
North Dakota State University--Fargo. F. Steve, MD: "Buy cheap Rumalaya no RX - Best Rumalaya".
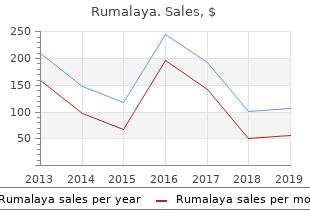
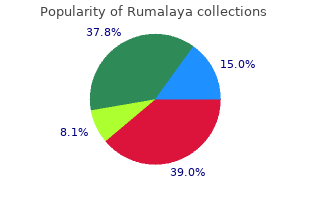
Dissection is a separation between the intimal and medial layers of the aortic wall order rumalaya without prescription symptoms 2 weeks pregnant, creating a false lumen for blood flow (Figs 60pills rumalaya amex symptoms 2 weeks pregnant. Both the true and false lumens fill with blood during82 systole generic rumalaya 60pills otc treatment neuropathy, but only the true lumen has blood flow during diastole. Intramural hematoma is considered a precursor of dissection and should be treated similarly. Cardiac Masses Cardiac tumors either can originate from the heart or are metastases from other sites. The most common primary tumor is myxoma, which is located most frequently at the interatrial septum (Fig. The potential of 1882 myxomas to obstruct the inflow or outflow region of a ventricle is demonstrated with Doppler echocardiography. Pacemaker wires, thrombus, and normal anatomic structures that mimic the appearance of pathology (Eustachian valve, crista terminalis, Chiari network, or “Coumadin” ridge) should be differentiated from tumors. Ultrasound-guided Central Vein Cannulation The placement of central venous catheters is associated with complications including injury to vascular structures (carotid artery), pleura, nerve bundles, lymphatic system, and even the spinal canal. Historically, anatomic landmarks guided needle orientation during central venous access. However, multiple studies have demonstrated that the anatomic relationship between the internal jugular vein and the carotid artery varies and that even experienced physicians encounter complications. Visual guidance by ultrasound provides85 real-time feedback, reducing the complication rate and the procedure time. In the midesophageal four-chamber view, a color-Doppler sector is positioned over the interatrial septum. The American Society of Echocardiography in collaboration with the Society of Cardiovascular 1886 Anesthesiologists has issued guidelines for the performance of epicardial echocardiography. The guide wire is seen as a thin echo-dense linear structure positioned in the lumen of the vein. Epiaortic scanning for atheroma is performed using a small footprint, linear array transducer. The echocardiography report from a preoperative examination is useful for assessing surgical risk and developing the anesthetic plan. Echocardiography has also established itself as particularly valuable in the assessment of postoperative hemodynamic instability. It offers rapid diagnosis by differentiating among the potential complications faced in postoperative care, such as hypovolemia, pericardial tamponade aortic dissection, myocardial infarction, endocarditis, and pulmonary embolism. Advancements in portable ultrasound technology have led to the wide availability of these devices throughout the hospital. As such, focused exams are increasingly performed at the bedside as an adjunct to the clinical exam by anesthesiology and critical care physicians lacking advanced training in echocardiography. The importance of structured training and maintenance of competencies has been recognized by 1888 professional societies as essential components to fully utilize the advantages and minimize drawbacks of this type of cardiac ultrasound examination. The aortic valve (arrow) is thickened and heavily calcified with restricted mobility. Focused Exam Views A focused cardiac examination uses transthoracic echocardiographic images obtained from the parasternal, apical, and subcostal windows. In 1889 addition, most of the cardiac abnormalities sought out can be easily recognized from these windows. Parasternal views are obtained in the third intercostal space at the left sternal border with the patient in left lateral position. Apical views are obtained at the point of maximal impulse (apex) with the patient in the left lateral position. The apical four-chamber view (A-4Ch) is obtained by aligning the probe notch to the left of the patient (Fig. Subcostal views are obtained from below the xiphoid process with the patient in supine position. The subcostal four-chamber view is obtained by aligning the probe notch to the patient’s left side (Fig. Table 27-10 Common Clinical Conditions and Associated Focus Targets Focused Assessed Transthoracic Echo Multiple focused ultrasound protocols have been proposed for detection of cardiac abnormalities at bedside. In addition, this protocol involves lung ultrasound imaging which is useful to identify pleural effusions, 1890 lung edema, and pneumothorax. Panel D: Subcostal four- chamber view (Subcostal) obtained with the probe positioned below the xiphoid process and marker pointing toward the left flank. Ventricular function in children during halothane anesthesia: an echocardiographic evaluation. Intraoperative transesophageal echocardiography: 5-year prospective review of impact on surgical management. Impact of routine use of intraoperative transesophageal echocardiography during cardiac surgery. Transesophageal echocardiography in cardiac and vascular surgery: implications and observer variability. The influence of transesophageal echocardiography on intra-operative decision making. Perioperative use of transesophageal echocardiography by anesthesiologists: impact in noncardiac surgery and in the intensive care unit. American Society of Anesthesiologists and the Society of Cardiovascular Anesthesiologists Task Force on Transesophageal Echocardiography. American Society of Anesthesiologists, Society of Cardiovascular Anesthesiologists Task Force. Practice guidelines for perioperative transesophageal echocardiography: An update report by the American Society of Anesthesiologists and the Society of Cardiovascular Anesthesiologists Task Force on Transesophageal Echocardiography. Quality assurance for intraoperative transesophageal echocardiography monitoring: a report of 846 procedures. The safety of intraoperative transesophageal echocardiography: a case series of 7200 cardiac surgical patients. Risk of dysphagia after transesophageal echocardiography during cardiac operations. Guidelines for performing a comprehensive intraoperative multiplane transesophageal echocardiographic 1893 examinations: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. The adequacy of basic intraoperative transesophageal echocardiography performed by experienced anesthesiologists. Basic perioperative transesophageal echocardiography examination: a consensus statement of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. Three-dimensional transesophageal echocardiography is a major advance for intraoperative clinical management of patients undergoing cardiac surgery: a core review. Usefulness of transesophageal three- dimensional echocardiography in the identification of individual segment/scallop prolapse of the mitral valve. Recommendations for quantification of Doppler echocardiography: a report from the Doppler Quantification Task Force of the Nomenclature and Standards Committee of the American Society of Echocardiography. Intraoperative determination of cardiac output using multiplane transesophageal echocardiography: a comparison to thermodilution. Multiplane transesophageal echocardiography acquisition of ascending aortic flow velocities: a comparison with established techniques.
However purchase genuine rumalaya on line medicine emblem, despite the longer elimination half-time of sufentanil generic rumalaya 60 pills visa medications like abilify, its context-sensitive half-time is actually less than that of alfentanil for infusions up to 8 hours in duration discount 60pills rumalaya with amex medicine cards. This phenomenon is explained in part by the huge distribution volume of sufentanil. After termination of a sufentanil infusion, the decay in plasma drug concentrations is accelerated not only by elimination but also by the continued redistribution of sufentanil into peripheral compartments. On the other hand, the small distribution volume of alfentanil equilibrates rapidly; therefore, peripheral distribution of drug away from the plasma is not a significant contributor to the decay in plasma concentration after an infusion. Thus, despite its short elimination half-time, alfentanil may not necessarily be superior to sufentanil. Although the context-sensitive half-time represents a significant advance in our ability to describe drug disposition, this parameter does not directly describe how long it will take the patient to recover from monitored anesthesia care. The context-sensitive half-time merely describes how long it will take for the plasma concentration of the drug to decrease by 50%. The difference between the plasma concentration at the end of the infusion and the plasma concentration below which awakening can be expected is an obvious factor in determining time to recovery. For example, if the drug concentration is maintained at a level just above that required for awakening, the time to recovery will be more rapid than after an infusion during which the drug concentration is much greater than that required for awakening (Fig. Furthermore, although context-sensitive half-time is a reflection of plasma drug decay, awakening from anesthesia is actually a function of effect site (i. Changes in effect site concentration demonstrate a variable time lag behind changes in plasma drug concentration. When a drug is administered intravenously by bolus or infused rapidly, there is a delay before the onset of clinical effect. This delay occurs because the plasma is not usually the site of action but is merely the route by 2054 which the drug reaches its effect site. Drugs with a short t1/2 e0k will equilibrate rapidly with the brain and have a shorter delay in onset than drugs that have a longer t1/2 e0k. Thiopental, propofol, and alfentanil have short t1/2 e0k values compared with midazolam, sufentanil, and fentanyl. Figure 30-3 The context-sensitive half-time is not the sole determinant of the time it takes for the patient to awaken. This parameter merely reflects the time taken for the plasma concentration of a drug to decrease by 50%. The time to awakening is determined in addition by the difference in concentration at the end of the procedure and the concentration below which awakening will occur. The t1/2 e0k allows predictions to be made of the time course of equilibration of the drug between the blood and the brain. Therefore, if an opioid is required to blunt the response to a single brief stimulus, alfentanil might represent a logical choice over fentanyl. The t1/2 e0k is an important determinant of bolus spacing when titrating drugs to clinical effect. In the case of drugs like midazolam and propofol, boluses of drug should be spaced far enough apart to allow the full peak effect to be clinically appreciated before further drug administration in order to avoid inadvertent overdosing. For 2055 example, a low cardiac output will markedly delay drug arrival at the site of action. If sufficient time is not given for the drug to take effect before giving additional drug increments, significant cardiorespiratory compromise may occur. Furthermore, the effects of initial doses of most drugs in anesthetic practice are terminated by redistribution, which depends on blood flow to redistribution sites. If there is reduced blood flow to redistribution sites because of pre-existing and iatrogenic decreases in cardiac output, the dangerous adverse effects of these drugs are likely to be both delayed and markedly prolonged. An example of this scenario is the patient with a hemodynamic compromise caused by a tachydysrhythmia who requires sedation for cardioversion. Careful, well-spaced, small boluses of drug should be given to induce the appropriate level of sedation, bearing in mind that it may take several minutes for the full effect of a small bolus dose to become apparent. Drug Interactions At the present time, no single drug can provide all the components of monitored anesthesia care (i. By acting synergistically, combinations of drugs enable reductions in the dose requirements of individual drugs. For example, the combination of propofol and fentanyl by infusion has been shown to produce a more rapid recovery and better stress response abolition than the use of propofol alone. However, synergistic interaction may also extend to the undesirable interactions of the drugs such as cardiorespiratory depression. Drug interactions may have both a pharmacodynamic and a pharmacokinetic basis and may vary depending on the combination of drugs being coadministered, the dose range over which these drugs are administered, and the specific clinical effect that is measured. For example, because fentanyl is primarily an analgesic rather than a hypnotic, it reduces propofol requirements for suppression of response to skin incision to a much greater degree than it reduces propofol requirements for induction of anesthesia. On the other hand, because midazolam has significant hypnotic16 properties, it displays significant synergism with propofol or thiopental when used to induce hypnosis for prevention of movement in response to a painful stimulus. For example, during general20 anesthesia, opioid requirements to suppress the responses to noxious stimuli are tenfold higher when used as the sole agent compared with when they are used in conjunction with a nitrous oxide/potent inhaled vapor technique. This interaction persists at the lighter levels of anesthesia encountered during monitored anesthesia care. Therefore, it is likely that a rapid recovery would be facilitated by using opioids in combination with other agents (e. However,17 when the dose of fentanyl is increased, there is no significant further reduction of the Cp 50 for propofol beyond a fentanyl concentration of 3ss ng/mL. Although the data presented here pertain to patients under general anesthesia, these findings have important implications for monitored anesthesia care. These studies demonstrate that the potentiating effects of opioids on coadministered sedatives are pronounced within the dose range commonly used during monitored anesthesia care. Furthermore, the data suggest that the dose–response curve is likely to be steep within this dose range, thus supporting the clinical impression that significant increases in depth of sedation can occur with only modest increments in opioid or hypnotic/sedative dosage. The following clinical recommendations can be made: During monitored anesthesia care, the maximum benefit of opioid supplementation, in terms of potentiation of other administered sedatives, will accrue when the opioid is used in the analgesic dose range. Opioid and benzodiazepine combinations are frequently used to achieve the components of hypnosis, amnesia, and analgesia. Approximately 25% of the median effective dose for each individual drug is required in combination to induce hypnosis in 50% of patients. If the combination were simply26 additive, hypnosis would be induced in only approximately 25% of patients. Even subanalgesic doses of alfentanil (3 μg/kg) produce a profound reduction in midazolam requirements for hypnosis. This synergism also extends to the27 unwanted effects of these drugs, producing the life-threatening complications of respiratory and cardiac depression.
Order 60pills rumalaya free shipping. 8 Signs of Dehydration in Dogs.
Relative influence on total cancelled operating room time from patients who are inpatients or outpatients preoperatively cheap 60pills rumalaya with visa medications used to treat bipolar. Risk assessment for respiratory complications in paediatric anaesthesia: a prospective cohort study generic 60pills rumalaya with visa medicine that makes you throw up. Hydration status after overnight fasting as measured by urine osmolality does not alter the magnitude of hypotension during general anesthesia in low risk patients buy rumalaya 60 pills cheap 9 medications that cause fatigue. Hunger and thirst numeric rating scales are 2134 not valid estimates for gastric content volumes: a prospective investigation in healthy children. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Committee on Standards and Practice Parameters. A comparison of three doses of a commercially prepared oral midazolam syrup in children. Effects of age and emotionality on the effectiveness of midazolam administered preoperatively to children. Efficacy spectrum of antishivering medications: meta-analysis of randomized controlled trials. Pharmacological interventions for prevention or treatment of postoperative pain in people undergoing laparoscopic cholecystectomy. Analgesic effectiveness of acetaminophen for primary cleft palate repair in young children: a randomized placebo controlled trial. Acetaminophen plus a nonsteroidal anti-inflammatory drug decreases acute postoperative pain more than either drug alone. Outcomes and charges associated with outpatient inguinal hernia repair according to method of anesthesia and surgical approach. Anaesthesia and post-operative morbidity after elective groin hernia repair: a nation-wide study. Neuraxial anesthesia improves long-term survival after total joint replacement: a retrospective nationwide population-based study in Taiwan. Peripheral regional anaesthesia and 2135 outcome: lessons learned from the last 10 years. Predictors of failure of awake regional anesthesia for neonatal hernia repair: Data from the general anesthesia compared to spinal anesthesia study-comparing apnea and neurodevelopmental outcomes. Comparison of bupivacaine and 2- chloroprocaine for spinal anesthesia for outpatient surgery: a double-blind randomized trial. Neuraxial analgesia in neonates and infants: a review of clinical and preclinical strategies for the development of safety and efficacy data. Continuous interscalene block in patients having outpatient rotator cuff repair surgery: a prospective randomized trial. A regional anesthesia-based “swing” operating room model reduces non-operative time in a mixed orthopedic inpatient/outpatient population. Post-anaesthesia care unit stay after total hip and knee arthroplasty under spinal anaesthesia. Ultrasound-guided transversus abdominis plane catheters and ambulatory perineural infusions for outpatient inguinal hernia repair. Total elbow arthroplasty as an outpatient procedure using a continuous infraclavicular nerve block at home: a prospective case report. Continuous popliteal sciatic nerve block for outpatient foot surgery—a randomized, controlled trial. Continuous epidural block versus 2136 continuous popliteal nerve block for postoperative pain relief after major podiatric surgery in children: a prospective, comparative randomized study. Reduction of verbal pain scores after anterior cruciate ligament reconstruction with 2-day continuous femoral nerve block: a randomized clinical trial. Ambulatory continuous interscalene nerve blocks decrease the time to discharge readiness after total shoulder arthroplasty: a randomized, triple-masked, placebo-controlled study. Ambulatory continuous peripheral nerve blocks in children and adolescents: a longitudinal 8-year single center study. Continuous peripheral nerve blocks in the ambulatory setting: an update of the published evidence. Ability of a meta-analysis to prevent redundant research: systematic review of studies on pain from propofol injection. Nitrous oxide-related postoperative nausea and vomiting depends on duration of exposure. Genetic factors associated with pharmacotherapy and background sensitivity to postoperative and chemotherapy-induced nausea and vomiting. Aprepitant plus ondansetron compared with ondansetron alone in reducing postoperative nausea and vomiting in ambulatory patients undergoing plastic surgery. Cancer recurrence and hyperglycemia with dexamethasone for postoperative nausea and vomiting prophylaxis: more moot points? Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. The efficacy of several neuromuscular monitoring modes at the P6 acupuncture point in preventing postoperative nausea and vomiting. Incidence and predictors of postdischarge nausea and vomiting in a 7-day population. The relationship of pain and nausea in postoperative patients for 1 week after ambulatory surgery. Dose-dependent association between intermediate-acting neuromuscular-blocking agents and postoperative respiratory complications. Predictors and clinical outcomes from failed Laryngeal Mask Airway Unique: a study of 15,795 patients. A comparison of ondansetron with promethazine for treating postoperative nausea and vomiting in patients who received prophylaxis with ondansetron: a retrospective database analysis. The effects of oral ibuprofen and celecoxib in preventing pain, improving recovery outcomes and patient satisfaction after ambulatory surgery. Single-dose systemic acetaminophen to prevent postoperative pain: a meta-analysis of randomized controlled trials. Risk factors associated with fast-track ineligibility after monitored anesthesia care in ambulatory surgery patients. Changing access to emergency care for patients undergoing outpatient procedures at ambulatory surgery centers: evidence from Florida. Twenty-one percent of the reported injuries sustained in offices were temporary and nondisabling in 2139 nature and 64% were permanent or led to death, whereas 62% of the injuries sustained in ambulatory surgical centers were temporary and nondisabling and only 21% were permanent or led to death. An ambulatory anesthetic is defined as one in which the patient arrives to the surgical venue on the day of the procedure, is anesthetized, and is discharged home later that same day. The surgical/medical office often provides practitioners with the 2140 space for other activities such as consultation with new patients, the performance of routine history and physicals, and office administration. Along with providing safe anesthetics across the spectrum of young to old, and healthy to medically challenged patients undergoing increasingly complex procedures, the anesthesiologist must understand office safety and policy, legal and financial issues such as antitrust laws, state laws or regulations that may exist, the need for possible accreditation and billing and collection issues. In 1856, John Snow documented his experience in providing anesthesia with chloroform for 867 dental patients, and approximately 3,021 teeth were extracted in private dental offices under his care.
A controlled myocardial infarction feels very much like an uncontrolled one so deep sedation will be necessary for the injection portion of the procedure buy genuine rumalaya online treatment 4 syphilis. Structural Heart Procedures Transcatheter Aortic Valve Replacement Calcific aortic stenosis affects almost 5% of adults over the age of 65 order 60 pills rumalaya with amex symptoms of. Rapid ventricular pacing is used to92 minimize left ventricular ejection so that the new valve can be deployed into the correct position generic rumalaya 60 pills amex medications herpes. The92 compressed CoreValve is slowly deployed as its delivery system is pulled back and allows for some repositioning before the valve is fully released. This valve expands with a balloon within the native valve with the goal of displacing the native leaflets. These patients are at high risk for cardiac death during94 the procedure and experience frequent hemodynamic instability during the rapid ventricular pacing that is required for balloon valvuloplasty and for valve deployment. The large cannulae that are exchanged in and out of the groin during the procedure can result in a surprising drop in hematocrit which should be checked frequently during the procedure. One-lung ventilation may be helpful for both the transapical approach and when directly cannulating the ascending aorta, which can be accomplished with either a double lumen tube or a bronchial blocker. The goal for most of these procedures is to extubate the patient in the procedure room or shortly thereafter. Many of the patients are elderly and at high risk for delirium; thus, benzodiazepines and long-acting opioids should be avoided if possible. The MitraClip delivers a clip device percutaneously that mimics the98 Alfieri edge-to-edge repair to create a double orifice mitral valve (Figs. As well, mortality associated with the MitraClip is less than with surgery using the predicted outcomes surgical risk predictors. Red arrow points between P1 (left) and P2 prolapsing segments of the posterior leaflet with flail chordae visible. Purple arrow shows where the two clips have been placed between A2 and P2 segments of the mitral valve. The device has been shown to reduce hemorrhagic stroke and cardiovascular death when compared to warfarin although there is an increased incidence of ischemic stroke as a periprocedural event. Arterial catheters should be used to measure arterial blood pressure for most of these procedures. These devices are usually implanted in the left pectoral area with one to three transvenous leads inserted into the axillary, subclavian, or cephalic veins. General anesthesia may be necessary for threshold testing in patients with left ventricular dysfunction. Ablation catheters are inserted via the femoral veins into the right heart to try to induce arrhythmias. Complex mapping techniques localize the source of the arrhythmia and an energy source is applied to ablate this source. Ablations can be performed with either radiofrequency or cryothermy with the former being much more stimulating for the patient. Avoidance of neuromuscular blockade will alert the electrophysiologist to phrenic irritation when this area is being ablated. The ablation 2214 process can also be painful and general anesthesia may be required. Invasive arterial blood pressure monitoring is helpful in these patients, especially for those with reduced ejection fractions in whom hemodynamically unstable arrhythmias might be induced. Device infections, lead endocarditis, thrombosis or venous stenosis, chronic pain due to leads/device, and nonfunctional leads are all reasons for lead removal. Vascular injury causing significant blood loss and cardiac tamponade is rare but the involved clinicians should be prepared for it. As expected, centers with higher lead extraction volume have a lower probability of complications and death. Elective electrical cardioversions are ideally performed with a bolus of propofol on fully monitored patients under the supervision of an anesthesiologist. The seizure usually lasts several minutes and minimum seizure duration of 25 seconds is recommended to ensure adequate antidepressant efficacy. Other sequelae include myalgias, bone fractures, joint dislocations, headache, emergence agitation, status epilepticus, and sudden death. Of these drugs, the monoamine oxidase inhibitors have the most significant interactions with anesthetic agents. Propofol is more effective at attenuating the acute hemodynamic responses than etomidate and in small doses (0. This increase has resulted in an expansion of anesthesia services in areas remote from the operating room that may not be familiar to anesthesia providers. This approach involves giving careful consideration to the evaluation and the needs of the patient, the particular challenges posed by the procedure, and the hazards and limitations of the environment. In all cases, the standards of anesthesia care and monitoring should be no different than those provided in the conventional operating room. Complications of non-operating room procedures: outcomes from the National Anesthesia Clinical Outcomes Registry. Risks of anesthesia or sedation outside the operating room: the role of the anesthesia care provider. Capnography enhances surveillance of respiratory events during procedural sedation: a meta-analysis. Adopting a surgical safety checklist could save money and improve the quality of care in U. Adverse clinical events during intrahospital transport by a specialized team: a preliminary report. Approved by the House of Delegates on October 25, 2005, and last amended on October 16, 2013. Continuum of depth of sedation: definition of general anesthesia and levels of sedation/analgesia. Occupational radiation protection in interventional radiology: a joint guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. Radiation exposure to operating room personnel and patients during endovascular procedures. The 2007 Recommendations of the International Commission on Radiological Protection. Contrast-induced nephropathy: identifying the risks, choosing the right agent, and reviewing effective prevention and management methods. Immediate drug hypersensitivity: epidemiology, clinical features, triggers and management. Contrast media controversies in 2015: imaging patients with renal impairment or risk of contrast reaction. International subarachnoid aneurysm trial of neurosurgical clipping versus endovascular coiling: subgroup analysis of 278 elderly patients. Guidelines for the management of patients with unruptured intracranial aneurysms: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association.