
Azusa Pacific University. M. Kan, MD: "Order cheap Zyprexa online no RX - Trusted online Zyprexa".
Dacie & Lewis Practical Haematology buy cheap zyprexa 7.5 mg symptoms 7 days after embryo transfer, 9th edn buy zyprexa discount medicine pills, Edinburgh: Churchill livingstone 20mg zyprexa for sale holistic medicine, 2001. However, we have provided the more important tests in current use which include: • Blood group and antibody screen. Safe transfusion practice Each year, patients are transfused with the wrong blood. However, it is also clear that delay in appropriate transfusion also contributes to mortality. A common error is clerical and generally involves the cross-matched sample being taken from the wrong patient, and so the compatibility test is performed on the wrong sample. Occasionally, the staf carrying out the transfusion connect the blood up to the wrong patient. How to minimize errors • First, ask yourself, ‘Does this patient really need to be transfused with blood or blood products (e. Use clinical judgement in helping decide whether or not to proceed with transfusion. Many transfusion laboratories insist on 1, 2, 5, 6, and 7, and either 3 or 4 from: 1. If this sounds cumbersome and bureaucratic Remember many people die annually because they are transfused with the wrong blood. In most cases, clerical error is to blame—people have flled out bottles in advance and failed to check patient identity. If the temperature rises to above 39°C or >2°C from baseline, with other signs/symptoms, consider bacterial contamination and monitor the patient carefully. Immediate transfusion reaction or bacterial contamination of blood If predominantly extravascular, may only sufer chills/fever 1h after starting transfusion—commonly due to anti-D. Mechanism Complement (C3a, C4a, C5a) release into recipient plasma l smooth muscle contraction. Initial steps in management of acute transfusion reaction • Stop blood transfusion immediately. Urgent investigations your local blood transfusion department will have specifc guidelines to help you with the management of an acute reaction. The following guide lists the samples commonly required to establish the cause and severity of a transfusion reaction (see Box 3. If you are uncertain about the labora- tory procedure or management of a patient who appears to have sufered a severe reaction, you must notify your hospital’s haematology medical staf who will provide advice. Mainly due to anti-HlA (human leu- cocyte antigen) antibodies in recipient serum or granulocyte-specifc anti- bodies (e. Check the compatibility label of the blood unit matches with the patient’s identity band, forms, and case notes. If mistake found, tell the blood bank urgently—the unit of blood intended for your patient may be transfused to another patient. Implicated organisms include Gram −ve bacteria, including Pseudomonas, Yersinia, and Flavobacterium. Background If an Rh (D) −ve mother has a baby that is Rh (D) +ve, she may develop antibodies (maternal anti-D) against fetal red cells. This may result in fetal red cell destruction termed rhesus haemolytic disease of the newborn, a seri- ous haemolytic disorder that is seen less today due to a greater understand- ing of the underlying mechanism and our ability to prevent it. The Kleihauer test should be performed on all Rh (D) −ve women who deliver an Rh (D) +ve infant. Fetal cells appear as darkly staining cells against a background of ghosts (these are the maternal red cells). An estimate of the required dose of anti- D can be made from the number of fetal cells in a low-power feld. After this, you will need to calculate the dose of anti-D to give the mother, but if you are unsure, either discuss with the haematology medical staf or contact your local transfusion centre. The typical anaemia found in renal disease is a result of failure of Epo production. For example, in the assessment of polycythaemic states, an i Epo level may be appropriate (e. Tests for antiplatelet and antineutrophil antibodies These tests are usually requested by the haematology department for patients with either thrombocytopenia or neutropenia, respectively. These assays are used to detect the presence of specifc antibodies against platelet or neutrophil antigens on the cell surface. These are useful for detecting even weak antibodies or where there are only a few antigenic sites per cell. Elegant though these tests are, they are actually not useful in clinical prac- tice for the diagnosis of neutropenia or thrombocytopenia where the cause is autoimmune, since these are largely clinical diagnoses. Most cells will express many diferent proteins, and the pattern of expression allows cellular characterization. Using a panel of diferent antibodies, an immunophenotypic profle of a sample is determined. Immunophenotyping is used in conjunction with standard morphological analysis of blood and marrow cells. The antibodies are labelled with fuorescent markers, and binding to cell proteins is detected by laser. Oxford Handbook of Clinical Haematology, 2nd edn, Oxford: Oxford University Press, 2004. Clonality assessment Particularly useful in determining whether there is a monoclonal B-cell or plasma cell population. Guidelines on the use of multicolour fow cytometry in the diagnosis of haematological neo- plasms. Chromosome abnormalities may be constitutional (inherited) or acquired later in life. Cytogenetic analysis of chromosome structure and number has been used for many years for the study of disorders such as Down’s syndrome. Acquired chromosomal abnormalities are found in malignancies, especially haematological tumours. The analysis and detection of cytoge- netic abnormalities is known as karyotyping. Because of the complexity of this subject area, we will concentrate on two main areas where chromo- some analysis is of value. Cytogenetic assays are expensive (around £250 for a leukaemia or lym- phoma karyotype), and if there is any doubt as to whether the test is indi- cated, we would suggest you discuss the case with one of your seniors or the cytogenetics staf. Arranging karyotyping before or during pregnancy is generally carried out by the obstetrician in charge of the woman’s care. Pre-implantation genetic diagnosis allows abnormalities to be detected even before implantation has occurred.
Once metastatic to the liver generic zyprexa 10mg without a prescription medications blood donation, this neuroendocrine malignancy secretes numerous vasoactive substances (e generic 10mg zyprexa visa treatment 2nd degree heart block. Carcinoid valvular disease is characterized by thickened buy zyprexa 2.5 mg lowest price symptoms hiatal hernia, retracted, shortened, and even fixed tricuspid leaflets, causing a mixed picture of regurgitation and stenosis. Unless there is a significant right-to-left shunt (via an atrial septal defect or patent foramen ovale), the left-sided heart valves are usually spared, owing to the clearance of vasoactive substances by the lungs. Resting cardiac output may be markedly reduced and may fail to augment with exercise, due to limited right ventricular preload. Right upper-quadrant pain can result from high systemic venous pressure and concomitant hepatomegaly, ascites, and abdominal distention. Occasionally, patients will experience a fluttering discomfort in the neck, caused by the giant a waves transmitted to the jugular veins. Elevated central venous pressure may lead to marked hepatomegaly, ascites, and peripheral edema. In sinus rhythm, a giant a wave in the jugular venous pulse at the first heart sound (S ) results from impaired right atrial diastolic filling during1 atrial systole. Accentuation of the murmur intensity with inspiration (Rivero-Carvallo sign) or other preload augmenting maneuvers (e. Despite elevated neck veins and venous congestion, the patient may be comfortable lying flat due to the absence of pulmonary congestion. Nowadays, hemodynamic diagnosis is rarely required, as the diagnosis is usually apparent on Doppler echocardiography. Given the accuracy of modern echocardiographic techniques, cardiac catheterization can often be bypassed. Right heart catheterization can be used to confirm the diagnosis already suggested by Doppler echocardiography and can serve as a prelude to therapeutic balloon valvuloplasty. Simultaneous measurement of the right atrial and right ventricular pressures with dual catheters (or a dual-lumen catheter) enables the calculation of the diastolic pressure gradient (Fig. Maneuvers such as lifting the legs or administration of atropine may accentuate the gradient. The indications for surgery or balloon valvuloplasty are usually determined by the severity of concomitant mitral or aortic valve disease. Bioprostheses are favored when valve replacement is necessary at the tricuspid position, as mechanical prostheses are more prone to thrombosis at this location. The neck veins will show loss of the usual x wave and a prominent systolic wave, usually referred to as a cv wave, followed by a rapid y descent. This may be heard as an early diastolic rumble (short and low-pitched) along the left sternal border. A right-sided third or fourth heart sound (S or 4 S ) is often present along the left sternal border, which augments with inspiration. Systolic pulsation of the liver is often an associated physical finding, although this may be diminished once congestive cirrhosis develops. Vegetations are evident with endocarditis, and a flail valve leaflet may be seen with iatrogenic damage (e. Eccentric, wall-hugging jets should be typically upgraded by one grade, as is done for mitral regurgitation, because these are generally not visualized fully by echocardiography. If right ventricular failure develops, medical therapy should be targeted at diuretic therapy and afterload reduction, as in other heart failure states. Usually tricuspid repair or annuloplasty is favored over prosthetic implantation where this is feasible. The pulmonary valve is a trileaflet valve that separates the right ventricle from the pulmonary vasculature. Dysfunction of the valve can have adverse effects on the right ventricle by producing pressure and/or volume overload. Acquired pulmonary valve disease is rare in comparison with other valvular disorders. Rarely, pseudopulmonary valve stenosis can occur as a result of right ventricular outflow obstruction from cardiac tumors or from an aneurysm of the sinus of Valsalva. When the stenosis is severe, patients may occasionally have retrosternal chest pain or syncope with exertion. If the foramen ovale is patent, right-to-left shunting may occur, producing cyanosis and clubbing. A thrill may be felt in the suprasternal notch and at the left upper sternal border. S is often split widely, and the degree of the splitting increases2 with worsening stenosis due to delay in P. The intensity of P may be increased in mild stenosis2 2 but is usually diminished with severe stenosis. An ejection click can sometimes be heard along the left sternal border, and it may vary with respiration. The right ventricular impulse may be palpated at the left sternal border and be hyperdynamic. However, in patients with reduced right ventricular compliance, a prominent a wave may be seen in the venous pulse. Chest radiography may reveal poststenotic dilation of the main pulmonary artery and diminished pulmonary vascular markings. Echocardiography is useful in diagnosing pulmonary valve stenosis and for quantifying the severity of the obstruction. The best images of the pulmonary valve are obtained from the short-axis view at the level of the base from the parasternal and subcostal windows. In adults, the leaflets can appear thickened and calcified with restricted motion. Right ventricular dilation and hypertrophy may be seen in adults, depending on the severity and the duration of this disease. This method of quantifying the degree of stenosis is well correlated with the direct measurement obtained during cardiac catheterization. Moderate stenosis: peak jet velocity of 3 to 4 m/s (peak gradient 36 to 64 mm Hg). The treatment of choice is balloon valvuloplasty, usually leading to a 75% decrement in the transvalvular gradient after a successful procedure. Prognosis and morbidity subsequent to the procedure are largely based on right ventricular function at the time of the procedure. The hypertrophic subpulmonary stenosis that may accompany valvular stenosis usually regresses after successful valvuloplasty. The most common acquired cause is pulmonary artery hypertension, followed by infective endocarditis. However, in the absence of significant pulmonary hypertension, it may be tolerated well for many years.
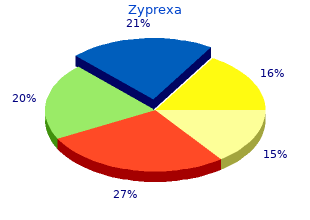
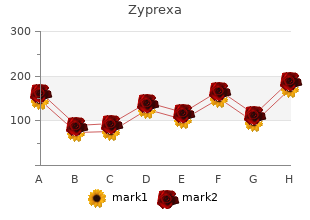
In patients with rheumatic valve disease buy cheap zyprexa online symptoms zinc deficiency, guidelines for the prevention of rheumatic fever should be applied buy zyprexa 7.5 mg with amex symptoms zinc overdose. Annual reevaluation is recommended order zyprexa amex treatment yeast infection men, but a yearly echocardiogram is not indicated unless there is a change in clinical status. Atrial fibrillation can clearly exacerbate symptoms, and cardioversion or rate control measures are important to maintain diastolic filling time. Results of natural history studies, conducted before valvotomy procedures were developed, indicate that young symptomatic patients have about 40% mortality at 10 years and almost 80% at 20 years. The technique involves placement of a balloon-tipped catheter into the left atrium through a transseptal puncture and then across the mitral valve. The hourglass-shaped balloon (Inoue balloon) is inflated and deflated to increasingly larger diameters until the desired result is obtained. The mean valve area usually doubles with a 50% to 60% reduction in transmitral gradient. There are four parts to the assessment (mobility, leaflet thickening, subvalvular thickening, and calcification) (Table 16. In general, extensive subvalvular disease results in a poorer outcome with valvuloplasty. Patients with extensive fluoroscopically visible mitral valve calcification also have a worse outcome after percutaneous therapy. Patients with high scores should not undergo valvuloplasty unless surgical treatment is impossible. No or minimal diastolic movement of valve Subvalvular thickening (grade 0–4, 0 being normal) 1. Extensive thickening to papillary muscles Thickening of leaflets (grade 0–4, 0 being normal) 1. Extensive thickening of all leaflet tissues (>8–10 mm) Calcification (grade 0–4, 0 being normal) 1. Percutaneous balloon dilatation of the mitral valve: an analysis of echocardiographic variables related to outcome and the mechanism of dilatation. The pressure half-time method is unreliable until 24 to 48 hours after the procedure. Data from the National Heart, Lung, and Blood Institute registry of all functional classes of patients show an 84% survival rate 4 years after treatment. These variables identify a population with more serious illness that frequently necessitates intervention and should not preclude valvuloplasty. This was performed through a thoracotomy (without cardiopulmonary bypass) and atriotomy with a valve dilator. This procedure is rarely used in the United States since the development of the percutaneous approach and improvements in open-heart surgery. Open mitral valvotomy involves direct visualization of the mitral valve (with cardiopulmonary bypass), debridement of calcium, and splitting of fused commissures and chordae. Studies in ideal patients for balloon valvuloplasty and commissurotomy suggest equal improvement in valve area and symptoms immediately postprocedure and in medium-term follow-up. In patients with a history of atrial fibrillation, warfarin should be restarted 2 to 3 days after the procedure. Clinical follow-up examination should be performed at least once a year and more often if symptoms develop. It has become common practice at many centers for patients to undergo follow-up echocardiography on a once-a-year basis, although no firm guidelines have been developed for this. A new method for quantification of mitral regurgitation based on color flow Doppler imaging of flow convergence proximal to regurgitant orifice. Percutaneous balloon versus surgical closed and open mitral commissurotomy: seven year follow-up results of a randomized trial. Hydraulic formula for calculation of area of stenotic mitral valve, other cardiac values and central circulatory shunts. Left ventricular function after valve repair for chronic mitral regurgitation: predictive value of preoperative assessment of contractile reserve by exercise echocardiography. Three-dimensional echocardiographic reconstruction of the mitral valve, with implications for the diagnosis of mitral valve prolapse. Identification of high-risk and low-risk subgroups of patients with mitral-valve prolapse. Predictors of long-term outcomes in patients with significant myxomatous mitral regurgitation undergoing exercise echocardiography. Percutaneous balloon dilatation of the mitral valve: an analysis of echocardio-graphic variables related to outcome and the mechanism of dilatation. Carcinoid heart disease is encountered in the setting of primary intestinal carcinoid tumors with secondary metastatic spread to the liver. The murmur increases with inspiration, and2 P is accentuated in the presence of pulmonary artery hypertension. The Graham Steell murmur is a high-pitched, blowing decrescendo diastolic murmur starting immediately after P , which is accentuated by inspiration. A right ventricular S and S may be audible in the fourth3 4 intercostal space and will be augmented by inspiration. Depending on the severity and duration of the regurgitant valve, signs and symptoms of right heart failure may also be present on examination. The pulmonary valve is best evaluated initially with echocardiography, using the left ventricle short-axis view from the parasternal and subcostal windows. The right ventricular outflow tract and pulmonary valve should be interrogated for abnormalities such as leaflet hypoplasia, increased cusp number, and abnormal valve motion (i. Color-flow Doppler will reveal a regurgitant jet toward the right ventricle during diastole. Maintenance of the regurgitant velocity during diastole suggests that pulmonary hypertension is the cause of valve incompetence. Furthermore, increasing pulmonary artery pressures correlate with decreasing acceleration times of pulmonary artery flow. Pulmonary artery pressures can be obtained using Doppler flow measurements and the following equation. The prognosis is very good; rarely is correction of the defect necessary, except in cases of intractable right heart failure. The prognosis due to endocarditis, carcinoid, or pulmonary artery hypertension is dependent on the prognosis and treatment of the primary disease. When a treatment is absolutely necessary, the preferred approach is valve replacement with a bioprosthesis or a pulmonary allograft. Percutaneous deployment of a prosthetic valve has been successfully accomplished in this setting and is another option in addition to surgery.
Excretion: In chronic nephritis safe zyprexa 10mg medications not to take with grapefruit, hypocalcemia occurs because the kidney cannot excrete phosphates order 2.5 mg zyprexa treatment 3rd metatarsal stress fracture. More phosphates are excreted in the stool 5mg zyprexa visa treatment gastritis, blocking calcium absorption and lowering serum calcium. In contrast, with renal tubular acidosis, the kidneys do not reabsorb calcium and phosphorus from the glomerular filtrate, causing hypocalcemia. Approach to the Diagnosis Determining the serum phosphate and alkaline phosphatase levels will facilitate differentiating the causes of hypocalcemia. The phosphates and alkaline phosphatase are elevated in chronic nephritis, but only the alkaline phosphatase is elevated in renal tubular acidosis and malabsorption syndrome. Only the phosphorus is elevated in hypoparathyroidism and pseudohypoparathyroidism. Considering the pituitary, one would remember hypopituitarism, and the thyroid hypothyroidism. If none of the above diagnoses seem to fit, the patient may have glycogen storage disease, cirrhosis, or functional hypoglycemia. Diabetics with hypoglycemia may be taking too much insulin, or their doses of oral hypoglycemic agents may be too high. Approach to the Diagnosis The clinical picture may fit one of the endocrine disorders mentioned above. Hospitalization for a 72-hour fast while taking frequent blood sugar tests will help to diagnose an insulinoma. It follows that starvation and anything else that interferes with the intake of potassium (such as vomiting or diarrhea) will cause depletion of body potassium. This mechanism contributes to the depletion of potassium in pyloric obstruction, intestinal obstruction, and diarrhea of many causes. Absorption: The poor absorption of water and salts in malabsorption syndrome leads to hypokalemia. Regulation: The hormone aldosterone activates the kidney to reabsorb large amounts of sodium in exchange for potassium and hydrogen ion. Consequently, when the adrenal cortex secretes large amounts of this hormone, as in primary aldosteronism, there is associated hypokalemia. Hypokalemia is also associated with secondary aldosteronism as occurs in malignant hypertension, renal artery stenosis, and Bartter syndrome. Excretion: In chronic renal failure of many causes, there is damage to the distal tubules of the kidney so that reabsorption of potassium is impaired; therefore, hypokalemia results. Diuretics such as 494 hydrochlorothiazide may inhibit the distal tubular reabsorption of potassium, causing hypokalemia. Hypokalemia develops in renal tubular acidosis because of a renal tubular defect causing more sodium to be absorbed in exchange for potassium, which creates a potassium deficit. Metabolic alkalosis also enhances the secretion of potassium in exchange for sodium to conserve hydrogen ion, causing hypokalemia. Approach to the Diagnosis A history of vomiting, diarrhea, or use of diuretics will be helpful in determining the cause of hypokalemia. However, serial electrolytes, chemistry panel, and a 24-hour urine potassium level will be most useful. Female genital tract: Such congenital anomalies as an imperforate hymen, imperforate vagina, cervical stenosis, double uterus, or the complete absence of any one or more of these organs would obviously cause amenorrhea. Radiation therapy may destroy the endometrium so that it cannot respond to female hormones. Pregnancy is the most common cause of amenorrhea, and it must be considered the cause of sudden onset of amenorrhea in an apparently healthy woman until proven otherwise. Excessive blood levels of endogenous or exogenous estrogen or progesterone will cause amenorrhea. The tubes should immediately suggest an ectopic pregnancy as the cause, although spotting and 495 metrorrhagia are frequent in these cases. M—Malformations of the ovary include Turner syndrome (where the ovaries are reduced to a fibrotic, pea-sized nodule), Stein–Leventhal syndrome, and other congenital cysts. Acquired malformations suggest the atrophy of menopause, which may occur as early as the late 20s. I—Intoxication includes the ovarian dysfunction of exogenous hormones, irradiation, chronic alcoholism, or drug addiction. N—Neoplasms of the ovary frequently cause amenorrhea, especially if they secrete hormones or are bilateral. The arrhenoblastomas, granulosa cell and theca cell tumors, and cystadenocarcinomas must be considered in this category. T—Trauma as a cause of amenorrhea is well known, but this is generally due to diffuse body trauma such as an automobile crash, severe burns, or extensive surgery. Direct trauma to the ovary merely reminds one that oophorectomy can cause amenorrhea. Emotional trauma is probably a more common cause of amenorrhea than any of the above. S—Systemic disease suggests the amenorrhea of leukemia, Hodgkin lymphoma, chronic nephritis, fever, and severe malnutrition. Thyroid: It is well known that hyperthyroidism causes hypomenorrhea or amenorrhea and hypothyroidism causes hypermenorrhea; however, the exact reverse may occur. Adrenal gland: Visualizing this organ should stimulate the recall of amenorrhea in the adrenogenital syndrome of adrenal hyperplasia or carcinomas and in Addison disease. M—Malformations here are Fröhlich syndrome and Chiari– Frommel syndrome, but perhaps more important is the reduced 497 output of pituitary hormone in many states of congenital mental retardation and brain damage. N—Neoplasm suggests the largest group of causes of hypopituitarism, including chromophobe adenomas and basophilic adenomas. T—Trauma recalls the hypopituitarism of postpartum hemorrhage and amniotic fluid emboli or Sheehan syndrome. One must keep an ectopic pregnancy in mind even if the examination is normal and plan follow-up examinations and ultrasonography should the situation warrant. The gynecologist may give a test dose of intramuscular progesterone to prove that the endometrium functions well. Case Presentation #52 A 34-year-old white mother of three complained of amenorrhea and weight loss. She has been under a lot of emotional distress for several months and has lost her appetite. Utilizing your knowledge of anatomy and physiology, what is your differential diagnosis? Further history reveals that she had a postpartum hemorrhage following her last delivery, and the amenorrhea began at that time. Review of systems reveals that she had loss of axillary and pubic hair and insignificant lactation following her last delivery. Consequently, pyloric obstruction, cholera, viral gastroenteritis, intestinal obstruction, acute ulcerative colitis, and bacterial dysentery lead to hyponatremia.
Discount 7.5mg zyprexa with amex. How Do I Know If I Need a Hip Replacement?.