
Wesleyan University. U. Curtis, MD: "Buy Trimox online in USA - Best Trimox no RX".
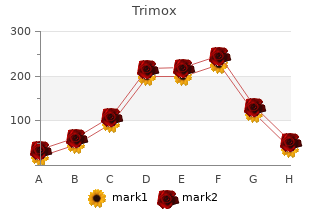
Epinephrine is generally administered first cheap trimox 500 mg without prescription bacterial bloom, and atropine or bicarbonate buy discount trimox online bacteria article, or both order generic trimox antibiotic resistance arises due to quizlet, may be administered subsequently. An attempt to pace the heart with an external device or an intracardiac pacing catheter is advisable although not usually successful, except for certain reversible bradyarrhythmias. With the development of more effective external pacing systems, the role of pacing and its influence on outcome must now be reevaluated. Unfortunately, all data to date have suggested that asystolic patients continue to have a very poor prognosis despite new techniques. These general guides are not to be interpreted as inclusive of all possible approaches or contingencies. Catecholamines are used for cardiac arrest not only in an attempt to achieve better electrical stability (e. Epinephrine is the first choice among the catecholamines for use in cardiac arrest because it increases myocardial contractility, elevates perfusion pressure, may convert electromechanical dissociation to electromechanical coupling, and improves the chances for successful defibrillation. Because of its adverse effects on renal and mesenteric flow, norepinephrine is a less desirable agent despite its inotropic effects. When the chronotropic effect of epinephrine is undesirable, dopamine or dobutamine is preferable to norepinephrine for inotropic effect. Isoproterenol may be used for the treatment of primary or postdefibrillation bradycardia when heart rate control is the primary goal of therapy intended to improve cardiac output. Stimulation of alpha adrenoceptors may be important during definitive resuscitative efforts. For example, the alpha adrenoceptor–stimulating effects of epinephrine and higher dosages of dopamine, which elevate aortic diastolic pressure by peripheral vasoconstriction with increased cerebral and myocardial flow, have been reemphasized. Post–Cardiac Arrest Care and Post–Cardiac Arrest Syndrome After return of spontaneous or stable assisted circulation, focus shifts to the diagnostic and therapeutic 161 elements of post–cardiac arrest syndrome, a field of pathophysiology and clinical intervention that emerged from the recognition that the various elements of injury following cardiac arrest should be organized into a multidisciplinary continuum. The four elements of post–cardiac arrest syndrome include brain injury, myocardial dysfunction, systemic ischemia and reperfusion responses, and control of persistent precipitating factors. The specialized and multidisciplinary nature of post–cardiac arrest care have led to the proposal and preliminary data supporting the concept of 162 specialized cardiac centers for post–cardiac arrest patients, analogous to trauma or stroke centers. The profile of the patient ready for transport is matched to the capabilities of the institution to which the victim is transported (Fig. The Copenhagen model provides a foundation for this additional level of coordination. Patients can be transported to the closest facility appropriate to the optimal or minimal care requirements. Color-coded symbols link level of patient urgency to recommended hospital resources on community grid maps. Some elements of post–cardiac arrest syndrome are common to all resuscitated patients, but the prognosis and certain details of management are specific for the clinical setting in which the cardiac arrest occurred. If ventricular arrhythmias persist after successful resuscitation, a lidocaine infusion is used. Persistent symptomatic bradyarrhythmias requiring permanent pacemakers rarely occur in such patients. Resuscitative efforts usually fail in such patients, and when successful, post–cardiac arrest management is often difficult. All patients in circulatory failure at the onset of arrest are in a high-risk category, with only a 2% survival rate in hypotensive patients noted in one study. In the former category, the ratio of tachyarrhythmic to bradyarrhythmic cardiac arrest is low, and the prognosis for survival of cardiac arrest is poor. Although the data may be somewhat skewed by the practice of assigning “do-not-resuscitate” orders to patients with end-stage disease, the data available for attempted resuscitations show a poor outcome. For the few successfully resuscitated patients in these categories, postarrest management is dictated by the underlying precipitating factors. Most antiarrhythmic drugs (see Chapter 36), a number of drugs used for noncardiac purposes, and electrolyte disturbances can precipitate potentially lethal arrhythmias and cardiac arrest. Beyond these, a broad array of pharmacologic and pathophysiologic- metabolic causes have been reported. Hypokalemia, hypomagnesemia, and perhaps hypocalcemia are the electrolyte disturbances most closely associated with cardiac arrest. Acidosis and hypoxia can potentiate the vulnerability associated with electrolyte disturbances. The in-hospital risk for recurrent cardiac arrest is relatively low, and arrhythmias account for only 10% of in-hospital deaths after successful out-of-hospital resuscitation. The routine use of temporary pacemakers has been evaluated in such patients but has not been found to be helpful for prevention of early recurrent cardiac arrest. Invasive techniques for hemodynamic monitoring are used in patients whose condition is unstable but are not used routinely in those whose condition is stable on admission. Anoxic encephalopathy is a strong predictor of in-hospital death or death within 6 months after discharge. The induction of therapeutic hypothermia to reduce metabolic demands and cerebral 126,127 edema should be applied promptly to a postarrest survivor who remains unconscious on hospital admission, providing a measurable survival benefit. General Care The general management of survivors of cardiac arrest is determined by the specific cause and the underlying pathophysiologic process. The indications for revascularization after cardiac arrest are limited to those who have a generally accepted indication for angioplasty or surgery, including a documented ischemic mechanism of the cardiac arrest. Moreover, in an uncontrolled observation comparing cardiac arrest survivors who had ever received beta blockers after the index event with those who had not, a significant improvement in long-term outcome with beta-blocker therapy was noted. Indications for implantable cardioverter-defibrillators based on evidence and judgment. Guideline classifications and levels of evidence are derived from an amalgamation of narrative and tabular statements in two 165,166 recent guidelines documents, with variations in the documents adjudicated by the authors. Indications for implantable cardioverter-defibrillators based on evidence and judgment. Four antiarrhythmic strategies, which are not mutually exclusive, can be considered for patients at high risk for cardiac arrest: implantable defibrillators, antiarrhythmic drugs, catheter ablation, and antiarrhythmic surgery. The mainstay of therapy for the highest-risk patients is the implantable defibrillator. The choice of a therapy, or combinations of therapies, is based on estimation of risk determined by evaluation of the individual patient by various risk-profiling techniques, coupled with available efficacy and safety data. Methods to Estimate Risk for Sudden Cardiac Death General Medical and Cardiovascular Risk Markers The presence and severity of acquired medical disorders (e. The model demonstrated large, nonlinear gradients of risk, with the major impact in the highest one or two deciles. This magnitude of risk is not sufficient to justify certain interventions, and further risk stratification is needed to identify even higher-risk subgroups at sufficient risk to merit advanced therapies. The potential importance of proper timing and combining of risk markers has been explored. Ambulatory Monitoring Ambulatory monitoring remains useful for profiling the risk for development of life-threatening sustained arrhythmias in individuals with certain forms of structural or electrophysiologic disease who are considered to be at high risk (see Chapter 35). Technological advances facilitate very-long-term monitoring and allow identification of episodic arrhythmias as causes of relevant symptoms, such as near- syncope and syncope.
A skin incision is made below the medial canthal tendon that is extended to the lacrimal fossa with blunt dissection buy trimox in united states online bacteria size. A Crawford lacrimal probe attached to silicone tubing is inserted into the superior punctum and advanced into the lacrimal sac safe trimox 250 mg antibiotics for uti with birth control, which is then opened along its medial wall purchase generic trimox pills infection humanitys last gasp. Following incision of the nasal mucosa through the osteotomy, the posterior flap of the lacrimal sac is sutured to the posterior nasal mucosa flap. The probe is advanced through the osteotomy and into the middle meatus, where it is retrieved through the nare. The second end of the probe is advanced along the same path but beginning through the inferior punctum. The ends of the silicone tubing are tied together in the nare and the anterior flaps of lacrimal sac and nasal mucosa are sutured together. Thrombin and gel foam can be used to control mucosal bleeding, and the skin is reapproximated after ensuring hemostasis. Variant procedures or approaches: If the lacrimal obstruction is more proximal to the lacrimal sac, a Jones tube can be placed (Fig. An endonasal approach using a rigid endoscopic ± laser offers the advantage of no skin incision, good visualization of intranasal pathology and less postop discomfort. The endoscopic approach is more common in children and young adults where the absence of skin creases makes scar concealment difficult. If possible, the surrounding ocular adnexa, including the conjunctiva, Tenon’s connective tissue, and extraocular muscles, are left in place to secure an orbital implant. The procedure begins with a 3608 conjunctival incision (peritomy) at the limbus, allowing exposure of the underlying extraocular muscles and sclera. Each of the recti muscles is isolated with a muscle hook and secured with fixation sutures before disinsertion from the globe. A curved clamp is closed across the optic nerve ~3–10 mm posterior to the globe, and the nerve is cut and the globe removed. After hemostasis has been ensured, an orbital implant (polymethylmethacrylate or hydroxyapatite) is placed into the socket. The overlying muscles, connective tissue, and conjunctiva are closed to improve motility and prevent extrusion. The globe is rotated laterally, while a curved clamp is introduced from the medial direction. Either a curved scissors or an enucleation snare may be used to transect the optic nerve. This usually is performed in cases of endophthalmitis, but never if malignancy is suspected. Exenteration is a more extensive procedure for the management of aggressive malignant tumors or infections where all orbital tissue, often including surrounding orbital bone and adjacent sinuses, is removed. If the extent of orbital tumors is unknown, frozen sections from the surgical margins will be used to determine if exenteration is needed. The orbit may be divided into several compartments, and the surgical approach will vary by the location and size of the lesion. In general, an anterior orbitotomy is used for small tumors in the anterior orbit and can be approached from a transconjunctival, transseptal, or transperiosteal incision. By contrast, a lateral orbitotomy allows for removal of larger masses located further posteriorly in the orbit, as well as those lesions involving the lacrimal gland. In this procedure, the skin incision can be placed just under the brow (Stallard-Wright), in the lid crease with lateral extension, or higher in the eyebrow (coronal). The dissection is carried down to the periosteum, which is then incised and reflected. The lateral orbital wall is exposed, and an osteotomy is performed using an oscillating saw, after preplacing suture holes with a power drill. The section of bone is removed with a clamp, and the periorbita is opened, allowing intraorbital dissection. After biopsy or removal of the mass, the periorbita is closed and the bone fragment replaced. Variant procedures or approaches: A medial orbitotomy is often required to access lesions that are located medial to the optic nerve. These patients are generally healthy, aside from the infection, tumor, or trauma underlying their ocular or periocular pathology. Preop evaluation should focus on possible coexisting disease and the systemic manifestations of previous therapeutic interventions (e. Retinal detachments are classified as traction, exudative (not usually treated with surgery), or rhegmatogenous (rupture, tear). In adults, retinal detachments are most frequently associated with diabetes, myopia, trauma, and previous cataract surgery. Rhegmatogenous retinal detachments (more common in adults) start off with a small retinal tear, which allows the vitreous to seep in between the retina and pigment epithelium, forcing retinal separation. Sx range from floaters and flashing lights to showers of black specks and, ultimately, to a dark shadow that impinges on the field of vision. Less commonly, retinal detachments are induced by other forms of vitreoretinal traction, or by trauma involving an open globe. On rare occasion, retinal detachments are due to the formation of a giant retinal tear. Just as rarely, retinal surgery may be done on premature infants in an effort to prevent or repair retinal detachments. The ultimate aim of retinal surgery is the preservation or recovery of vision through the restoration of normal posterior segment anatomy. Scleral buckles are silicone rubber appliances sutured to the sclera to indent the eye wall, thereby relieving vitreous traction and functionally closing retinal tears. This is an external procedure in which the eye may either not be entered at all or entered with a small needle puncture through the sclera for drainage of subretinal fluid, or injection of gas. Cryotherapy or lasers are used frequently to establish chorioretinal adhesions around retinal tears. Cryotherapy is applied to the sclera; a laser is applied with a fiberoptic cable introduced into the vitreous cavity during vitrectomy surgery, often in combination with a wide-field viewing system. It also can be administered with an indirect ophthalmoscope delivery system for those eyes not undergoing vitrectomy. Simple detachments frequently can be repaired by a pneumatic retinopexy, in which retinal tears are treated with cryotherapy and/or laser, and an expanding gas is injected into the vitreous cavity. This technique usually is done in phakic eyes (eyes with intact lens) with tears between the 9 o’clock and 4 o’clock positions. Vitrectomy (removal of vitreous) is commonly performed to reduce traction on the retina (↓ retinal detachment), clear blood and debris, and remove scar tissue.
Sex differences in the cardiovascular consequences of diabetes mellitus: a scientific statement from the American Heart Association generic 250mg trimox with mastercard bacteria jacuzzi. Risk of all-cause mortality and vascular events in women versus men with type 1 diabetes: a systematic review and meta-analysis purchase generic trimox online antibiotics human bite. Lipoprotein particle profiles by nuclear magnetic resonance compared with standard lipids and apolipoproteins in predicting incident cardiovascular disease in women order discount trimox line bacteria 4 in urinalysis. Association of high-density lipoprotein cholesterol with incident cardiovascular events in women, by low-density lipoprotein cholesterol and apolipoprotein B100 levels: a cohort study. Exercise capacity and the risk of death in women: the St James Women Take Heart Project. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. Cause-specific excess deaths associated with underweight, overweight, and obesity. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. Relationship of physical fitness vs body mass index with coronary artery disease and cardiovascular events in women. The effect of including C-reactive protein in cardiovascular risk prediction models for women. C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8-year follow-up of 14 719 initially healthy American women. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Cardiovascular disease in patients with chronic inflammation: mechanisms underlying premature cardiovascular events in rheumatologic conditions. High prevalence of metabolic syndrome in first-degree male relatives of women with polycystic ovary syndrome is related to high rates of obesity. Impaired glucose tolerance, type 2 diabetes and metabolic syndrome in polycystic ovary syndrome: a systematic review and meta-analysis. Pregnancy-induced hypertension and diabetes and the risk of cardiovascular disease, stroke, and diabetes hospitalization in the year following delivery. Preeclampsia and the risk of ischemic stroke among young women: results from the Stroke Prevention in Young Women Study. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. Primary atherothrombotic occlusive vascular events in premenopausal women with history of adverse pregnancy outcome. Early cardiovascular events in women with a history of gestational diabetes mellitus. Clinical predictors for a high risk for the development of diabetes mellitus in the early puerperium in women with recent gestational diabetes mellitus. Why are women more likely than men to develop heart failure with preserved ejection fraction? Preventing and Experiencing Ischemic Heart Disease as a Woman: state of the science: a scientific statement from the American Heart Association. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. Role of noninvasive testing in the clinical evaluation of women with suspected ischemic heart disease: a consensus statement from the American Heart Association. How to improve noninvasive coronary artery disease diagnostics in premenopausal women? National Council on Radiation Protection and Measurements report shows substantial medical exposure increase. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. Impact of ethnicity and gender differences on angiographic coronary artery disease prevalence and in-hospital mortality in the American College of Cardiology-National Cardiovascular Data Registry. Retinal arteriolar narrowing and risk of diabetes mellitus in middle-aged persons. Mechanisms of myocardial infarction in women without angiographically obstructive coronary artery disease. Sex differences in medical care and early death after acute myocardial infarction. Reduction in sex-based mortality difference with implementation of new cardiology guidelines. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. Incidence and prognostic implications of stable angina pectoris among women and men. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries. Sex differences in hospital mortality after coronary artery bypass surgery: evidence for a higher mortality in younger women. Off-pump coronary bypass provides reduced mortality and morbidity and equivalent 10-year survival. Sex differences in mortality after transcatheter aortic valve replacement for severe aortic stenosis. Sex-Specific Differences at Presentation and Outcomes Among Patients Undergoing Transcatheter Aortic Valve Replacement: A Cohort Study. Transcatheter Mitral Valve Repair in Surgical High- Risk Patients: Gender-Specific Acute and Long-Term Outcomes. A call to action: women and peripheral artery disease: a scientific statement from the American Heart Association. Sex Differences in the Incidence of Peripheral Artery Disease in the Chronic Renal Insufficiency Cohort. One-year costs in patients with a history of or at risk for atherothrombosis in the United States. A population-based study of peripheral arterial disease prevalence with special focus on critical limb ischemia and sex differences. Sex differences in calf muscle hemoglobin oxygen saturation in patients with intermittent claudication. Gender differences in interventional management of peripheral vascular disease: evidence from a blood flow laboratory population. An evaluation of gender and racial disparity in the decision to treat surgically arterial disease. Analysis of gender-related differences in lower extremity peripheral arterial disease.