
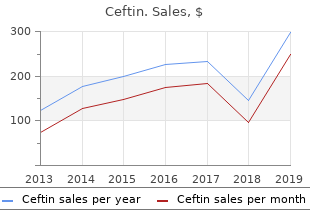
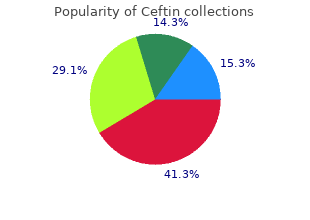
San Joaquin College of Law. N. Hatlod, MD: "Buy online Ceftin cheap - Safe online Ceftin".
A painful axillary mass is usually an acute abscess or an acute inflammation of the lymph node caused by infection on the extremity or breast supplied by the lymph node or hidradenitis suppurativa order cheap ceftin on-line virus 0000. Fever with a bilateral axillary mass would suggest an acute systemic infection or infectious mononucleosis buy online ceftin antimicrobial countertops. Fever with a unilateral axillary mass would suggest that there is mastitis ceftin 500 mg visa antibiotics for cellulitis, a breast abscess, or lymphangitis of the extremity supplied by the axillary lymph nodes. If the mass is unilateral, are there signs of an infection on the extremity or breast supplied by the axillary nodes? In tularemia, there will be a bubo on the extremity supplied by the axillary nodes, and in lymphadenitis, there should be an infectious lesion on the extremity involved. If the lymphadenitis is caused by mastitis, there should be a breast discharge or extreme tenderness and enlargement of the breast. Mammography should be done in cases of unilateral axillary masses that suggest lymphadenopathy. In the final analysis, a biopsy of the mass may need to be done to make the diagnosis. Babinski’s sign of acute onset is because of trauma or vascular diseases in most cases. If there is fever, one should consider an infectious process, most likely a cerebral abscess. Unilateral Babinski’s signs suggest a space-occupying lesion of the brain such as hematoma, abscess, or tumor. If Babinski’s signs are bilateral, it may be because of a toxic or degenerative condition of the brain such as encephalitis. It may also be because of a spinal cord tumor or other space-occupying lesion of the spinal cord. If there is associated central facial palsy on the ipsilateral side, one should consider an infarct or a space-occupying lesion of the opposite cerebral hemisphere. If there are cranial nerve signs aside from a facial palsy, one should consider a brain stem lesion, especially if they are contralateral. Babinski’s sign with hypoactive reflexes, if it is of acute onset, would be considered a traumatic or vascular lesion of the brain if it is unilateral and an acute vascular or traumatic lesion of the spinal cord if it is bilateral. Hypoactive reflexes of relatively insidious onset should make one think of pernicious anemia or Friedreich’s ataxia. Unilateral hyperactive reflexes of the upper and lower extremity with cranial nerve signs should bring to mind middle cerebral artery thrombosis or hemorrhage, carotid stenosis, and a space-occupying lesion of the brain. Hyperactive reflexes of the upper and lower extremities with no cranial nerve signs should suggest a high spinal cord tumor or a herniated cervical disk, especially if it is unilateral. Unilateral hyperactive reflexes of the lower extremity only would suggest an anterior cerebral artery thrombosis or parasagittal meningioma. Hyperactive reflexes of all extremities with cranial nerve signs should suggest a basilar artery thrombosis, brain stem tumor, or other lesion of the brain stem. Weakness and hyperactive reflexes of all four extremities without 97 cranial nerve signs and without any sensory changes should suggest a primary lateral sclerosis, although multiple sclerosis may occasionally present in this manner. Hyperactive reflexes with sensory changes confined to the trunk and extremities would make one think of a spinal cord lesion such as multiple sclerosis, pernicious anemia, or Friedreich’s ataxia, and, especially if it is unilateral, one would consider a space-occupying lesion of the spinal cord. Other considerations are transverse myelitis and anterior spinal artery occlusion. This is an important question to ask, as this would suggest a spinal cord tumor of the thoracic level or a parasagittal meningioma. The association of radicular pain in the cervical or thoracic area would make one think of a spinal cord tumor or other space-occupying lesions of the spinal cord. The finding of fever along with a unilateral Babinski’s sign should make one think of a cerebral abscess or an epidural abscess somewhere in the spinal column. The finding of fever with bilateral Babinski’s signs should make one think of encephalitis, particularly if there are disturbances of consciousness. However, fever may be associated with a cerebral vascular accident, so don’t be misled. The diagnostic workup depends on other symptoms and signs that help the physician determine what level the neurologic lesion might be. If there is an acute unilateral Babinski’s sign with hemiplegia and cranial nerve signs, a space- occupying lesion or vascular lesion of the brain must be considered. A spinal tap would not be done if there is any possibility of increased intracranial pressure. If a cerebral vascular disease is suspected, then a source for an embolism should be looked for. The fact that Babinski’s sign is a definite sign of neurologic disease is reason enough to call a neurologic specialist in before undertaking any diagnostic studies. Following the algorithm, you find there is no history of trauma, fever, or chills. The pain radiates down the back of both legs and he has had difficulty with urination for the past month. Your examination shows a suprapubic mass, a small nodule of the right lobe of the prostate, saddle hypesthesia and hypalgesia, and absent Achilles reflexes bilaterally. The suprapubic mass disappears after you catheterize him and remove 625 mL of urine. If it is of acute onset, one must consider the possibility of epidural abscess, pyelonephritis, or other abdominal conditions as the cause of the back pain. If it is of gradual onset, one should consider that it may be a tumor, particularly of the spinal cord or cauda equina, a pelvic tumor, or an aortic aneurysm that is compressing one of the nerve roots. In addition, chronic conditions such as lumbar spondylosis, rheumatoid spondylitis, and prostatitis must be considered. If there is a history of trauma, one should consider a compression fracture of the spine, a sprain or herniated disk, as well as spondylolisthesis. Without a history of trauma, one should consider a tumor, herpes zoster, or dissecting aneurysm. Lumbar spondylosis might be silent for a while only to cause pain after a significant traumatic event. Radiation of the pain would certainly be more likely to signify a space-occupying lesion of the spinal column such as a tumor, an epidural abscess, or a herniated disk. If there is no radiation, one would consider osteoarthritis or lumbar spondylosis and rheumatoid spondylitis. If there are, then one must consider the possibility of a spinal cord tumor, cauda equina tumor, or kidney disease. With the patient standing straight and one of your hands on his shoulder and the other on the opposite hip, rotate his body. At least one-fourth of the patients with back pain have one leg shorter than the other. A sedimentation rate and arthritis panel should be done if rheumatoid arthritis is suspected. It is very important to get anteroposterior (A-P) views, as well as oblique and lateral views. At this point, it is wise to observe the results of conservative therapy before ordering expensive diagnostic tests.
Pressure on the hernia induces a desire for micturition particularly when it is distended order cheap ceftin online virus 3 game online. That means its contents can be returned into the abdominal cavity ceftin 500mg cheap virus 101, but the sac remains in its position purchase ceftin with mastercard antibiotic resistance in agriculture. Various causes of irreducibility are :— (i) adhesion of its contents to each other, (ii) adhesion of its contents with the sac, (iii) adhesion of one part of the sac to the other part, (iv) sliding hernia and (v) very large scrotal hernia (scrotal abdomen). Clinically a strangulated hernia is also irreducible, but it is extremely tender and tense and the overlying skin may be red. It must be remembered that there is no interference with the blood supply to the intestine in this hernia. One must be very careful to make this diagnosis, as strangulated hernia also possesses two of its features i. Of course the third and most important feature of a strangulated hernia is missing in this hernia i. Strangulated hernia (irreducibility+obstruction+arrest of blood supply to the contents). Diagnosis of strangulation is made when a hernia is irreducible, without any impulse on coughing, extremely tense and tender. Diagnosis is made by the presence of constitutional disturbances associated with local signs of inflammation — overlying skin becomes red and oedematous and the swelling becomes painful, tender and swollen. The only differentiating feature from a strangulated hernia is that this hernia is not tense and is not associated with intestinal obstruction. A large globular hernia when descends well into the scrotum this condition is suspected. This condition may be associated with strangulated small intestine within its sac or a strangulated large intestine outside the sac. The loop in the circumference of the bowel becomes The thick line represents abdomen is always found strangulated. This condition often the peritoneum, Note that at a more advanced stage complicates a femoral hernia and the colon forms the wall of strangulation than the rarely an obturator hernia. The patient may or may not vomit, intestinal colic is present but the bowels are opened normally. The loop within the abdomen becomes first strangulated and can only be suspected when tenderness is elicited above the inguinal ligament along with presence of intestinal obstruction. The hernia actually comes out superficially through the saphenous opening situated Wi inches below and lateral to the pubic tubercle. When the hernia is within the femoral canal it remains narrow, but once it escapes through the saphenous opening into the loose areolar tissues, it expands considerably. Femoral Femoral Nerve Femoral Artery Femoral Vein hernia is commoner in FttiMraiRing women (2 : 1). But the Lacunar ligament students must remember that even in women the Superficial commonest hernia in the Inguinal Ring groin is the inguinal! The right side is affected twice as common as the left side and in 20 per cent of cases the condition is bilateral. One thing must be borne in mind that the femoral canal being a rigid opening this hernia becomes strangulated very often. Similarly a Inferior Epigastric Vessels Femoral Nerve femoral hernia can be prevented from coming out by Femoral Ring through which Femoral pressure applied over the Hernia Comes out femoral canal or the saphenous Obturator Nerve External Iliac Vessels opening. The so called impulse on coughing is present in this condition as well, but it is actually a fluid thrill and not an expansile impulse to the examining fingers. The track of the psoas abscess from the caries spine upwards to the saphena varix felt by the fingers is shown in the figure. Sometimes that femoral hernia lies on the medial side of a venous hum can be heard when the the femoral vessels. The gland of Cloquet lying within the femoral canal may be enlarged and simulates exactly an irreducible femoral hernia. If any focus cannot be Pectineus Muscle found out or any cause of Superior Ramus of Pubis enlargement of lymph nodes cannot be detected, the Fig. It is a painless swelling and if the pulsation of the femoral artery can be palpated it will be appreciated that the swelling is lateral to the artery. Sometimes there is an iliac part of the abscess which is determined by cross-fluctuation. Examinations of the back and corresponding iliac fossa including X-rays clarify the diagnosis. Presence of osteoarthritis in the hip joint, a cystic swelling, absence of impulse on coughing and that the swelling diminishes in size during flexion of the hip joint are the diagnostic points in favour of this condition. The neck of the hernia is generally wide and hardly gives rise to intestinal obstruction or strangulation. The main diagnostic features are — (i) Bulge through the centre of the umbilical scar everting the whole umbilicus; (ii) Age of the patient; (iii) The swelling is easily reducible (spontaneously reduced when the child lies down) and there is definite impulse on crying; (iv) The size of the hernia varies — it may be a small defect admitting the tip of the little finger alone to quite a large opening admitting two or three fingers; (v) The content is usually small intestine, so resonant to percussion; (vi) About 90% of these herniae disappear spontaneously during the first 5 years of life as the umbilical scar thickens and contracts. It is very rare in comparison to the para-umbilical hernia which is described below. Almost invariably it is due to raised intra-abdominal pressure which has forced the hernia through the umbilical scar. One must try to find out the cause of raised intra-abdominal pressure in these cases. Common causes are — pregnancy, ascites, bowel distension, ovarian cyst and fibroid. The usual site is just above the umbilicus between the two recti, in fact lower half of the fundus of the sac is covered by the umbilicus. The diagnostic features are as follows : (i) Para-umbilical hernia develops in the middle and old age; (ii) Obese women are more commonly affected; (iii) Usual symptoms are pain and swelling. If the swelling is very small, it may not be noticed by the patient and the pain and discomfort become the main symptoms; (iv) The surface is smooth and the edge is distinct except when the patient is very fat; (v) It contains omentum or bowel. The lump is soft and resonant to percussion when the content is bowel; (vi) Many paraumbilical herniae are irreducible when the contents become adherent to the sac or the neck of the sac becomes narrow. If the hernia can be reduced, the firm fibrous edge of the defect in the linea alba can be felt; (vii) As the defect in the linea alba is firm and does not enlarge proportionately these herniae do give rise to intermittent abdominal pain, though strangulation is not common. This defect is usually placed somewhere between the xiphisternum and the umbilicus. So whenever a patient will complain of epigastric discomfort or pain palpate the abdominal wall first to detect a small lump of epigastric hernia. It must be remembered that usually these herniae do not have impulse on coughing and cannot be reduced. That the swelling cannot be moved over the underlying structures favours the diagnosis of epigastric hernia. By repeated contractions of the flat muscles of the abdomen the two recti show tendency to diverge particularly when the linea alba is weak. In this condition the hernial sac passes between the layers of the anterior abdominal wall. There is another superior lumbar triangle being bounded by the 12th rib above, by the sacrospinalis medially and the posterior border of the internal oblique laterally. Incisional lumbar hernia may follow an operation on kidney, the incisional wound being infected.
This usually consists of adenomas of other endocrine glands purchase cheap ceftin online virus film, such as pituitary discount ceftin uk antibiotic resistance rates, pancreatic islets (Beta cells) order ceftin without a prescription taking antibiotics for sinus infection, parathyroid and adrenal cortex. But another condition with polyendocrine adenomas and peptic ulceration often have giant gastric rugae. Abnormally located peptic ulcers in the distal portions of the duodenum and jejunum occur in 25% of cases. Diarrhoea is often caused by high volume of acid alongwith neutralization of pancreatic enzymes causing steatorrhoea-type diarrhoea. The overnight resting secretion often contains 200 to 300 mEq of free hydrochloric acid. Another important feature is that the secretory rate is already close to its maximum and further stimulation with histamine generally produces very little response, that means basal secretion is quite high almost reaching the maximal secretion. A ratio of basal acid output to maximal output (histamine-stimulated) is greater than 60% and this is almost diagnostic of Zollinger-Ellison syndrome. Gastric hypersecretion is associated with distressing watery diarrhoea in about l/3rd of cases. About 2 to 8 litres of liquid stool daily has been reported and may precede the onset of peptic ulceration. Steatorrhoea may also occur, either due to inactivation of pancreatic enzymes in abnormally acid environment in duodenum or due to irritative action of acid on the mucosa of the small bowel. Diagnosis of gastrinoma is mainly by suspicion and by measurement of serum gastrin. When the serum gastrin level is not elevated to a great extent, the case may be diagnosed by gastric pH analysis followed by a secretin test. This test is accomplished by measuring basal serum gastrin level and then injecting 2 units of secretin per Kg of body weight followed by measurements of serum gastrin level at various periods upto 1 hour. Patients with this disease will show an abnormal elevation of serum gastrin level whereas normal patients should have no change or a reduction in serum gastrin level following intravenous secretin injection. Medical management consists of high dose of H antagonist or omeprazol to control the ulcer disease. Partial venous sampling for gastrin is occasionally successful to localise intraoperatively the gastrinoma. Majority of the gastrinomas exist in the head of the pancreas in the gastrinoma triangle formed by an apex is at the cystic duct-common duct junction and base is formed by the third part of the duodenum. After opening the abdomen the transverse colon is completely mobilised to expose the entire surface of the pancreas. Kocher’s manoeuvre is performed to mobilise the duodenum and to facilitate the palpation of the pancreas. Intraoperative ultrasonography may be used at this stage to localise the lesion particularly in the head of the pancreas. The lymph nodes around should be biopsied, as solitary gastrinomas are sometimes found in these lymph nodes. If ultrasonography fails to detect the gastrinoma, a pyloroplasty is made and the duodenal wall is palpated through the lumen to localise isolated duodenal gastrinomas. Only in case of multiple lesions in the head of the pancreas, a Whipple resection (Pancreaticoduodenectomy) is necessary. If no lesion is detected, or in whom the disease is multicentric or metastatic, a palliative ulcer operation in the form of truncal vagotomy and pyloroplasty should be performed. Some surgeons even prefer to do highly selective vagotomy, but scarring at the lesser curvature following this operation may lead to difficulty in performing subsequent gastrectomy. Only on rare occasions total gastrectomy is required, who do not respond to medical therapy and in whom proper localisation of tumour is not possible. Diarrhoea is usually profuse averaging 4 to 5 litres per day and contains 200 to 400 mEq of potassium daily. The most likely explanation for the symptoms is the secretion of vasoactive intestinal peptide, pancreatic polypeptide, gastrointestinal inhibitor peptide and secretin. About 40% are benign tumours, 40% are malignant tumours usually with metastases and 20% are hyperplasia of these cells of the islets. Primary infection is usually due to Bovine strain of Mycobacterium tuberculosis and results from ingesting infected milk. This produces hyperplastic tuberculosis and occurs most commonly in the ileo-caecal region, although solitary or multiple lesions of the lower ileum may be present. The more common form ulcerative tuberculosis is secondary to pulmonary tuberculosis and arises as a result of swallowing tubercle bacilli. In Western Countries all cases are due to ingestion of mycobacterium tuberculosis bovis, whereas in Eastern Countries, like India, Pakistan, Bangladesh etc. Infection first starts in the lymphoid follicles and spreads to the submucous and subserous planes. This thickening is partly due to tubercular granulation tissue and oedema, but is mostly due to excess fibrous tissue. Unlike the ulcerative variety, there is no ulceration and unlike regional ileitis abscess formation and fistula are not seen. Microscopically, tubercular lesions are seen as usual with more lymphocytes and more fibrosis. This is due to narrowing of the lumen of the involved segment and sometimes enterolith may impact within the narrowed segment to cause acute intestinal obstruction. Attacks of abdominal pain off and on due to subacute intestinal obstruction are often the first symptom. This may be associated with intermittent diarrhoea (alternate constipation with pain and diarrhoea). Features of blind-loop syndrome’ may develop due to stasis, distension and chronic infection in the segment of ileum proximal to obstruction. Anaemia(due to vitamin B12 deficiency), loss of weight and steatorrhoea are the features of ‘blind-loop syndrome’. This is rather confusing as one must exclude Crohn’s disease, actinomycosis and carcinoma of the caecum. Barium meal radiography will reveal (i) persistent narrowing of the affected segment i. The ileum may drop down almost vertically from the caecum to make the ileo-caecal angle about 180°. Treatment— (a) When the diagnosis is definite and there is no intestinal obstruction the treatment is antitubercular chemotherapy with sanitary regime. Right hemicolectomy with removal of the diseased segment is the treatment of choice. In the terminal ileum there are multiple ulcers, the long axes of which lie transversally (cf.

Postprandial belching ceftin 250mg lowest price virus zombie movies, often described as flatulant dyspepsia purchase ceftin australia global antibiotic resistance journal, is also a common symptom of this condition buy ceftin amex antibiotics quizlet. Attacks of pain are irregular lasting for weeks or months or pain free intervals of varying length. Jaundice is not a sign of cholecystitis although a slight icteric tinge may be present due to associated cholangitis. In majority of cases the gallbladder is not palpable unless a mucocele or empyema develops. The various modes of X-ray are quite confirmatory and have already been discussed under the heading of "Special Investigations". This results from obstruction to the common bile duct due to infestation by the Chinese liver flukes (Clonorchis Sinensis). The patient never presents before six months of age and about half of the cases present only in adult life. Abdominal pain is the main presenting symptom which starts in the epigastrium and tends to pass through to the back. The pain is often quite intolerable which becomes slightly relieved when the patient sits up. Jaundice is present in less than 20% of cases but diabetes is more common (about 1/3 of cases). Best way to palpate the pancreas is to turn the patient to the right and hips and knees are flexed. Intermission may be seen in cases of carcinoma of the ampulla of Vater due to sloughing of the growth. The pale stools are quite common upper figure one can see a mass in the head of the and steatorrhoea from enzyme deficiency is pancreas near ampulla of Vater with dilated pancreatic also a feature of this condition. So old patients when present with these symptoms one should investigate thoroughly to exclude carcinoma of the pancreas. The peculiar feature of the pancreatic pain is that it passes through to the back. It is aggravated when the patient lies down and lessened when he sits up so the patient often spends the night sitting up with his arms folded across the chest. Thrombophlebitis migrans may be an indication of the presence of pancreatic carcinoma. Thrombophlebitis which appears spontaneously and resolves only to appear again elsewhere is the type one often comes across. A vague pain in the abdomen which is more often complained at the right iliac fossa is probably the earliest symptom in majority of cases. Scalding pain on micturition or pain which mimics ureteric colic is often complained of. Perianal lesions such as abscesses, fissure and fistulae are quite common in this condition. The clinical picture is best considered in 4 stages : (1) the inflammatory stage, when a mass is palpable in the right iliac region; (2) the colitis stage, when diarrhoea, fever, anaemia and loss of weight are present; (3) the stenotic stage, when the picture of small gut obstruction supervenes and (4) the fistula stage, either external or internal — communicating with the sigmoid colon, bladder, caecum, etc. Differentiation from an appendicular lump is made by the absence of origin of pain in the umbilical region, insidious onset and presence of occult blood in stool. If the condition has involved the colon, in barium enema a coarse cobblestone pattern may be present but it is often difficult to differentiate this from pseudopolyposis of ulcerative colitis. Sometimes abdominal lump may be present due to peri-colonic thickening or infection. This type of fistula formation is never found in ulcerative colitis though occasionally seen in diverticulitis. Rectal bleeding is less frequent than that in ulcerative colitis and diverticulitis. In contradistinction to ulcerative colitis, rectum is involved in only half the cases, so in sigmoidoscopy normal rectal mucosa does not exclude this condition. The mucosa when affected shows oedematous swelling, granularity and scattered small ulcers with normal mucosa in between (cf. Systemic disorders like erythema nodosum, synovitis, iritis and minor septic skin conditions may be seen with this condition. Loss of weight and diarrhoea with fetid odour stools containing pus and occult blood are complained of. Barium meal follow-through may demonstrate non-filling or inadequate filling of terminal ileum, caecum and proximal part of ascending colon due to narrowing and hypermotility of the ulcerated segment. There are various types of presentation of this disease — (a) As a cause of abdominal pain. Enlarged lymph nodes may be palpable as firm, discrete, round nodules on the right of the umbilicus, (b) As a cause of general symptoms. These diverticula are due to excessive intracolonic pressure from thickened circular fibres which interdigitate with each other. This leads to excessive segmentations and an increase in the intracolonic pressure. Inflammation usually starts at the wall of the diverticulum and spreads in the pericolic tissue and mesenteric fat. This bleeding may be profuse and occurs due to trauma round the neck of the diverticula when it steps in and out through the defect in the muscle under varying degree of intra-luminal pressure, ft must be remembered that profuse rectal bleeding in the elderly is more often due to diverticular disease than carcinoma. Appearance of symptoms suggests that diverticulosis has progressed to diverticulitis. Intermittent abdominal pain especially in the left iliac fossa with flatulence and slight distension are the characteristic features of this condition. The pain may be due to over distension of an isolated section of the colon or due to a small localized abscess. The patient passes small, pebbly motion which may be accompanied by blood and/or mucus. The result of perforation may be anything from small localized abscess (commoner) to general peritonitis. This localized abscess may be absorbed on its own by conservative treatment or may become adherent to the bladder or another loop of bowel forming a vesico-colic or entero- colic fistula. It is difficult or may be impossible to pass the sigmoidoscope beyond the recto-sigmoid junction due to excessive spasm of the sigmoid colon. Barium meal follow through or barium enema may be helpful in diagnosing this condition. In infective stage it shows a straight sigmoid colon without much convolutions and sacculations. The pathology starts in the distal rectum and spreads to a variable distance proximally and even may spread into the small intestine. This leads to inability of the bowel to adequately contract which leads to failure in peristalsis. It shows a familial tendency and mostly occurs in the first year of life commonly within 3 days following birth.
Ceftin 250mg with amex. Air Conditioner Cleaning Indoor and Outdoor Unit Using Nu-Calgon Coil Cleaner.