
Coleman College. Y. Finley, MD: "Buy Brahmi online in USA - Effective Brahmi online OTC".
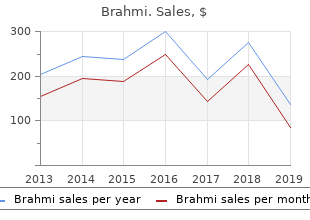
However discount 60caps brahmi with visa symptoms quivering lips, the application of new approaches is complicated by the problem of its high cost order cheap brahmi line treatment nerve damage. To make the analyzes of "willingness-to-pay" in the organization of treatment of patients with depressive disorders in Ukraine brahmi 60 caps discount medications excessive sweating. The object of the research was the survey data of psychiatrists (55 persons) and family members of patients with severe depression (75 people), which was conducted during 2015 in Zaporozhye. The questionnaire worked up for physicians consisted of two parts, in the first part it was necessary to specify personal data (age, place of work, position, work experience in the position, etc. The aim of the second unit was to establish the attitudes of respondents towards the "willingness-to- pay" at the expense from personal funds and rationality of the real cost of treatment with the drug Vortioxytine from the perspective of the health system as a whole. The purpose of questioning of other suffering from depressive disorders patients was to identify the "willingness-to-pay" opportunities by private funds (before that, the respondents indicated the average monthly income per 1 person in the family ), the rationality of the real costs for the treatment with the medicine Vortioxytine from the standpoint of the patient (indicating the cost of its implementation) and determining the maximum "willingness-to-pay" for the expense of personal budget and the rationality of the real costs from the position of health care organization. In the last decade, the results of pharmacoeconomic analysis is widely used in the health care system of the developed countries, while taking such management decisions as registration of medicinal products, development of forms and clinical guidelines (recommendations, standards of conducting patients), to draw up a restrictive list of medical technologies, whicn should to be paid from the expense budget or social insurance. The most valuable for the decision makers, are considered 205 the results of the analysis "cost-effectiveness" and "cost-utility". The analysis of "cost- benefit" remains quite attractive for economists in the field of health care organization because only it gives an indication of economic (monetary) benefit of the technologies contributing to the restoration, preservation or promotion of health. In addition, the results give us an insight into the preferences of the population (potential market) and at the same time can be used for economic justification of the use of medicines. Among others patients the proportion of responses to questions was higher than that among health care workers – to assess "willingness-to-pay" for the personal expense without knowing the cost of treatment with Vortioxytine could 91. After the respondents were informed about the cost of the treatment, to evaluate "willingness-to-pay" could only 79. The study calculated the ratio of the absolute difference of the benefits and costs depending on the size of «willingness-to-pay» for pharmaceutical ensure of different groups of respondents. If we consider the responses of doctors, the use of Vortioxytine is obviously beneficial. But taking into the consideration the opinion of the patients‘ significant additional monetary investment is needed. Evaluation of "willingness-to-pay" which was conducted among physicians showed that 51% of respondents believe that all the expense for the treatment are to be carried out by the health care budget. One of the important issues was to assess the feasibility of the real costs of Vortioxytine. The answer was given after the respondents recognized the real costs to treat depression using Vortioxytine. Among the asked whether it is appropriate to apply Vortioxytine considering its real value and efficiency, responded "no" only around 17. Thus, the results of the study found out that the most "willingness- to-pay " for effective treatment was practitioners than average patients with depressive disorders. Considering the peculiarities of the health care system of Ukraine and the level of current financing, to ensure access of patients with depressive disorders it is necessary to conduct pharmacoeconomic analysis by the method of "risk sharing". Its results will justify a state procurement and establishing the price of the drug depending on the quantity (number of packages) for the treatment of depression, considering the limited financing of the branch. The scheme of partial state financing can also be implement for the expensive treatment involving 3 participants (the government – manufacturer – patient). It is only necessary to determine the percentage of reimbursement of expensive drugs in the case of the introduction of health insurance to ensure access of patients to high-tech means and methods of treatment. Medical insurance - a form of social protection in the interests of public health, resulting in a guaranteed payment of medical care in the event of an insurance case, due to the accumulated byinsurerfunds. The situation prevailing in the Ukraine in the field of public health requires immediate action. According to Article 9 of the Law of Ukraine ―On insurance‖ franchise - a part of the losses which is not compensated by the insurer under the insurance contract. Table 2 Health care facilities category The size of the franchise according to provides by insurance option health care facilities category 1 2 3 4 1, 2, 3, 4 0% 0% 0% 0% 2, 3, 4 20% 0% 0% 0% 3, 4 40% 20% 0% 0% 4 80% 60% 30% 0% For example, if the insured elected to service the medical institutions of the 3rd, 4th category, and assistance was provided in the institution 1 category, the franchise will be 40%. In this case, the insured person has their own reimburse 40%, and the insurer pays 60% of the cost of services. The development of medical science, improvement of living standards and the establishment of democratic institutions contributes to the requirements of health workers and increasing cases of disciplinary measures for improper performance of professional duties. However, health workers can potentially be held accountable for crimes under twelve articles of the Criminal Code of Ukraine, the Code of Ukraine on Administrative Offences and Civil Code of Ukraine. In the public mind, and formed a long time maintained naturally thought of the enormous responsibility of doctors for life and health. However, the reality of the last decade in Ukraine indicate that the urgency of the consideration of legal liability in medicine confirmed by the increasing number of claims with regard to various disorders during treatment. The aim of the study is to clarify aspects of the modern application of legal liability for health workers in Ukraine and abroad. In the modern Australian law there are two models of responsibility - objective and relative. The first is that medical officer responsible for injury victim, if the terms of an objective assessment of the average observer behavior is influenced by the doctor on the natural course of events. Instead, the relative responsibility model is 209 used when there is material damage caused as a result of treatment. The criterion for such damage is the general rules on goods, services, securities, profits and such others. In Ukraine, a long time it was mainly about the criminal methods of influence on offenders in medicine. The adoption of the new Civil Code of Ukraine, development of legislation on health care, the formation of judicial practice in cases of prosecution of health professionals indicates the presence of four fundamentally different types of doctors liable for offenses committed: criminal; civil (property); administration; disciplinary. Today, according to various sociological studies, doctors are more competent in matters of criminal liability, but increase in the prosecution of doctors to other types of liability causes to focus on their education. The key to quality of legislative work directed towards the improvement of legislation on health care, is a qualitative theoretical framework which should be formed as a result of comprehensive research involving lawyers, health care, doctors, practitioners and representatives of other interested parties. Therefore, we should focus on the need to provide effective remedies in domestic science and practice to address issues of accountability for health workers or that the damage caused to the health of the patient. Thus, physicians should clearly understand the responsibility that comes in the case of offenses and patients to be sure that the protection of rights and legitimate interests guaranteed by the state and society in law. The problem of full and timely immunization coverage of children‘s contingent of the population is highly important for Ukraine at the present stage. However, in recent years there has been a significant discrepancy in the existing results to the needed indicator, one of the reasons of which is a lack of reliable information for the population about the effectiveness of vaccination in the prevention of infectious diseases and contradictions of its legal nature, which causes distrust of the population to this measure and the refusal of parents to vaccinate their child. Considering the above, the aim of our study was to investigate the views of pediatricians, who among healthcare workers are the most involved in the process of children‘s vaccination, about legislative and ethical aspects of the children‘s routine vaccination. During the work the method of questionnaire survey, that is widely used in research of organizational and economic nature, was used.
Diseases
Because increased liver enzyme levels may occur in patients receiving long-term lovastatin therapy discount brahmi 60caps visa treatment yeast infection men, liver function test results should be monitored 60 caps brahmi for sale medicine you cant take with grapefruit. A patient diagnosed with hypertension is most likely to be prescribed which class of drugs first? Types of drugs used to treat disorders of the hematologic system include: • hematinic • anticoagulant • thrombolytic buy brahmi uk medicine lake. They do so by increasing hemoglobin, the necessary element for oxygen transportation. Iron, vitamin B12, folic acid This section discusses hematinic drugs used to treat micro- cytic and macrocytic anemia—iron, vitamin B12, and folic acid. Iron preparations discussed in this section include ferrous fumarate, ferrous gluconate, ferrous sul- fate, iron dextran, and sodium ferric gluconate complex. Pharmacokinetics (how drugs circulate) Iron is absorbed primarily from the duodenum and upper jejunum of the intestine. Different iron formulations don’t vary in absorp- tion, but they do vary in the amount of elemental iron supplied. Low iron increases absorption The amount of iron absorbed depends partially on the body’s stores of iron. On the oth- er hand, when total iron stores are large, the body absorbs only about 5% to 10% of the iron available. Enteric-coated preparations decrease iron absorption because, It takes about in that form, iron isn’t released until after it leaves the duodenum. Iron is transported by the blood and bound to transferrin, its carri- er plasma protein. About 30% of the iron is stored primarily as he- mosiderin or ferritin in the reticuloendothelial cells of the liver, spleen, and bone marrow. Excess iron is excreted in urine, stool, sweat, and through intestinal cell-sloughing. Pharmacodynamics (how drugs act) Although iron has other roles, its most important role is the pro- duction of hemoglobin. Pharmacotherapeutics (how drugs are used) Oral iron therapy is the preferred route for preventing or treating iron deficiency anemia. It’s used to prevent anemias in children ages 6 months to 2 years because this is a period of rapid growth and development. Pregnant women may need iron supplements to replace the iron used by the developing fetus. To guard against such a reaction, administer an initial test dose before giving a full-dose in- cause acute hypersensi- fusion. To test for drug with end-stage renal disease who are receiving hemodialysis may sensitivity and prevent also receive parenteral iron therapy at the end of their dialysis ses- serious reactions, al- sion. While parenteral iron therapy corrects the iron store defi- ways give a test dose of ciency quickly, it doesn’t correct the anemia any faster than oral iron dextran before be- preparations would. Iron preparations available for parenteral administration are Carefully assess the iron dextran (given by I. Other drug interactions involving iron include: nephrine and standard • Absorption of tetracyclines (demeclocy- emergency equipment cline, doxycycline, minocycline, oxytetracy- readily available. Pharmacokinetics Vitamin B12 is available in parenteral, oral, and intranasal forms. For the body to absorb oral forms of vitamin B12, the gastric mu- cosa must secrete a substance called intrinsic factor. People who Some patients have a deficiency of intrinsic factor develop a special type of ane- lack a crucial mia known as vitamin B -deficiency pernicious anemia. It then travels via the bloodstream to the liver, where 90% of the body’s supply of vitamin B12 is stored. Although hydroxocobalamin is absorbed more slowly from the injection site, its uptake in the liver may be greater than that of cyanocobalamin. Most gets lost With either drug, the liver slowly releases vitamin B12 as needed by the body. About 3 to 8 mcg of vitamin B12 are excreted in bile each day and then reabsorbed in the ileum. Within 48 hours after a vitamin B12 injection, 50% to 95% of the dose is excreted unchanged in urine. Pharmacodynamics When vitamin B12 is administered, it replaces vitamin B12 that the body would normally absorb from the diet. This vitamin is essen- tial for cell growth and replication and for the maintenance of myelin (nerve coverings) throughout the nervous system. Pharmacotherapeutics Cyanocobalamin and hydroxocobalamin are used to treat perni- cious anemia, a megaloblastic anemia characterized by decreased gastric production of hydrochloric acid and intrinsic factor defi- ciency. Intrinsic factor, a substance normally secreted by the pari- etal cells of the gastric mucosa, is essential for vitamin B12 absorp- tion. Intrinsic factor deficiencies are common in patients who have had total or partial gastrectomies or total ileal resection. Adverse reactions to vitamin B12 therapy No dose-related adverse reactions occur with vitamin B12 therapy. However, some rare reactions may occur when vitamin B12 is adminis- tered parenterally. Parenteral problems Adverse reactions to parenteral administration can include hypersensi- tivity reactions that could result in anaphylaxis and death, pulmonary edema, heart failure, peripheral vascular thrombosis, polycythemia vera, hypokalemia, itching, transient rash, hives, and mild diarrhea. Oral vitamin B12 preparations are used to supplement nutri- tional deficiencies of the vitamin. The parenteral and intranasal formulations are used to treat patients with pernicious anemia. Drug interactions Alcohol, aspirin, neomycin, chloramphenicol, and colchicine may decrease the absorption of oral cyanocobalamin. This type of anemia usually occurs in patients who have tropical or nontropical sprue, although it can also result from poor nutritional intake during pregnancy, infancy, or childhood. Pharmacokinetics Folic acid is absorbed rapidly in the first third of the small intes- tine, distributed into all body tissues, and metabolized in the liver. Excess folate is excreted unchanged in urine, and small amounts of folic acid are excreted in stool. Adverse Pharmacotherapeutics reactions to Folic acid is used to treat folic acid deficiency. Patients who are folic acid pregnant or undergoing treatment for liver disease, hemolytic ane- Adverse reactions to mia, alcohol abuse, or skin or renal disorders typically need folic folic acid include: acid supplementation. Serum folic acid levels below 5 ng/ml indi- • erythema cate folic acid deficiency. Folic drugs usually acid, iron, vitamin B12, replace one of Erythropoietin agents amino acids, copper, these missing and cobalt are all parts. After subQ administration, serum levels of epoetin alfa peak in 5 to 24 hours, while serum levels of darbepoetin alfa peak in 24 to 72 hours. The circulating half-life of epoetin alfa is also shorter at 4 to 13 hours, compared to 49 hours for darbepoetin alfa. The therapeutic effect of these agents lasts for several days after ad- ministration.
Diseases
Overall order 60 caps brahmi with visa medications janumet, prescription drug sales remain strongly concentrated in the United States cheap brahmi 60caps without prescription symptoms 10dpo, Europe purchase cheapest brahmi medicine 031, and Japan. Even with a larger population, Europe’s share of global pharmaceutical consumption was nearly ffteen percent less than that of the United States (see Table 5, below). Clinical trials offer a further indication of where the pharmaceutical industry is orienting its activities. While press attention has focused on the outsourcing of clinical trials to developing countries, as of spring 2008 the vast majority of trials underway were in North America or Europe. Yet with over twice as many clinical trials going on in the United States as in the European Union, frms appear to be running trials in their home countries, creating a virtuous cycle from R&D investment to testing to market approval for frms in the United States. Measured by the patient pool, costs, regulatory conditions, availability of expertise, and infrastructure, Germany’s high costs, modest 279 Arthur Daemmrich patient populations, and challenges of recruiting participation in clinical research put it below the Czech Republic, the United Kingdom, Poland, and Hungary. In February of 006, the Bundestag passed legislation lowering the “reference price” – the amount that insurers must cover – to the bottom third of existing prices. Patients are responsible for making up the difference for drugs priced above the limit. As a commentary in Nature Biotechnology noted, however, “In theory, innovative drugs should be excluded from the mechanism, but in the past, more and more patent-protected drugs were included as they were dubbed ‘pseudo-innovative’ by the system’s oversight bodies. Quoting an expert from the trade magazine 15 Wynn Bailey, Carol Cruickshank and Nikhil Sharma, “Clinical Trial Offshoring: Country Attractiveness Index”. Ketcham, “Reference Pricing of Pharmaceuticals for Medicare: Evidence from Germany, the Netherlands, and New Zealand,” in David M. Richard Wang, “The Quantity and Quality of Worldwide New Drug Introductions, 198 - 00 ,” Health Affairs 25 (2006), 452-460. There are 80 million ‘consumers’ here, and the older they get, the more medicine they’re going to need. American patients are thus benefting with “access to cutting-edge medicines before they are available in Europe. The Bain report further argued that European countries will suffer delayed access to drugs and poorer health outcomes. Quantifying results, Bain estimates that Germany lost nearly $5 billion in health value from lowered access to innovative drugs and thousands of “high value added” jobs that were created instead in the United States. Firms may be motivated to open sales branches in countries with higher margins, but this does not explain the relative decline of the German and French pharmaceutical industry. While measures of the top ffteen frms may be skewed because German frms did not merge to global scale in the same way as companies in the United Kingdom (GlaxoSmithKline), France (Sanof-Aventis) or Switzerland (Novartis), smaller frms in the United States (Eli Lilly) and Japan (Takeda) also did not undertake signifcant mergers to achieve growth. Instead, as the rest of this chapter argues, differences in regulatory cultures – notably, responses to a new disease, boundaries to compassionate use, and attention to biomarkers and other aspects of consumer-oriented drug development – provides an important explanatory dimension missing from other analyses the pharmaceutical sector. Results presented here focus on the United States and Germany; further work is needed to develop 20 Martin Schrader, “The Decline of German Pharma Companies,” Deutsche Welle (21 April 2005). The comparison reveals that pharmaceutical frms in Germany operate in a distinctive innovation and regulatory culture characterized by tensions regarding authority and evidence among physicians, industry, and government offcials. The German system operated in a collaborative mode that fostered its domestic pharmaceutical industry before the 1980s. Since that time, the predictability of centralized regulation based on a tight regime of quantifed clinical trials in the United States coupled to the emergence of a focus by the regulatory system on consumers and their rights to access ultimately benefted frms operating in that country over their German counterparts. Consumer-Oriented Pharmaceutical Regulation Although there were some 19th century precedents, government mandates for proof of safety and effcacy primarily were established over the course of the 0th century, especially in the wake of the thalidomide tragedy of the early 1960s. In effect, a new form of surveillance and regulation emerged based on disease-based interest groups that not only pressure legislative bodies for additional research funding, but also closely monitor both government agencies and industry. Employing the internet and other communication technologies to build their membership and communal identity, these consumerist and activist groups have signifcantly impacted the regulatory terrain. Policy debates in Europe followed a different direction, with greater attention to prices, equality of access, and protection from dangerous compounds. A shift to new regulatory approaches did not take place to the same degree, likely due to a combination of fewer resources among potential activists and health systems that provided not just drugs, but more comprehensive care. The disease eventually provoked a crisis in American drug regulation, pitting disease activists against an agency supposedly acting in their interests. Under these provisions, companies could distribute unapproved medicines to patients with life- threatening diseases, so long as there was a “reasonable basis” for concluding that the drug was effective and would not expose patients in clinical trials to “signifcant additional risks. In particular, patient groups denounced screening methods, requirements for placebo use, and restrictions on trial participants. Rheinstein, “Access to Investigational Drugs for Treatment Purposes,” American Family Physician (15 September 1994): 845-847. Delaney, “The Case for Patient Access to Experimental Therapy” Journal of Infectious Diseases. As a result, companies could more easily recruit patients and potential new drugs moved from the laboratory to the clinic more rapidly than in the past. They also provided direct assistance for patients in advanced stages of the disease. Patients and activists generally agreed with government offcials that the 1976 Drug Law already accounted for contingencies associated with the emergence of a new and deadly disease. Access to test results, however, remained limited to the drug company, physicians conducting clinical trials, and government offcials. Since well-controlled boundaries distinguished between experts and patients, drug testing did not become a site for debates about representation or access to medicines. Compassionate Use and Underserved Patients In recent years, the compassionate use of pharmaceuticals still in various stages of pre-market testing has engaged patient groups, industry, and government agencies in ways that further illustrate the differences in regulatory approaches followed by the United States and Europe. Patients with terminal diseases have long occupied a special status and despite stronger regulatory controls implemented over the course of the 20th century, physicians have retained the right to prescribe medicines for off-label uses. Nevertheless, many cancer patients continue to fall outside the health status defned by sponsor companies for their experimental drugs. For companies required by law to report and investigate any adverse reactions or fatalities that occur when a patient is on their medicine, compassionate use programs pose a challenge. But frms are understandably nervous that if a patient dies while taking a still-experimental therapy, it can be diffcult to differentiate the natural course of disease from an adverse reaction to the treatment. Citing several tragic cases of terminally ill patients who failed to qualify for clinical trials of new anti-cancer agents due to their advanced disease, an organization called the Abigail Alliance (begun by Frank Burroughs and named for his deceased daughter) fled a lawsuit heard in D. Specifcally, the Alliance sought to make available any drug that had cleared phase I trials (which collect data about a chemical’s pharmacological properties in small numbers of healthy subjects; they generally do not determine dosage or effcacy in patients with the disease). In the United States it is now widely held that the production of information about drugs requires large, double-blinded, placebo- controlled studies. In this framework, the individual is served best by statistical analysis of large populations. Medical authorities and the industry worried that access to medicines outside of clinical trials would undermine incentives for patients to volunteer as subjects. As a consequence, the issue does not feature as prominently in legal circles or media coverage of pharmaceutical regulation.