
Princeton University. G. Lee, MD: "Purchase cheap Synthroid online no RX - Cheap Synthroid online OTC".
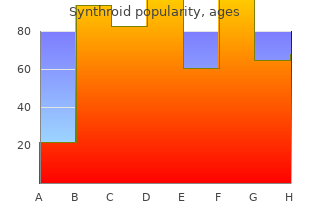
Feeding fuids with dextrose discount 75 mcg synthroid with amex symptoms 3 weeks into pregnancy, or octreotide are all adequate options for this purchase 50mcg synthroid otc symptoms of mono, with two or all three sometimes required purchase 50mcg synthroid with mastercard symptoms 0f diabetes. Symptoms of hypoglycemia are due to both the effects on the brain and a refex sympathetic surge. Neurological effects include confusion, altered mental sta- tus, agitation, unresponsiveness, and symptoms that may mimic acute stroke such as focal neurological defcits. Peripheral effects due to a sympathetic out- put of catacholamines cause anxiety, irritability, vomiting, palpitations, tremor, and sweating. One amp of D50 is about 100 calories, which is insuffcient to maintain adequate blood glucose beyond a few minutes. Rapid blood glucose determination is essential in all patients with altered men- tal status. The elderly and severely malnourished (ie, alcoholics) can present with hypo- glycemia in the absence of sympathetic signs or even awareness of hypoglyce- mia, often mimicking intoxication, unresponsiveness, or stroke. They had arrived 2 days before to go skiing for the week and the symptoms started yesterday morning after waking up. This morning, they were planning to go skiing but the patient complained of worsening headache and unsteadiness; no chest pain, shortness of breath, palpita- tions, vomiting, diarrhea, fever, or blurry vision. Nobody else with similar symp- toms; arrived yesterday to the mountains by helicopter, ascended 10 000 feet. Social: lives with wife at home, smokes one pack of cigarettes a day for 20 years, denies alcohol, drugs, not sexually active; works as an investment banker g. Travel history: arrived yesterday to the mountains by helicopter, ascended 10 000 feet G. Eyes: extraocular movement intact, pupils equal, reactive to light, no papille- dema on fundoscopic examination d. Neuro: intact refexes throughout, ataxic on tandem gait, poor fnger to nose, positive Romberg’s test, no focal weakness, no sensory defcit p. Our patient pres- ents with fu-like symptoms a day after rapid ascent to a mountain by heli- copter, commonly seen with acute mountain sickness. The history of being there to ski can be given early but the candidate must ask specifc questions on how he got there to illicit the history of rapid ascent. Important early actions include early recognition, treatment with oxygen, steroids, and acet- azolamide, and rapid decent. If there is early recognition and management, the patient will do well and will be stable for transferred. High altitude illness typically occurs within the frst 48 hours after rapid ascent above altitudes of 2500 m. Patient appears stated age, speaking in full sentences, nauseous, and inattentive. Patient’s wife states that her husband is increasingly confused at home over the past few days and had been complaining of weakness, dizziness, and nausea. He has also been stating that things look funny (if asked, states “things have yellowish hue”). Patient denies chest pain, shortness of breath, fever, cough, urinary symptoms, headache, or pain; baseline mental status is good and he is able to go to the store on his own. He was placed on erythromy- cin several days ago for bronchitis that has now resolved. Social: lives with wife at home, leaving apartment less these days, denies alco- hol, smoking, drugs, not sexually active 272 Case 63: Altered Mental status Figure 63. Extremities: full range of motion, no deformity, normal pulses, 1+ pitting edema Case 63: Altered Mental status 273 n. Digibind 6 vials over 30 minutes (if digiband not given, patient will continue to be bradycardia and more confused) b. This is a case of chronic digoxin (digitalis) toxicity from new renal insuffciency and new antibiotic. Digoxin is heart medicine used to control irregular cardiac rhythms which, in excess, can lead to life threatening abnormalities in heart con- duction. The patient presents with nonspecifc complaints of nausea, confusion, and dizziness but also has disturbances in color vision that can occur with digoxin toxicity. The candidate should initially cast a broad differential to exclude causes of altered mental status such as low blood sugar, myocardial infarctions, and infection. A thorough history should illicit digoxin as a medication and a level should be ordered. As the case continues, the patient will become more brady- cardic and hypotensive complaining of dizziness and sweating. At this time, the patient should be empirically treated with the antidote, digibind. Symptoms may be nonspecifc including weakness, dizziness, shortness of breath, confusion, disturbances in color vision (yellow-green tendency), nau- sea, vomiting, and headache. Digoxin level does not necessarily correlate with toxicity, especially in chronic toxicity. There are three methods for calculating the appropriate dose of digibind in the settings of digoxin toxicity. Which method used depends on whether the ingestion is acute or chronic, and whether the amount ingested or a serum level is known. In acute life 276 Case 63: Altered Mental status Case 64: shortness of Breath threatening dysrhythmias where no information is available, 10 vials of digibind should be administered for acute overdose, and 4-6 vials for chronic ingestion. Patient appears stated age, uncomfortable, sitting upright to breathe, cannot speak in full sentences, and diaphoretic. She also stopped leaving apartment (patient lives on the third foor of walk-up, and cannot walk up stairs without becoming short of breath); denies nausea, vomiting, leg swelling, cough, fever, or chest pain. The patient was given 1 sub- lingual nitroglycerine, oxygen, and 40 mg of furosemide. Social: lives with husband at home, leaving apartment less these days, denies alcohol, smoking, drugs, not sexually active g. Heart: tachycardia, regular rhythm, no murmurs, rubs, or gallops 278 Case 64: shortness of Breath Figure 64. Extremities: full range of motion, no deformity, normal pulses, 2 + pitting edema o. This is a condition in which fuid leaks into the lung tissue because of poor heart function leading to diffculty breathing. If nitrates are started (either high-dose intrave- nously or multiple sublingual doses) the patient will do well. If no nitrates are given or only in small doses, the patient will continue to worsen and require 280 Case 64: shortness of Breath Case 65: shortness of Breath intubation. Patients will often present with diffculty in breathing on exertion, such as dif- fculty climbing stairs or walking. Physical fndings include pitting edema, crackles, wheezing (although “not all that wheezes is asthma”), jugular venous distension, S3 or S4 on cardiac examination. Treatment includes preload reduction with nitroglycerin and diuresis as well as ventilator support. Patient appears stated age, lethargic, tachypneic, mild intercostal and subcostal retractions.
Revised interim guidelines on confidentiality for police surgeons in England buy 125 mcg synthroid mastercard treatment urinary incontinence, Wales and Northern Ireland cheap 200 mcg synthroid amex treatment 6th feb. Association of Police Surgeons (now the Association of Forensic Physi- cians) effective 25 mcg synthroid medicine keychain, East Kilbride. The Stationery Office, London, 1999; and on the Department of Constitutional Affairs (formerly Lord Chancellor’s Department). Sexual Assualt Examination 61 Chapter 3 Sexual Assault Examination Deborah Rogers and Mary Newton 1. All health professionals who have the potential to encounter victims of sexual assaults should have some understanding of the acute and chronic health problems that may ensue from an assault. However, the pri- mary clinical forensic assessment of complainants and suspects of sexual assault should only be conducted by doctors and nurses who have acquired specialist knowledge, skills, and attitudes during theoretical and practical training. There are many types of sexual assault, only some of which involve pen- etration of a body cavity. This chapter encourages the practitioner to under- take an evidence-based forensic medical examination and to consider the nature of the allegation, persistence data, and any available intelligence. The chapter commences by addressing the basic principles of the medical examination for both complainants and suspects of sexual assault. Although the first concern of the forensic practitioner is always the medical care of the patient, thereafter the retrieval and preservation of forensic evidence is para- mount because this material may be critical for the elimination of a suspect, identification of the assailant, and the prosecution of the case. Thus, it is imper- ative that all forensic practitioners understand the basic principles of the foren- sic analysis. Thereafter, the text is divided into sections covering the relevant body areas and fluids. Each body cavity section commences with information regard- From: Clinical Forensic Medicine: A Physician’s Guide, 2nd Edition Edited by: M. This specialist knowledge is manda- tory for the reliable documentation and interpretation of any medical findings. The practical aspects—which samples to obtain, how to obtain them, and the clinical details required by the forensic scientist—are then addressed, because this takes priority over the clinical forensic assessment. The medical findings in cases of sexual assault should always be addressed in the context of the injuries and other medical problems associated with con- sensual sexual practices. Therefore, each section summarizes the information that is available in the literature regarding the noninfectious medical compli- cations of consensual sexual practices and possible nonsexual explanations for the findings. The type, site, and frequency of the injuries described in asso- ciation with sexual assaults that relate to each body area are then discussed. Unfortunately, space does not allow for a critical appraisal of all the chronic medical findings purported to be associated with child sexual abuse, and the reader should refer to more substantive texts and review papers for this infor- mation (1–3). Throughout all the stages of the clinical forensic assessment, the forensic practitioner must avoid partisanship while remaining sensitive to the immense psychological and physical trauma that a complainant may have incurred. Although presented at the end of the chapter, the continuing care of the com- plainant is essentially an ongoing process throughout and beyond the primary clinical forensic assessment. Immediate Care The first health care professional to encounter the patient must give urgent attention to any immediate medical needs that are apparent, e. Nonetheless, it may be possible to have a health care worker retain any clothing or sanitary wear that is removed from a complainant until this can be handed to someone with specialist knowledge of forensic packag- ing. Timing of the Examination Although in general terms the clinical forensic assessment should occur as soon as possible, reference to the persistence data given under the relevant sections will help the forensic practitioner determine whether the examination of a complainant should be conducted during out-of-office hours or deferred Sexual Assualt Examination 63 until the next day. Even when the nature of the assault suggests there is unlikely to be any forensic evidence, the timing of the examination should be influenced by the speed with which clinical signs, such as reddening, will fade. Place of the Examination Specially designed facilities used exclusively for the examination of com- plainants of sexual offenses are available in many countries. The complainant may wish to have a friend or relative present for all or part of the examination, and this wish should be accommodated. Suspects are usually examined in the medical room of the police station and may wish to have a legal representative present. During the examinations of both complainants and suspects, the local ethical guidance regarding the conduct of intimate examinations should be followed (4). Consent Informed consent must be sought for each stage of the clinical forensic assessment, including the use of any specialist techniques or equipment (e. When obtaining this consent, the patient and/or parent should be advised that the practitioner is unable to guarantee confidentiality of the material gleaned during the medical examination because a judge or other presiding court officer can rule that the practitioner should breach medical confidentiality. If photo documentation is to form part of the medical examination, the patient should be advised in ad- vance of the means of storage and its potential uses (see Subheading 2. Details of the Allegation If the complainant has already provided the details of the allegation to another professional, for example, a police officer, it is not necessary for him or her to repeat the details to the forensic practitioner. Indeed, Hicks (5) notes that attempts to obtain too detailed a history of the incident from the complainant may jeopardize the case at trial because at the time of the medical examination the patient may be disturbed and, consequently, the details of the incident may be confused and conflict subsequent statements. The details of the allegation can be provided to the forensic practitioner by the third party and then clarified, if necessary, with the complainant. It may be difficult for the complainant to describe oral and anal penetrative sexual assaults, and the forensic practitioner may need to ask direct questions regarding these acts sensitively (6). Medical and Sexual History The purpose of obtaining the medical and sexual history is essentially twofold: first, to identify any behavior or medical conditions that may cause the doctor to misinterpret the clinical findings, for example, menstrual bleed- ing; and second, to identify any medical problems that may be attributable to the sexual assault, for example, bleeding, pain, or discharge. Other specific details may be required if emergency contraception is being considered. When children are examined, the parent or caregiver should provide comprehensive details of the past medical history. When adults are exam- ined, only relevant medical and sexual history should be sought because confidentiality cannot be guaranteed. What constitutes relevant medical his- tory must be determined on a case-by-case basis by considering the differ- ential causes for any medical findings and the persistence data for the different sexual acts. Forensic practitioners should not ask suspects about the alleged incident or their sexual history. General Examination In all cases, a complete general medical examination should be conducted to document injuries and to note any disease that may affect the interpretation of the medical findings. Anogenital Examination Whenever there is a clear account of the alleged incident, the anogenital examination should be tailored to the individual case (e. However, in some cases, the complainant may not be aware of the nature of the sexual assault. Further- more, children and some adults may not have the language skills or may feel unable to provide a detailed account of the sexual acts at the initial interview. In such cases, a comprehensive anogenital examination should be undertaken if the patient or the person with legal authority to consent on behalf of the patient gives his or her consent. Ownership and Handling of Photo Documentation Any video or photographic material should be retained as part of the practitioner’s confidential medical notes and stored in a locked cabinet a locked premises.