
Bethany College, Scotts Valley, CA. U. Zakosh, MD: "Buy Aciphex online no RX - Effective Aciphex online no RX".
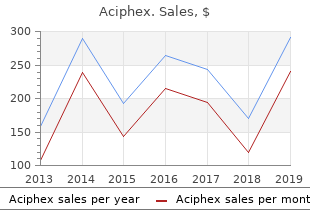
Continuous pharmacological prophylaxis is also conditions 20 mg aciphex with mastercard gastritis diet êóðñ, cost and reimbursability buy aciphex mastercard gastritis x helicobacter pylori. Patient-related factors to be not indicated in most children with febrile seizures who are older considered include seizure type and syndromic diagnosis trusted aciphex 10 mg gastritis symptoms vomiting, age, than 1 year (the treatment of febrile seizures is considered further gender, comorbidities, comedications, risk factors for potential in Chapter 14) [42]. Phenobarbital may also be started at a ‘thera- used) peutic’ dosage, but because of its long half-life the time-course of Easy management (effcacy and safety of individual drugs can be pharmacological action is infuenced by the slow accumulation of evaluated separately) the drug in plasma, a process that may require several weeks. Children, elderly individuals and individuals with certain comorbidities or comedications may require doses and titration rates diferent from those given in Table 9. The rate of dose escalation is also partly dependent on the treatment setting: a pa- as personal attitudes in relation to possible recurrence or seizures tient with frequent seizures, for example, may require more rapid or appearance of specifc adverse drug efects. Initial target maintenance dosage The initial target maintenance dosage can be defned as the dosage Dose escalation at which the patient is stabilized at the end of the initial dose esca- When an immediate therapeutic efect is required, as in the man- lation phase [45]. In general, this corresponds to the lowest daily agement of status epilepticus or frequently recurring seizures, treat- dosage that is expected to produce seizure control in that individual. In most situations, how- This approach is justifed by the desire to minimize the probability ever, this aggressive approach is neither necessary nor desirable, of exposing individuals to long-term treatment with dosages higher and treatment should be initiated with a small dose and increased than necessary. Gradual dose escalation has In recent years, evidence has accumulated that most individuals several advantages. In a slowly afer initiation of treatment [46], and immediate use of a large single-centre study that explored the efectiveness of the frst full maintenance dosage may cause major tolerability problems. In a recent randomized trial that com- topiramate, tiagabine, zonisamide and perampanel. Primidone pared carbamazepine and levetiracetam in adults with newly di- may cause a particularly marked transient intolerance reaction in agnosed focal epilepsy, about 90% of seizure-free individuals were individuals not previously exposed to barbiturates, and it should controlled at doses of 400 mg/day for carbamazepine and 1000 mg/ be started at a dose (62. An indication of possible initial target maintenance dosages • Despite common belief, allergic and idiosyncratic reactions are is provided in Table 9. In practice, the target dosage should be ofen dependent on starting dose and rate of dose escalation [47]. Many genetic (syn: idiopathic) general- ated at too-high doses are especially frequent with carbamaze- ized epilepsies respond well to treatment, and it may be justifed in pine, phenytoin and lamotrigine. Because valproic acid increases these individuals to aim at initial maintenance dosages and plasma the plasma levels of lamotrigine, the risk of lamotrigine-induced drug levels in the low range. For example, the dosage of valproic allergic reactions is greatly increased in individuals comedicat- acid required to control primary generalized tonic–clonic seizures ed with valproic acid, and in these individuals it is essential that has been found to be about 30% lower than that required to control lamotrigine dosage is escalated at a very slow rate. A high seizure frequency before starting ther- • Some individuals can be optimally controlled at doses below the apy, symptomatic epilepsy, focal seizures, multiple seizure types, initial target maintenance dosage. When seizure frequency is suf- associated neurological handicaps and an unfavourable response to fciently high to permit a meaningful assessment of therapeutic previous antiepileptic drug therapy all infuence the prognosis neg- response over a short period, slow dose escalation may allow atively [51,52], and individuals with these features are expected to identifcation of the lowest dose regimen at which individuals require comparatively higher doses and plasma drug levels. Conversely, some individuals are unusually sensitive to factors afecting choice of the initial maintenance dosage include adverse efects, and slow dose escalation will prevent them from the presence of physiological or pathological conditions leading being exposed to dosages higher than those tolerated. Elderly individuals, in par- tration rates are seldom established in regulatory clinical trials and ticular, generally require dosages in the low range, because they therefore they are mostly identifed through postmarketing experi- exhibit an increased sensitivity to the efects of antiepileptic drugs ence. Usual initial target Usual maintenance maintenance Frequency of Drug dosage (mg/day) dosage (mg/day) administration Suggested titration rate Carbamazepine 400–600a 400–1600 2–3 times/day (twice Start with 100 or 200 mg/day and increase to target daily with controlled- dosage over 1–4 weeks release formulations) Clobazam 10–20 10–40 Once or twice daily Start with 10 mg/day. If indicated, increase to 20 mg/ day after 1–2 weeks Eslicarbazepine 800 800–1200 Once daily Start with 400 mg/day and increase to target dosage acetate after 1 or 2 weeks Ethosuximide 500–750 500–1500 2–3 times/day Start with 250 mg/day and increase to target dosage over 1–3 weeks Felbamate 1800–2400 1800–3600 3 or 4 times/day Start with 600–1200 mg/day and increase to target dosage over 10–21 days Gabapentin 900–1800 900–3600 2 or 3 times/day Start with 300–900 mg/day and increase to target dosage over 5–10 days Lacosamide 200–300 200–400 Twice daily Start with 100 mg/day and increase to target dosage by increments of 100 mg/day every week Lamotrigine 50–150 50–200 Twice daily (once Monotherapy: start with 25 mg/day for 2 weeks, then (monotherapy); (monotherapy or daily possible with increase to 50 mg/day for 2 weeks. Further increases 50–100 (patients on patients on valproic monotherapy by 50 mg/day every 2 weeks valproic acid); acid); 200–500 and valproic acid Valproic acid comedication: start with 25 mg on 200–300 (patients (patients on comedication) alternate days for 2 weeks, then 25 mg/day for 2 weeks. Further increases by 50–100 mg/day every 2 weeks Levetiracetam 1000–2000 1000–3000 Twice daily Start with 500 or 1000 mg/day and increase, if indicated, after 2 weeks Oxcarbazepine 600–900 600–3000 2 or 3 times/day Start with 300 mg/day and increase to target dosage over 1–3 weeks Perampanel 4–8 4–12 Once daily Start with 2 mg and increase to target dosage at 2-week intervals (weekly intervals may be used for patients taking comedications that shorten the half-life of perampanel) Phenobarbital 50–100 50–200 Once daily Start with 30–50 mg at bedtime and increase, if indicated, after 10–15 days Phenytoin 200–300 200–400 Once or twice/day Start with 100 mg/day and increase to target dosage over 3–7 days Pregabalin 150–300 150–600 2 or 3 times/day Start with 75 mg/day for 3 days, then increase to 150 mg/day. If indicated, increase to 300 mg/day after 2 weeks Primidone 500–750 500–1500 2 or 3 times/day Start with 62. In patients on enzyme-inducing comedication a faster titration may be used Retigabine 600 600–1200 3 times/day Start with 50–150 mg/day and increase to target dosage at about weekly intervals Rufnamide 1200 1200–3200 Twice daily Start with 400 mg/day and increase by 400 mg/day increments every 2–4 days (Continued) 116 Chapter 9 Table 9. This information refects the author’s assessment of available evidence and may differ from information reported in data sheets in individual countries. Some patients will require dosages, titration rates and dosing regimens different from those given in this table. The individual’s attitude and circumstances should also be con- with valproic acid, which prolongs the half-life of lamotrigine (see sidered. Some neurologists have agabine, more than two daily administrations may be required to also in the past favoured the use of relatively high initial mainte- minimize excessive fuctuations in plasma concentration. This is nance dosages out of a fear that a delay in achieving complete sei- especially important for individuals in whom half-lives are at the zure control might increase the probability of the epilepsy becom- shorter end of the spectrum, such as children and enzyme-induced ing intractable. With these drugs, intermittent adverse efects are for most of the epilepsy syndromes, there is no evidence that this not uncommon at the time of peak drug concentration, whereas is the case. More than twice-daily dosing may similarly be Frequency of administration required for gabapentin, which also has a short half-life and, ad- For most antiepileptic drugs, attainment of an adequate response is ditionally, is absorbed from the intestine by a saturable transport dependent on the persistence of efcacious drug concentrations at mechanism (see Chapter 36). Because the concentration at the site high dosages, utilizing multiple daily administrations of gabapen- of action is in equilibrium with the concentration in plasma, a dos- tin provides a strategy to improve the oral absorption of the drug. Tese are discussed briefy in the next rate of absorption of the drug and its elimination half-life (see Chap- section of this chapter. With rapidly absorbed compounds, it is a good general rule In some individuals, even drugs with short half-lives such as gab- to choose a dosing interval that is no greater than the half-life of the apentin and tiagabine may still produce adequate responses with drug. Drugs with a slow elimination rate such as phenobarbital may a twice-daily schedule. This may be explained, at least in part, by be given once daily at bedtime, but most other antiepileptic drugs pharmacodynamic variability (i. The optimal frequency of may tolerate well high peak plasma drug levels or, conversely, main- administration may also vary depending on pharmacokinetic pat- tain a good response at low trough concentrations). For example, lamotrigine should be there is also evidence that a dissociation exists between their con- given twice daily in individuals taking concomitant enzyme-induc- centration profle in plasma and the duration of efect. For example, ing antiepileptic drugs (due to its relatively short half-life in these levetiracetam is recommended for use on a twice-daily schedule individuals), but it may be given once daily in adults receiving no despite a plasma half-life of about 7 h. In the case of vigabatrin, comedication, and, even more appropriately, in those comedicated which also has a plasma half-life of about 7 h, even once-daily General Principles of Medical Management 117 dosing might be appropriate because its action involves irrevers- viduals. Tere is some In recent years, a number of reports have highlighted the possibili- evidence that valproic acid also has a longer duration of action than ty of adverse clinical outcomes following generic substitution [66], expected from its half-life [61], and once-daily dosing of valproate although this is not confrmed in all studies [67], and evidence is feasible in many individuals, particularly when a sustained-re- from long-term well-designed randomized controlled trials on this lease formulation is used. In view of these considerations, there is gen- recommended in women of child-bearing potential, because ani- eral agreement that any switch between pharmaceutical products mal studies suggest that teratogenic efects may be enhanced at high of antiepileptic drugs should be approved by the physician, that peak plasma concentrations of the drug [62]. Greater concerns apply to countries in For individuals stabilized on chronic treatment, tablets or capsules which regulatory control of the quality of pharmaceuticals is less should be preferred to syrups, whenever possible, because they strict, particularly low-income countries [68]. Monitoring plasma allow more precise dosing, avoid the efect of tooth-damaging in- concentrations can be useful for rapid detection of potential chang- gredients such as sucrose, and minimize the risk of adverse efects es in plasma drug concentration when switching formulations. Nearly all children Sometimes it is desirable to modify a drug’s rate and extent of above the age of 5 years can cope with conventional solid dosage absorption in order to obtain a more favourable plasma concentra- forms.
Diseases
The mean lamotrigine half-lives determined were ing autopsies [54] order 20 mg aciphex mastercard gastritis diet óêðíåò, showed good penetration into the brain order aciphex on line gastritis diet âê. Elimination Lamotrigine is metabolized by the liver buy aciphex 10 mg low cost gastritis diet óêðàèíà, predominantly via N-glu- Hepatic dysfunction curonidation, which is the rate-limiting step in lamotrigine elimi- The clearance of lamotrigine is reduced by about 25% in patients nation [45]. Approximately 70% of a single oral dose is recovered with mild hepatic dysfunction. A more prominent reduction in in the urine during the frst 6 days and about 2% of an oral dose is lamotrigine clearance is observed in patients with moderate and excreted in the faeces. Clearance is increased by 20– syndrome, the clearance of lamotrigine clearance is moderately 170% in children, but not for the frst week of life. In comparative reduced and the lamotrigine half-life is prolonged by about 35% studies of lamotrigine monotherapy, apparent oral clearance and compared with values found in healthy subjects [58]. In the study in children, weight-normalized clearance a clear understanding of possible interactions between lamotrigine appeared to be higher in children younger than 6 years (0. The pharmacokinetics of lamotrigine afer multiple dose admin- istration conforms to that predicted from single-dose studies [45], Effects of co-administered drugs on lamotrigine indicating that clinically signifcant autoinduction does not occur pharmacokinetics [57]. Diminished glucuronidation of lamotrigine accounts for an Other antiepileptic drugs age-related decline in the clearance of the drug in the elderly [55]. Co-administration of valproic acid, an inhibitor of lamotrigine A comparison of the pharmacokinetics of lamotrigine (150 mg oral glucuronidation, has been shown to markedly reduce lamotrig- dose) in healthy young (26–38 years) and elderly (65–76 years) vol- ine clearance and to prolong markedly lamotrigine half-life [25]. Tese changes reverse rapidly within the frst pronounced peak–trough fuctuations in serum lamotrigine con- few days post partum. The changes in lamotrigine pharmacokinet- centrations at steady state, particularly in children under 6 years of ics during pregnancy seem to be much less signifcant in women age [47]. Synergistic therapeutic efects, as well as some adverse efects (par- Dosing guidelines have been developed to optimize dose titra- ticularly development of tremor), have been observed when com- tion and target dosages in relation to age and type of co-medication. Diplopia, dizziness, nausea, ataxia and nystagmus – classic signs While some reports have suggested that lamotrigine clearance may of carbamazepine toxicity – were reported in some adult and pae- be accelerated by oxcarbazepine, a carefully conducted study in diatric patients when lamotrigine was added to carbamazepine healthy volunteers found no evidence of a pharmacokinetic inter- therapy [83,84,85]. However, the efects of lamotrigine Oral contraceptives and hormone replacement therapy on the serum concentration of carbamazepine-10,11-epoxide are Addition of combined oral contraceptive decreases lamotrigine lev- ambiguous. In adults, the addition of lamotrigine to existing car- els by around 50% on average [77]. The interaction, which is caused bamazepine therapy has variously been reported to increase serum by stimulation of lamotrigine metabolism by the oestrogen com- carbamazepine-10,11-epoxide concentrations by 10–45% [84] or ponent of the contraceptive, may result in loss of seizure control if to leave them unaltered [85,86]. In children, the mean serum con- lamotrigine dosage is not appropriately adjusted. This interaction centration of carbamazepine-10,11-epoxide decreased signifcant- shows a biphasic time course, with a prominent decrease in serum ly when lamotrigine was added to carbamazepine therapy in one lamotrigine concentration during the period of pill intake, and study [87]. A pharmacodynamic interaction resulting in reciprocal gradual return toward baseline levels during the 7-day pill-free in- facilitation of adverse efects has also been reported between lamo- terval. A decrease in serum lamotrigine concentration is also seen A clear relationship between serum lamotrigine concentrations with hormone replacement therapy in postmenopausal women and clinical response has not been established in clinical trials [86]. Cessation of intake of oestrogen-containing medications can A target range of between 1 and 4 µg/mL was initially suggested result in a marked rise in serum lamotrigine levels, with the atten- [80,88,89] but children and adults with refractory epilepsy fre- dant risk of manifestations of toxicity. Interestingly, concomitant quently require higher serum concentrations to gain optimum sei- intake of valproic acid seems to antagonize the stimulating efects zure control [80]. Although dose-related improvements in seizure of combined steroid contraceptives on lamotrigine metabolism, control have been observed in children over the serum concentra- and in women co-medicated with valproic acid, serum lamotrigine tion range of 4–21 µg/mL [80], most investigators have not found levels appear to be comparable in the presence and in the absence of this [44,75,80]. Likewise, there is a variable relationship between serum con- Other drugs centration and incidence of adverse efects [44,80,93,94], although Olanzapine can cause a modest (about 25%) reduction in serum some studies suggest that a useful correlation does exist. Rifampicin also reduces serum lamotrigine con- atric study of high-dose lamotrigine therapy, increases in lamotrig- centrations. With respect to interactions with antiretroviral drugs, ine serum concentrations above 21 µg/mL were prevented because serum lamotrigine concentrations are reduced by about 50% by of the development of unacceptable levels of nausea that did not lopinavir/ritonavir, and by about 30% by atanazavir/ritonavir [79]. In a ret- Conversely, atanazir alone and raltegravir do not afect lamotrigine rospective study of 811 patients, reviewing 3731 lamotrigine serum exposure. The correlation between serum lamotrigine levels and tolera- to a clinically important extent (for review see [[39,49,80]. Lamotrigine 503 Effcacy 50% reduction in focal seizures compared with baseline was seen in The frst randomized trials of the antiepileptic efcacy of lamotrigi- 42% in the lamotrigine group and 16% in the placebo group [80]. A greater than 50% A large number of short-term, randomized, double-blind, seizure reduction was seen in 42% of lamotrigine-treated patients placebo-controlled studies, many with a cross-over design, have compared with 24% for the placebo group. Because of the uncontrolled nature of the study, these re- py, reducing total seizure frequency by 36%, with a responder rate sults should be interpreted with caution. A pooled analysis of pivotal trial data focusing on seizure free- Efcacy has also been demonstrated against focal seizures in dom indicated that lamotrigine was only infrequently associated childhood. Median Patients Baseline reduction with at least seizure in seizure 50% seizure Number of frequency Dosage in mg/day frequency in reduction in patients (seizures/ (number of patients the lamotrigine the lamotrigine Reference randomized month) per group) group (%) group (%) Binnie et al. The 144 patients in the carbamazepine arm were randomly al data were utilized to compare lamotrigine with carbamazepine, a assigned to add-on lamotrigine (98 patients) and add-on carbamaz- better tolerability of lamotrigine was confrmed, but comparison of epine (46 patients) before withdrawing concomitant medication. Monotherapy was completed (at least 7 weeks) in 56% of lamotrig- ine patients and 54% of carbamazepine patients. Seizure freedom Conversion to monotherapy studies in refractory was attained during the monotherapy phase in 41% of lamotrigine epilepsies patients and 30% of carbamazepine patients. Neither of these difer- A double-blind, short-term active–control study in adolescents and ences was signifcant. Among the 158 patients in the valproic acid adults with refractory seizures further confrmed the efcacy of arm (105 assigned to lamotrigine and 53 to valproic acid), mono- lamotrigine in focal epilepsy [105]. A total of 156 patients on mon- therapy was completed in 49% of lamotrigine patients and 40% of otherapy with carbamazepine or phenytoin were assigned to receive valproic acid patients. While maintaining the concomitant freedom during the monotherapy phase with 32% versus 11% in drug at a steady dose level during baseline, the lamotrigine group favour of lamotrigine. Lamo- Monotherapy studies in newly diagnosed, trigine dosage was adjusted in the valproic acid group as valproic predominantly focal, epilepsy acid was withdrawn. In the remaining groups, serum lamotrigine As monotherapy, lamotrigine was reported to be no less efective concentrations rose as the concomitant drug was withdrawn. One study limited pathic’ tonic–clonic seizures (61%) than in those with focal seizures to focal epilepsy [108] allowed inclusion of 233 patients between 2 (43%). Tree studies [80,108,111] recruited elderly pa- statistical signifcance was reached for the focal seizures group only. Lamotrigine and carbamazepine were similar in efca- Although the valproic acid group experienced better seizure control cy, when evaluated in a diverse range of patient populations. How- during the add-on phase than the other groups, more patients in the ever, they difered in tolerability, because withdrawal secondary to valproic acid group tended to deteriorate during the phase of con- treatment-emergent adverse events was more likely with carbamaz- version to lamotrigine monotherapy. Tese results were interpreted epine, possibly most signifcantly in children and particularly in the as evidence of synergism between lamotrigine and valproic acid. In the studies for which only one seizure was A multicentre study from Poland recruited two equal groups of required for entry [25,108], seizure freedom attained tended to be 63 patients with uncontrolled focal or generalized seizures on mon- higher for both agents, without statistically signifcant diferences. The four study In a randomized comparative trial, lamotrigine and phenytoin phases consisted of a 4-week lamotrigine dose escalation, an 8-week were similarly efective [112] in terms of time to the frst seizure and lamotrigine add-on therapy, an 8-week carbamazepine–valproic time to discontinuation. The 181 recruited patients ranged from 14 acid withdrawal if clinically appropriate, and an 8-week lamotrigine to 75 years of age, and patients with primary generalized tonic– monotherapy. Adverse events led to discontinuation tion and add-on therapy, and 85 (68%) completed the lamotrigine of 13 patients (15%) in the lamotrigine group and 18 (19%) in the monotherapy phase.
Diseases
The secondary outcomes were time from randomization epilepsies to a frst seizure generic aciphex 20 mg on line gastritis diet information, time to 2-year remission aciphex 10 mg with mastercard gastritis aguda, the incidence of clinically The efcacy of lamotrigine monotherapy in patients with newly important adverse events and adverse efects emerging afer rand- diagnosed childhood absence epilepsy was demonstrated in three omization generic aciphex 10mg line gastritis diet forum. Carbamazepine had a non-signifcant advantage over blind dose escalation phase [119]. In the subsequent double-blind, lamotrigine, topiramate and oxcarbazepine for time to 12-month placebo-controlled phase restricted to patients who had respond- remission. A per-protocol analysis supported non-inferiority of ed to open-label treatment, signifcantly more patients remained lamotrigine compared with carbamazepine. The results for arm B of seizure-free among those randomized to continue lamotrigine the study are reported in the section ‘Monotherapy studies in newly (62%, n = 15) than in those switched to placebo (21%, n = 14). In the second trial, 38 children (3–13 years of age) were randomly assigned to lamotrigine or valproic acid according to an open-label Adjunctive therapy studies in generalized epilepsies design [120]. At 3 months, 63% of children taking valproic acid and In a multicentre double-blind cross-over study, a total of 26 pa- 37% of those taking lamotrigine were controlled. Afer 12 months, tients with various generalized epilepsies, including absence, were 68% of children taking valproic acid and 53% taking lamotrigine randomized to lamotrigine (at a maintenance dose of either 75 or remained seizure-free. Twenty-two patients completed signifcant, possibly because of the limited sample size. A greater than 50% seizure reduction A truly pivotal randomized double-blind trial of lamotrigine in occurred in 50% of patients with tonic–clonic seizures and in 33% comparison with valproic acid and ethosuximide in the treatment of those with absence seizures. In the continuation phase, fve pa- of childhood absence epilepsy was conducted more recently by tients (25%) remained seizure-free. All drugs were titrated according to clinical re- In a single-centre study employing an innovative design [80], sponse with maximal target doses of 60 mg/kg/day or 2000 mg/day 17 of 30 patients (57%) experienced a greater than 50% seizure for ethosuximide, 60 mg/kg/day or 3000 mg/day for valproic acid reduction when lamotrigine was added on in an initial open-label and 12 mg/kg/day or 600 mg/day for lamotrigine, and the children phase. Fifeen of the responders were then assigned, according to remained in the trial unless treatment had failed. At the 16-week as- a double-blind cross-over design, to lamotrigine or placebo afer a sessment, the primary comparison based on freedom-from-failure washout period, with the two double-blind phases consisting of 12- rates showed that lamotrigine (29% freedom-from-failure rate) was week periods separated by a 3-week cross-over. With the exception signifcantly inferior to both ethosuximide and valproic acid (53% of a single patient, the seizure count was lower during the lamo- and 58%, respectively), mainly due to inferior efcacy. Twenty of the 30 patients recruited at initiation had follow-up at 12 months, freedom-from-failure rates remained low- Lennox–Gastaut syndrome, and 11 of these patients (65%) were in er with lamotrigine (21%) than for ethosuximide and valproic acid the responder group. Almost two-thirds of the 125 The efcacy of lamotrigine in the management of Lennox– children with treatment failure as a result of lack of seizure control Gastaut syndrome was demonstrated in a double-blind, add-on were in the lamotrigine cohort. A higher rate of attentional dys- study [102] in which a total of 169 patients were randomized to function, already present at 16–20 weeks in the valproic acid group 16 weeks’ treatment with lamotrigine (n = 79) or placebo (n = 90). Based on these fndings, ethosuximide was consid- well as proportion of patients with greater than 50% seizure reduc- ered to represent the treatment of choice for childhood absence tion was signifcantly higher in the lamotrigine group than the pla- epilepsy, being superior to lamotrigine in efcacy and superior to cebo group. In this arm of the study, valproic acid was quency of primary generalized tonic–clonic seizures occurred in better than lamotrigine for time to 12-month remission, where- Lamotrigine 507 as topiramate was inferior to both valproic acid and lamotrigine Risk of seizure aggravation mainly in terms of tolerability. Lamotrigine can aggravate myoclonus [141,142,143,144,145] and even precipitate myoclonic status epilepticus [143], although im- Other studies proved control has also been reported in some cases [80]. In a A large number of experiential clinical studies have documented recent prospective open-label trial from Cuba, 72 patients with the place of lamotrigine in epilepsy treatment [25,46,80,123,124,12 juvenile myoclonic epilepsy were randomized to valproate or lamo- 5,126,127,128,129,130]. In an open study, for example, 21 patients trigine, the primary end-points being time from randomization to (16–65 years old) with epileptic seizures of frontal lobe origin were treatment failure and time from randomization to seizures remis- maintained on a combination of lamotrigine and valproic acid [131]. Lamotrigine was efective on both end-points and no At the end of 1 year, 17 patients continued on this combination and signifcant diference was seen between the two groups. Treatment outcome of some epilepsy syn- Dravet syndrome in whom lamotrigine use led to decreased seizure dromes was quantitatively evaluated with electroencephalogram duration and frequency. Myoclonus can represent a new symptom when lamotrigine verse events were recorded and compared with the patient’s treat- is initiated in a patient with genetically determined forms of epilepsy ment history as own control. Tere is a single case report of recurrent Successful applications of lamotrigine in refractory epilepsy have absence status epilepticus associated with lamotrigine therapy [149]. A comprehensive review of the rapidly ex- trigine is retained during chronic use, mostly in patients with re- panding literature on this topic is beyond the scope of this chapter. In one study of longer than 3 years’ duration, Lamotrigine has also been shown to be efective in the management the proportion of patients retained on lamotrigine treatment was of acute and chronic pain [152]. Another multicentre study of 6 years’ duration, in mostly difcult-to-treat patients, demonstrated a retention rate of some- Adverse effects what less than 40% [138]. The same study demonstrated that fewer than 4% of the patients remained free of seizure recurrences. Tere Overview of the most common adverse effects also exists the need to better defne the efcacy of lamotrigine in Assessment of the tolerability profle of lamotrigine has been generalized epilepsies [138]. Adverse events necessitated withdrawal of adjunctive Quality of life assessments lamotrigine therapy in 10. Of these, skin rash was most frequently in newly diagnosed epilepsy with health-related quality of life as cited, and was responsible for discontinuation in 3. The population was identical to that The most common adverse events associated with adjunctive lamo- of an already reviewed trial [80] that demonstrated a diference trigine use were primarily neurological, gastrointestinal and derma- in study completion rate (lamotrigine 65% versus carbamazepine tological. Skin rash was reported by 10% of lamotrigine patients, but dysphoria and tiredness subscales. Improvement observed among the diference compared with the placebo group was not signifcant. Addition of lamotrigi- did not difer signifcantly between lamotrigine and gabapentin ne was tolerated in 155 patients, and lamotrigine monotherapy was [108,113]. In two studies comparing lamotrigine and valproic acid successfully established in 51 patients. The lamotrigine monothera- in newly diagnosed patients, diferences in rates of withdrawal from py group experienced an improvement in mood measures. Lamotrigine was implicated in three, and all three patients experienced interictal events, consisting of delirium in two Lamotrigine, Carbamazepine, Phenytoin and mood disorder in one. Schizophrenia-like psychotic symptoms Study total [80,112,131] total [80,131] [112] were reported in six patients receiving lamotrigine for epilepsy n 536 338 95 [162]. Tourette symptoms were provoked in a single patient with a Daily dose 100–200 mg 600 or 400 mg 300 mg bipolar disorder [163]. Additional neurobehavioural adverse expe- Headache 99 (18%) 53 (17%) 18 (19%) riences include aggression [164] and insomnia [155]. Sporadic reports suggest an association of lamotrigine use with Asthenia 79 (15%) 69 (20%) 28 (29%) chorea without a family history [165,166,167]. Tere is a single case Rash 57 (11%) 47 (14%) 9 (9%) report of downbeat nystagmus [168]. Sleepiness 43 (8%) 58 (17%) 27 (29%) Neuroendocrine effects Dizziness 49 (9%) 43 (13%) 11 (12%) In a double-blind trial comparing lamotrigine (100–500 mg/ day) with valproic acid (10–60 mg/kg/day) monotherapy in 38 patients, among the adolescent patients (12–20 years old), body weight gain was more common in the valproic acid group Pooled data from 536 patients with newly diagnosed epilepsy during the 24 weeks of the maintenance phase, and the diference treated with lamotrigine monotherapy identifed headache (18%), between the two groups was signifcant at 10 weeks [170]. In an- asthenia (15%), rash (11%), nausea (10%), dizziness (9%) and other monotherapy comparison, there was a suggestion of a sub- somnolence (8%) as the most frequent adverse events (Table 38. When compared with carbamazepine and pheny- group, but only a small number of obese females had a polycystic toin, lamotrigine showed tolerability advantages in terms of a lower ovarian syndrome [171]. In fact, insomnia can be an adverse efect (n = 119) and valproic acid (n = 103) monotherapy for longer than of lamotrigine [155]. Tolerability data available from studies com- 5 years were compared in an open-label study [172]. More lamo- paring lamotrigine with gabapentin or valproic acid are more lim- trigine patients (87%) than valproic acid patients (77%) reported ited than those available for carbamazepine and phenytoin.