium,thebasal membrane dient. The rel- will be present in the uncharged, reabsorb- ative density of this barrier depends on the ableform. LoweringorraisingurinarypHby electric charge of molecules that attempt to half a pH unit would result in analogous permeate it. Intentional alteration of urinary pH can proximal tubules into the tubular fluid via be used in intoxications with proton-accep- special energy-consuming transport sys- tor substances in order to hasten elimination tems. During passage down the renal tubule, primary urinary volume shrinks to about 1%; accordingly, there is a corresponding concentration of filtered drug or drug me- tabolites (A). The resulting concentration gradient between urine and interstitial fluid is preserved in the case of drugs incapable of permeating the tubular epithelium. How- ever, with lipophilic drugs the concentration gradient will favor reabsorption of the fil- tered molecules. In this case, reabsorption is not based on an active process but results instead from passive diffusion. Accordingly, Luellmann, Color Atlas of Pharmacology © 2005 Thieme The Kidney as an Excretory Organ 41 A. Glomerular filtration Blood Plasma protein Endothelium Basal membrane Slit diaphragm Epithelium 180 l Glomerular Primary urine filtration Drug of drug Podocyte processes Primary urine D. Tubular reabsorption pH = 7,0 pKa of substance pKa= 7,0 100 + R 50 Concentration of drug 1,2 l % in tubule 6 6,5 7 7,5 8 Final urine pKa= 7,5 100 C. Active secretion 50 + + + + % + + + 6 6,5 7 7,5 8 + + + + + + + + pKa= 6,5 + + 100 + + + + + Tubular - - transport 50 system for - - - - - - + - - Cations - - - % – - - - - 6 6,5 7 7,5 8 Anions - - - - - pH = 7,0 pH of urine Luellmann, Color Atlas of Pharmacology © 2005 Thieme 42 Drug Elimination cytes, only a fraction of the amount Presystemic Elimination absorbed may reach the blood in the The morphological barriers of the body are hepatic vein. Depending on the in enzyme activity (increase in physicochemical properties of drugs, in- smooth endoplasmic reticulum) can tended targets on the surface or the inside be induced by other drugs. Parenteral administration of a drug of pharmacokinetics will be subject to yet an- course circumvents presystemic elimina- other process. The drug permeates through the epithe- lipid-rich organ with a large surface, the lial barrier of the gut into the enterocyte; lungs can take up lipophilic or amphi- however, a P-glycoprotein transports it philic agents to a considerable extent back into the intestinal lumen. As a result, and release them slowly after blood levels the amount actually absorbed can be fall again. This counter-trans- lungs act as a buffer and protect the heart port can vary interindividually for an against excessive concentrations after identical substance and moreover may rapid i. An general circulation, the ingested sub- im portantexam pleistheuseofglucocorti- stance is broken down enzymatically, coids in the treatment of asthma. Other drugs or systemic elimination entail only a minimal agents may inhibit or stimulate the systemic load for the organism (p. Here, many enzymes are atworktoalterendogenousand exog- enoussubstanceschem icallysoasto promote their elimination. Depending on the quantity of drug being taken up and metabolized by the hepato- Luellmann, Color Atlas of Pharmacology © 2005 Thieme Presystemic Elimination 43 A. Presystemic elimination Estradiol >95% Examples of presystemic elimination Testosterone >95% Fraction of oral dose that does not reach systemic circulation: Sumatriptan ~85% Budesonide >80% Verapamil ~80% Drug Furosemide 50–70% Metabolite Nifedipine ~50% Atenolol 40–50% Diclofenac ~40% Propranolol 20–50% Systemic bioavailability (fraction of oral dose) Lung: Storage Liver: Biotransformation Intestinal wall: Biotransformation Back-transport into lumen by efflux pumps Luellmann, Color Atlas of Pharmacology © 2005 Thieme 44 Pharmacokinetics and the apparent volume of distribution Vapp Drug Concentration in the Body as a (p. For absorption, this follows from the simple The smaller the volume of distribution or the fact that the amount of drug being moved larger the total clearance, the shorter is the per unit of time depends on the concentra- half-life. In drug absorp- unchanged form, the half-life of elimination tion from the alimentary tract, the intestinal can be calculated from the cumulative ex- content and blood would represent the com- cretion in urine; the final total amount elim- partments containing initially high and low inated corresponds to the amount absorbed. In drug elimi- Hepatic elimination obeys exponential nation via the kidney, excretion often de- kinetics because metabolizing enzymes op- pends on glomerular filtration, i. As the blood concentration falls, the amount of drug metabolized per unit time amount of drug filtered per unit of time diminishes with decreasing blood concen- diminishes. The exponential The best-known exception to exponential time course implies constancy of the interval kinetics is the elimination of alcohol (etha- duringwhichtheconcentrationdecreasesby nol), which obeys a linear time course (zero- one-half. This interval represents the half- order kinetics), at least at blood concen- life (t½) and is related to the elimination rate trations > 0. The rate-limiting enzyme, alcohol dehydrogen- two parameters, together with the initial ase, achieves half-saturation at very low sub- concentration c0, describe a first-order (ex- strate concentrations, i. Thus, reaction velocity reaches a The constancy of the process permits cal- plateau at blood ethanol concentrations of culation of the plasma volume that would be about0. Depending on whether plasma concentration falls as a result of urinary ex- cretion or of metabolic alteration, clearance is considered to be renal or hepatic. Renal and hepatic clearances add up to total clear- ance (Cltot) in the case of drugs that are eliminated unchanged via the kidney and biotransformed in the liver. Cltot represents the sum of all processes contributing to elimination; it is related to the half-life (t½) Luellmann, Color Atlas of Pharmacology © 2005 Thieme D rugConcentrationintheBody 45 A. Exponential elimination of drug Concentration (co) of drug [amount/vol] Plasma half-life t1 c =c ·e-kt 2 t o c = 1 c 1 2 o ct:Drug concentration at timet 2 t = ln 2 co:Initial drug concentration after 12 k administration of drug dose e:base of natural logarithm k:elimination constant Unit of time Time (t) Notional plasma volume per unit of time freed of drug = clearance[vol/t] Amount excreted per unit of time[amount/t] Total amount of drug (Amount administered) = Dose excreted Time (t) Luellmann, Color Atlas of Pharmacology © 2005 Thieme 46 Pharmacokinetics function (k1 and k2 represent the rate con- Time Course of Drug Concentration stants for absorption and elimination, re- in Plasma spectively). The velocity of absorption depends on thus represents an open system wherein the the route of administration. The more rapid actual drug concentration reflects the inter- the absorption, the shorter will be the time play of intake (ingestion) and egress (elimi- (tmax) required to reach the peak plasma nation). When orally administered drug is level (cmax), the higher will be the cmax,and absorbed from the stomach and intestine, the earlier will the plasma level begin to fall speed of uptake depends on many factors, again. Transport in blood conveys the and intravenous administrations of a given drug to different organs (distribution), into dose of a particular drug corresponds to the which it is taken up to a degree compatible proportion of drug entering the systemic with its chemical properties and rate of circulation after oral administration. Absorption from The determination of plasma levels affords a the gutdiminishes as the mucosa–blood gra- comparison of different proprietary prepara- dient decreases. Plasma concentration tions containing the same drug in the same reaches a peak when the amount of drug dosage. Identical plasma level–time curves leaving the blood per unit of time equals that of different manufacturers’ products with being absorbed.

It has no significant with an estimated 250 million cases and 1 million deaths drug–drug interactions cheap kamagra chewable 100 mg overnight delivery vasodilator drugs erectile dysfunction, with no dose adjustment required annually discount kamagra chewable 100 mg otc erectile dysfunction lubricant, mainly in sub-Saharan African children (where in renal or hepatic impairment buy discount kamagra chewable 100mg line impotence sentence. Plasmodium falciparum differs Jesuit priest and trained apothecary, who sent a small quan- in that it has no persistent hepatic cycle. It cides) act at this site and are used for: was used for all fevers, among them malaria, the occurrence • Radical cure, i. Female anopheles mosquitoes require a blood meal for Vaccine development against both falciparum and vivax egg production, and in the process of feeding they inject malaria concentrates mostly on surface antigens (e. As no cumsporozoite protein) involved in the pre-erythrocytic drugs are effective against sporozoites, infection with the stages, before invasion of liver cells (stage 1). The merozoites re-enter red cells and the cycle is iable, advice on therapy and prophylaxis in this section is repeated. Drugs that act at this stage in the cycle of the parasite may be used for: Chemotherapy of an acute attack • Treatment of acute attacks of malaria. This is called suppressive prophylaxis Successful management demands attention to the follow- as it does not cure the hepatic cycle (above). Drugs used for malaria, and their principal actions, are clas- Falciparum (‘malignant’) malaria sified in Table 15. Falciparum malaria in the non-immune is a medical emer- gency, and malaria of unknown infecting species should be Drug-resistant malaria treated as though it were falciparum. The regimen depends on the condition of the patient; the doses quoted are for Drug-resistantparasites constitutea persistent problem. Chloroquine resistance is now widespread; there- modium falciparum is now resistant to chloroquine and fore this drug should not be used for the treatment of fal- sulfadoxine-pyrimethamine in many parts of the world. Areas of high risk for resistant parasites include sub-Saharan Africa, Latin America, Oceania (Papua New Guinea, Solo- If the patient can swallow and there are no serious com- mon Islands, Vanuatu) and some parts of South-East Asia. There options are as follows: are concerns with emerging artesunate resistance in western A quinine salt:4 600 mg 8-hourly by mouth for 5–7 • Cambodia due to monotherapy. Chloroquine-resistant Plas- days, followed by doxycycline 200 mg daily for at least modium vivax is also reported. This additional therapy is necessary as quinine propriate or low dosing of antimalarials are important alone tends to be associated with a higher rate of drivers of resistance. It is not necessary to use follow-on therapy after • Intravenous artesunate showed a clear benefit when Riamet, mefloquine or Malarone. Jones K L, Donegan S, Lalloo D G 2007 Artesunate quinidine or mefloquine in the previous 24 h; see also warnings about versus quinine for treating severe malaria. Intravenous artesunate • Mefloquine, doxycycline and atovaquone-proguanil should be accompanied by a 7-day course of (Malarone) are the most commonly advised doxycycline. Chloroquine, alone or in combination with proguanil, may be considered in Non-falciparum (‘benign’) malarias areas of the world where the risk of acquiring These are usually due to Plasmodium vivax or less commonly chloroquine resistant falciparum malaria is low, to Plasmodium ovale or Plasmodium malariae. This is sufficient for Plasmo- • The progressive rise in plasma concentration to steady dium malariae infection, but for Plasmodium vivax and Plas- state (after t½Â 5), sometimes attained only after weeks modium ovale eradication of the hepatic parasites is (consider mefloquine t½ 21 days, chloroquine t½ 50 necessary to prevent relapse, by giving: days), allows unwanted effects (which can impair • Primaquine, 15 mg/day for 14 days started after the compliance or be unsafe) to be delayed, in some chloroquine course has been completed. British acquired about the time of departure, are still incubating National Formulary, that apply particularly to their own in the liver and will develop into the erythrocyte phase. The traveller should be aware that any 8Dondorp A, Nosten F, Stepniewska K, et al 2005 Artesunate versus illness occurring within a year, and especially within 3 quinine for treatment of severe falciparum malaria: a randomised trial. Chloroquine and proguanil may be used for periods of 9 • The active component of many drugs, whether acid or base, is relatively up to 5 years, and mefloquine for up to 1–2 years; insoluble and may present a problem in formulation. This is overcome by adding an acid to a base or vice versa; the weight of the salt differs expert advice should be taken by long-term travellers, according to the acid or base component, i. Where there may be variation, therefore, the amount of drug prescribed is expressed as the weight of the active • Naturally acquired immunity offers the most reliable component, in the case of chloroquine, the base. Chloro- partial immunity and the disease often becomes no quine may be used in full dose to treat chloroquine- more than an occasional inconvenience. Mefloquine considered for pregnant women and young is teratogenic in animals and a woman should avoid preg- children returning to their permanent homes in nancy while taking it, and for 3 months afterwards (al- malarious areas after a prolonged period of stay in a though evidence is accruing that it may be safe for use in non-endemic area, pending suitable arrangements for chloroquine-resistant areas). It is active against the blood forms and also the of parasite may differ gametocytes (formed in the mosquito) of Plasmodium vivax, n during the last few months of pregnancy in areas Plasmodium ovale and Plasmodium malariae; it is ineffective where Plasmodium falciparum is prevalent (to avert against many strains of Plasmodium falciparum and also the risk of miscarriage). Chloroquine is readily absorbed from the gastrointestinal tract and is concentrated several- Examples of standard prophylactic regimens fold in various tissues, e. Chloroquine is partly inactivated by metabolism • Malarone: 1 tablet daily (start 1–2 days before travel). These available) in the last minute traveller with no history of are not a threat to vision and reverse when the drug is previous mefloquine exposure or who is intolerant of stopped. In the early stage it takes the form of visual field mend giving a loading dose of prophylactic antimalarials defects; late retinopathy classically gives the picture of mac- for the purpose of rapidly achieving steady-state plasma ular pigmentation surrounded by a ring of pigment (the concentration. Where subjects are already taking of scotomas, photophobia, defective colour vision and de- other drugs, e. Other reactions include pruritus, which may be intoler- able and is common in Africans, headaches, gastrointesti- nal disturbance, precipitation of acute intermittent Antimalarial drugs and pregnancy porphyria in susceptible individuals, mental disturbances Women living in endemic areas in which Plasmodium falci- and interference with cardiac rhythm, the latter especially parum remains sensitive to chloroquine should take chloro- if the drug is given i. Long-term use is associated with reversible bleach- (an ‘antifol’, see below) may be taken for prophylaxis ing of the hair and pigmentation of the hard palate. More rarely, hallucinations, seizures diac arrhythmias and coma; as little as 50 mg/kg can be and psychoses occur. These effects are principally due to the profound neg- patients taking b-adrenoceptor and calcium channel an- ative inotropic action of chloroquine. Diazepam was found tagonists, because it causes sinus bradycardia; quinine fortuitously to protect the heart and adrenaline/epineph- can potentiate these and other dose-related effects of rine reduces intraventricular conduction time; this combi- mefloquine. Less severe reactions includ- Halofantrine ing headache, dizziness, depression and insomnia have been reported but there is uncertainty as to whether these Halofantrine (t½2. The drug should not be used forms of all four Plasmodium species, especially Plasmodium in travellers with a history of neuropsychiatric disease in- falciparum and Plasmodium vivax, and at the schizont stage. Absorp- activities require fine coordination or spatial performance, tion of halofantrine from the gastrointestinal tract is vari- e. It is no inate the hepatic forms of Plasmodium vivax and Plasmodium longer recommended for the treatment of drug-resistant ovale after standard chloroquine therapy, but only when the Plasmodium vivax malaria and should also not be used for risk of re-infection is absent or slight. Primaquine is well absorbed from the gastroin- as a fixed drug combination with artemether (Riamet or testinal tract, is only moderately concentrated in the tissues, Co-artem). Unlike halofantrine, cramps, methaemoglobinaemia, granulocytopenia and there are no cardiotoxicity concerns and it is well haemolytic anaemia, especially in patients with genetic tolerated. Mefloquine is rapidly absorbed from the gastrointestinal Proguanil (chloroguanide) tract and its action is terminated by metabolism. When Proguanil (t 17 h) inhibits dihydrofolate reductase, ½ used for prophylaxis, 250 mg (base)/week should be which converts folic to folinic acid, deficiency of which taken, commencing 1–3 weeks before entering and con- inhibits plasmodial cell division. It bacteria but unlike humans, cannot make use of pre- should not be given to patients with hepatic or renal formed folic acid. It is used alone (usually with chloro- tosis) and increasing resistance to pyrimethamine, this reg- quine) for malaria prophylaxis, and is also available imen is no longer recommended for prophylaxis, although with atovaquone (as Malarone: proguanil hydrochlo- it continues to be available in parts of Africa, in particular ride 100 mg plus atovaquone 250 mg) for prophylaxis Zimbabwe and neighbouring countries. Proguanil is moderately well absorbed from the gut and Quinine is excreted in the urine either unchanged or as an active me- Quinine (t½ 9 h; 18 h in severe malaria) is obtained from tabolite.
Generic 100mg kamagra chewable otc. Men impotence will be cured with Siddha.
Thus kamagra chewable 100 mg discount weight lifting causes erectile dysfunction, most drug interactions with tacrolimus are managed using appropriate tacrolimus dosage modification with tacrolimus concentration monitoring as a guide buy line kamagra chewable erectile dysfunction from stress. Gastrointestinal prokinetic agents (cisapride cheap generic kamagra chewable uk erectile dysfunction age onset, metoclopramide) may increase tacrolimus concentrations. It allows individualized target serum con- centrations to be chosen for a patient, and each pharmacokinetic parameter can be cus- tomized to reflect specific disease states and conditions present in the patient. Literature- based recommended dosing is a very commonly used method to prescribe initial doses of tacrolimus. Doses are based on those that commonly produce steady-state concentrations in the lower end of the therapeutic range, although there is a wide variation in the actual concentrations for a specific patient. Pharmacokinetic Dosing Method The goal of initial dosing of tacrolimus is to compute the best dose possible for the patient in order to prevent graft rejection or graft-versus-host disease given their set of disease states and conditions that influence tacrolimus pharmacokinetics, while avoiding adverse drug reactions. In order to do this, pharmacokinetic parameters for the patient will be estimated using average parameters measured in other patients with similar dis- ease state and condition profiles. Unfortunately, there is no good way to estimate the elimination characteristics of liver metabolized drugs using an endogenous marker of liver function in the same fashion that serum creatinine and esti- mated creatinine clearance are used to estimate the elimination of agents that are renally eliminated. Because of this, a patient is categorized according to the disease states and conditions that are known to change tacrolimus clearance, and the clearance previously measured in these studies is used as an estimate of the current patient’s clearance rate. For example, an adult transplant patient with normal liver function would be assigned a tacrolimus clearance rate equal to 0. Because of the complex absorption profile and the fact that the drug is usually administered twice daily, a very simple pharmacokinetic equation that calculates the average tacrolimus steady-state concentration (Css in ng/mL =μg/L) is widely used and allows maintenance dose computation: Css = [F(D/τ)] / Cl or D = (Css ⋅ Cl ⋅τ) / F, where F is the bioavailability fraction for the oral dosage form (F averages 0. If the drug is to be given as a continuous intravenous infusion, the equivalent equation for that route of administra- tion is Css = ko/Cl or ko = Css ⋅ Cl, where ko is the infusion rate in milligrams per hour. More important than these general guidelines are the specific requirements for each graft type as defined by the transplant center where the surgery was conducted. Clinicians should become familiar with the tacrolimus protocols used at the various institutions at which they practice. Although it is unlikely that steady state has been achieved, tacrolimus concentra- tions are usually obtained on a daily basis, even when dosage changes were made the previ- ous day, owing to the critical nature of the therapeutic effect provided by the drug. Suggest an initial oral tacrolimus dose designed to achieve a steady-state tacrolimus trough blood concentration equal to 15 ng/mL. Tacrolimus concentrations would be obtained on a daily basis with steady state expected to occur in about 3 days (5 half-lives = 5 ⋅ 12 h = 60 h). Example 2 Same patient as in example 1, except compute an initial dose using intra- venous tacrolimus. Tacrolimus concentrations would be obtained on a daily basis with steady state expected to occur in about 3 days (5 half-lives = 5 ⋅ 12 h = 60 h). Literature-Based Recommended Dosing Because of the large amount of variability in tacrolimus pharmacokinetics, even when concurrent disease states and conditions are identified, many clinicians believe that the use of standard tacrolimus doses for various situations is warranted. The original com- putation of these doses was based on the pharmacokinetic dosing method described in the previous section, and subsequently modified based on clinical experience. In general, the expected tacrolimus steady-state concentration used to compute these doses is dependent upon the type of transplanted tissue and the post transplantation time line. Suggest an initial oral tacrolimus dose designed to achieve a steady-state tacrolimus trough blood concentration within the therapeutic range. Choose tacrolimus dose based on disease states and conditions present in the patient and transplant type. Tacrolimus concentrations would be obtained on a daily basis with steady state expected to occur after 3 days (5 half-lives = 5 ⋅ 12 h = 60 h) of treatment. Example 4 Same patient as in example 3, except compute an initial dose using intra- venous tacrolimus. Choose tacrolimus dose based on disease states and conditions present in the patient and transplant type. Tacrolimus concentrations would be obtained on a daily basis with steady state expected to occur after 3 days (5 half-lives = 5 ⋅ 12 h = 60 h) of treatment. Because of pharmacokinetic variability, the narrow therapeutic index of tacrolimus, and the severity of tacrolimus adverse side effects, measurement of tacrolimus concentrations is mandatory for patients to ensure that therapeutic, nontoxic levels are present. In addition to tacrolimus concen- trations, important patient parameters (transplanted organ function tests or biopsies, clinical signs and symptoms of graft rejection or graft-versus-host disease, potential tacrolimus side effects, etc. Since alternate methods to monitor cyclosporine concentrations have met with some success, investigators have begun suggesting similar methods for tacrolimus. When tacrolimus concentrations are measured in patients and a dosage change is nec- essary, clinicians should seek to use the simplest, most straightforward method available to determine a dose that will provide safe and effective treatment. In most cases, a simple dosage ratio can be used to change tacrolimus doses assuming the drug follows linear pharmacokinetics. Sometimes, it is useful to compute tacrolimus pharmacokinetic con- stants for a patient and base dosage adjustments on these. In this case, it may be possible to calculate and use pharmacokinetic parameters to alter the tacrolimus dose. Finally, com- puterized methods that incorporate expected population pharmacokinetic characteristics (Bayesian pharmacokinetic computer programs) can be used in difficult cases where con- centrations are obtained at suboptimal times or the patient was not at steady state when concentrations were measured. Linear Pharmacokinetics Method Assuming tacrolimus follows linear, dose-proportional pharmacokinetics,33 steady- state concentrations change in proportion to dose according to the following equation: Dnew/Css,new = Dold/Css,old or Dnew = (Css,new/Css,old)Dold, where D is the dose, Css is the steady-state concentration, old indicates the dose that produced the steady-state concen- tration that the patient is currently receiving, and new denotes the dose necessary to pro- duce the desired steady-state concentration. The patient would be expected to achieve steady-state conditions after the third day (5 t1/2 = 5 ⋅ 12 h = 60 h) of therapy. Using linear pharmacokinetics, the new dose to attain the desired concentration should be proportional to the old dose that produced the measured concentration (total daily dose = 5 mg/dose ⋅ 2 doses/d = 10 mg/d): Dnew = (Css,new/Css,old)Dold = (15 ng/mL / 24 ng/mL) 10 mg/d = 6. A steady-state trough tacrolimus concentration should be measured after steady state is attained in 3–5 half-lives. Since the patient is expected to have a half-life equal to 12 hours, the tacrolimus steady-state concentration could be obtained anytime after the third day of dosing (5 half-lives = 5 ⋅ 12 h = 60 h). Tacrolimus concentrations should also be meas- ured if the patient experiences signs or symptoms of graft rejection, or if the patient develops potential signs or symptoms of tacrolimus toxicity. The patient would be expected to achieve steady-state conditions after the third day (5 t1/2 = 5 ⋅ 12 h = 60 h) of therapy. Since the patient is expected to have a half-life equal to 12 hours, the tacrolimus steady-state concentration could be obtained anytime after the third day of dosing (5 half-lives = 5 ⋅ 12 h = 60 h). Tacrolimus concentrations should also be meas- ured if the patient experiences signs or symptoms of graft rejection, or if the patient develops potential signs or symptoms of tacrolimus toxicity. Pharmacokinetic Parameter Method The pharmacokinetic parameter method of adjusting drug doses was among the first techniques available to change doses using drug concentrations. It allows the computa- tion of an individual’s own, unique pharmacokinetic constants and uses those to calcu- late a dose that achieves desired tacrolimus concentrations. The pharmacokinetic param- eter method requires that steady state has been achieved and uses only a steady-state tacrolimus concentration. Tacrolimus clearance can be measured using a single steady- state tacrolimus concentration and the following formula for orally administered drug: Cl = [F(D/τ)] / Css, where Cl is tacrolimus clearance in L/h, F is the bioavailability fac- tor for tacrolimus (F = 0. If tacrolimus is administered intravenously, it is not necessary to take bioavailabil- ity into account: Cl = ko/Css, where Cl is tacrolimus clearance in liters per hour, ko is the tacrolimus infusion rate in milligrams per hour, and Css is the tacrolimus steady-state concentration in nanograms per milliliter which also equals micrograms per liter. Although this method does allow computation of tacrolimus clearance, it yields exactly the same tacrolimus dose as that supplied using linear pharmacokinetics.
Patients with painful conditions such as arthritis may continually change medications in the hope of finding a better one generic 100 mg kamagra chewable amex incidence of erectile dysfunction with age. Characteristics of the therapy itself can limit the degree of compliance; patients taking a drug once a day are much more likely to be compliant than those taking a drug four times a day purchase kamagra chewable online now erectile dysfunction research. Packaging may also be a deterrent to compliance—elderly arthritic patients often have difficulty opening their medication containers 100 mg kamagra chewable free shipping causes of erectile dysfunction in 60s. Lack of transportation as well as various cultural or personal beliefs about medications are likewise barriers to compliance. Strategies for improving compliance include enhanced communication between the patient and health care team members; assessment of personal, social, and economic conditions (often reflected in the patient’s lifestyle); development of a routine for taking medications (eg, at mealtimes if the patient has regular meals); provision of systems to assist taking medications (ie, containers that separate drug doses by day of the week, or medication alarm clocks that remind patients to take their medications); and mailing of refill reminders by the pharmacist to patients taking drugs chronically. The patient who is likely to discontinue a medication because of a perceived drug-related problem should receive instruction about how to monitor and understand the effects of the medication. Physicians, dentists, podiatrists, and veterinarians—and, in many states, specialized pharmacists, nurses, physician’s assistants, and optometrists—are granted authority to prescribe dangerous drugs (those bearing the federal legend statement, “Rx Only”) on the basis of their training in diagnosis and treatment (see Box: Who May Prescribe? Pharmacists are authorized to dispense prescriptions pursuant to a prescriber’s order provided that the medication order is appropriate and rational for the patient. Because of the multiplicity of third-party payers (health insurers) and Medicare and Medicaid claimants, the concept of electronic processing of prescriptions (“e-prescribing”) has become urgent. In addition to a health care provider’s unique identification number, some states require that prescriptions for controlled substances be written on tamper-resistant security prescription forms. The purpose of this legislation is to prevent forgeries and to tighten the control of prescription order forms. The concept of a “secure” prescription form was expanded by the federal government in 2008 to all prescriptions written for Medicaid patients. Any prescription for a Medicaid patient must be written on a security form if the pharmacist is to be compensated for the prescription service. The federal legend statement as well as the package insert is part of the packaging requirements for all prescription drugs. The package insert is the official brochure setting forth the indications, contraindications, warnings, and dosing for the drug. The prescriber, by writing and signing a prescription order, controls who may obtain prescription drugs. The pharmacist may purchase these drugs, but they may be dispensed only on the order of a legally qualified prescriber. Thus, a prescription is actually three things: the prescriber’s order in the patient’s chart, the written order to which the pharmacist refers when dispensing, and the patient’s medication container with a label affixed. Whereas the federal government controls the drugs and their labeling and distribution, the state legislatures control who may prescribe drugs through their licensing boards, eg, the Board of Medical Examiners. Prescribers must pass examinations, pay fees, and—in the case of some states and some professions—meet other requirements for relicensure such as continuing education. The federal government and the states further impose special restrictions on drugs according to their perceived potential for abuse (Table 65–2). The right to prescribe drugs has traditionally been the responsibility of the physician, dentist, podiatrist, or veterinarian. Prescribing now includes—in a number of states and in varying degrees—pharmacists, nurse practitioners, nurse midwives, physician’s assistants, and optometrists (see below). The development of large health maintenance organizations has greatly strengthened this expansion of prescribing rights because it offers these extremely powerful economic bodies a way to reduce their expenses. Many state boards have attempted to reserve some measure of the primary responsibility for prescribing to physicians by requiring that the ancillary professional work with or under a physician according to a specific protocol. In the state of California, this protocol must include a statement of the training, supervision, and documentation requirements of the arrangement and must specify referral requirements, limitations to the list of drugs that may be prescribed (ie, a formulary), and a method of evaluation by the supervising physician. Pharmacists may prescribe controlled substances under physician supervision in California, Massachusetts, Montana, New Mexico, North Carolina, North Dakota, and Washington. However, multiple prescriptions for the same drug may be written with instructions not to dispense before a certain date and up to a total of 90 days. These restrictive prescribing laws are intended to limit the amount of drugs of abuse that are made available to the public. Unfortunately, the inconvenience occasioned by these laws—and an unwarranted fear by medical professionals themselves regarding the risk of patient tolerance and addiction—continues to hamper adequate treatment of patients with terminal conditions. There is no excuse for inadequate treatment of pain in a terminal patient; not only is addiction irrelevant in such a patient, it is actually uncommon in patients who are being treated for pain (see Chapter 31). Some states have recognized the underutilization of pain medications in the treatment of pain associated with chronic and terminal conditions. California, for example, has enacted an “intractable pain treatment” act that reduces the difficulty of renewing prescriptions for opioids. These approved (labeled) uses or indications are set forth in the package insert that accompanies the drug. For a variety of reasons, these labeled indications may not include all the conditions in which the drug might be useful. Therefore, a clinician may wish to prescribe the agent for some other, unapproved (off-label), clinical condition, often on the basis of adequate or even compelling scientific evidence. Even if the patient suffers injury from the drug, its use for an unlabeled purpose does not in itself constitute “malpractice. Drug Safety Surveillance Governmental drug-regulating agencies have responsibility for monitoring drug safety. Practitioners may submit reports on any suspected adverse drug (or medical device) effect using a simple form obtainable from http://www. Dispensers of medications are required to distribute “Med Guides” to patients when these medications are dispensed. In addition, pharmacists often provide patient educational materials that describe the drug, its use, adverse effects, storage requirements, methods of administration, what to do when a dose is missed, and the potential need for ongoing therapy. For drugs in common use, the difference in cost between the trade-named product and generic products varies from less than twofold to more than 100-fold. In most states and in most hospitals, pharmacists have the option of supplying a generically equivalent drug product even if a proprietary name has been specified in the order. If the prescriber wants a particular brand of drug product dispensed, handwritten instructions to “dispense as written” or words of similar meaning are required. Some government- subsidized health care programs and many third-party insurance payers require that pharmacists dispense the cheapest generically equivalent product in the inventory (generic substitution). However, the principles of drug product selection by private pharmacists do not permit substituting one therapeutic agent for another (therapeutic substitution); that is, dispensing trichlormethiazide for hydrochlorothiazide would not be permitted without the prescriber’s permission even though these two diuretics may be considered pharmacodynamically equivalent. It cannot be assumed that every generic drug product is as satisfactory as the trade-named product, although examples of unsatisfactory generics are rare. Bioavailability—the effective absorption of the drug product—varies between manufacturers and sometimes between different lots of a drug produced by the same manufacturer.