
New College of Florida. K. Ugrasal, MD: "Order Cefixime online in USA - Best Cefixime".
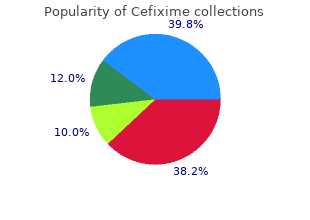
These academic departments tend to be among the larger groups of anesthesiologists purchase genuine cefixime online antibiotic used to treat bv, but the aggregate fraction of the entire anesthesiologist population is small discount cefixime 100mg fast delivery bacteria 4kids. It is interesting order cefixime with amex antibiotic used to treat uti, however, that by the nature of the system, most residents and fellows finishing their training have almost exclusively been exposed only to academic anesthesiology. Accordingly, finishing trainees in the past often were comparatively unprepared to evaluate and enter the anesthesiology job market. Some finishing trainees (residents or fellows) who know they are eventually headed for private practice have started their attending careers as full-time junior faculty in an academic department. Most trainees, however, do not become junior faculty; they accept positions in practice immediately. Academic Practice For those who choose to stay in academic practice, a number of specific characteristics of academic anesthesia departments can be used as screening questions. Junior faculty sometimes can get lost in very big departments and be treated as little better than glorified senior residents. On the other hand, the availability of subspecialty service opportunities and significant research and educational resources can make large departments extremely attractive. In smaller academic departments, there may be fewer resources, but the likelihood of being quickly accepted as a valued and contributing member of the teaching faculty (and research team, if 164 appropriate) may be higher. In very small departments, the number of expectations, projects, and involvements could potentially be overwhelming. In addition, a small department may lack a dedicated research infrastructure, so it may be necessary for the faculty in this situation to collaborate with other, larger departments to accomplish meaningful academic work. If teaching one resident class every other week is standard, the candidate must enthusiastically accept that assignment and the attendant preparation work and time up front. Likewise, if it is expected that junior faculty will, by definition, be actively involved in publishable research, specific plans for projects to which the candidate is amenable must be made. In such situations, clear stipulations about startup research funding and nonclinical time to carry out the projects should be obtained as much as possible (although clinical workload demands and revenue generation expectations may make this very difficult in some settings). Particularly important is determining what the expectation is concerning outside funding. For example, it can be a rude shock to realize that projects will suddenly halt after 2 years if extramural funding has not been secured. Many new junior faculty directly out of residency start with medical school appointments as instructors unless there is something else in their background that immediately qualifies them as assistant professors. It is wise to understand from the beginning what it takes in that department and medical school to facilitate academic advancement. There may be more than one academic “track”; the tenure track, for example, usually depends on published research whereas the clinical or teacher track relies more heavily on one’s value in patient care and as a clinical educator. The criteria for promotion may be clearly spelled out by the institution—number of papers needed, involvement and recognition at various levels, grants submitted and funded, and so on—or the system may be less rigid and depend more heavily on the department chairman’s and other faculty evaluations and recommendations. In either case, careful inquiry before accepting the position can avert later surprise and disappointment. Traditionally, academic anesthesiologists have not earned quite as much as those in private practice—in return for the advantage of more predictable schedules, continued intellectual stimulation, and the intangible rewards of academic success. There is now great activity and attention concerning reimbursement of anesthesiologists, and it is difficult to predict future income for any anesthesiology practice situation. However, all of the forces influencing payment for anesthesia care may significantly diminish the traditional income differential between academic and private practice. In many cases, a faculty member is exclusively an employee of the institution or a component financial entity, which bills and collects or 165 negotiates group contracts for the patient care rendered by the faculty member, and then pays a negotiated amount (either an absolute dollar figure or a floating amount based on volume—or, especially, a combination of the two) that constitutes the faculty person’s entire income. Under other much less and less common arrangements, faculty members themselves may be able to bill and collect or negotiate contracts for their clinical work. Some institutions have an (comparatively small) academic salary from the medical school for being on the faculty, but many do not; some channel variable amounts of money (from the so-called Part A clinical revenue) into the academic practice in recognition of teaching and administration or simply as a subsidy for needed service. Usually, the faculty will be members of some type of group or practice plan (either for the anesthesia department alone or for the entire faculty as a whole) that bills and collects or negotiates contracts and then distributes the practice income to the faculty under an arrangement that must be examined by the candidate. In most academic institutions, practice expenses such as all overhead and malpractice insurance as well as reasonable benefits, including discretionary funds for meetings, subscriptions, books, dues, and so forth, are automatically part of the compensation package, which often may not be true in private practice and must be counted in making any comparison. An important corollary issue is that of the source of the salaries of the department’s primary anesthesia providers—residents and, in some cases, nurse anesthetists. Although the hospital usually pays for at least some and, often, most or all of these, arrangements vary, and it is important to ascertain whether the faculty practice income is also expected to cover the cost of the primary providers. Overall, it is appropriate for the candidate to ask probing questions about the commitment of the institution to the maintenance of reasonable compensation for faculty. Private Practice in the Marketplace Obviously, rotations to a private practice hospital in the final year of anesthesia residency could help greatly in regard to the realities of private practice, but not all residency programs offer such opportunities. In that case, the finishing trainee who is certain about going into traditional private practice must seek information on career development and mentors from the private sector. In the past, independent individual practice was a viable option for some versus a position with a group (sole proprietorship, partnership, or corporation) that functions as a single financial entity. Independent practice became increasingly less viable in many locations because of the need to be able to bid for contracts with health systems, practice facilities, or managed care entities. However, where independent practice may still be possible, it 166 usually first involves attempting to secure clinical privileges at a number of hospitals or facilities in the area in which one chooses to live. This may not always be easy, and this issue has been the subject of many (frequently unsuccessful) antitrust suits over recent years (see Antitrust Considerations). Then the anesthesiologist makes it known to the respective surgeon communities that he or she is available to render anesthesia services and waits until there is a request for his or her services. The anesthesiologist obtains the requisite financial information from the patient and then either individually bills and collects for services rendered or employs a service to do billing and collection for a percentage fee (which will vary depending on the circumstances, especially the volume of business; for billing [without scheduling services] it would be unlikely to be more than 7% or, at the most, 8% of actual collections). How much of the needed equipment and supplies will be provided by the hospital or facility and how much by the independent anesthesiologist has varied widely. If an anesthesiologist spends considerable time in one operating suite, he or she may purchase an anesthesia machine exclusively for his or her own use and move it from room to room as needed. It is likely to be impractical to move a fully equipped anesthesia machine from hospital to hospital on a day-to-day basis. Among the features of this style of practice are the collegiality and relationships of a genuine private practice based on referrals and also the ability to decide independently how much time one wants to work. The downside is the potential unpredictability of the demand for service and the time needed to establish referral patterns and obtain bookings sufficient to generate a livable income. The growing availability and ease of access for online job searching has allowed prospective anesthesiologists and potential employers often to locate suitable candidates without the expense of commercial placement services. However, the most recent trend appears to be increasing reliance on placement services because these concerns vet an applicant for the practices, saving time and energy, and only present “qualified candidates” who look like a potential good fit for the practice. Some of the screening questions by the applicant are the same as for an academic position, but there must be even more emphasis on the exact details of clinical expectations and financial arrangements. Some trainees finish residency (or fellowship even more so) very highly skilled in complex, difficult anesthesia procedures. They can be 167 surprised to find that in some private practice group situations, the junior- most anesthesiologist must wait some time, perhaps even years, before being eligible to do, for example, open heart anesthesia, and in the meantime will mostly be assigned more routine or less challenging anesthetics.
Contraction encompasses the isovolumic contraction and the first half of ejection discount cefixime 100mg without prescription antimicrobial and antifungal. The critical insight into the proposal of Nishimura and Tajik is that relaxation begins during the second part of ejection order cefixime 100mg with amex bacteria no estomago, and then continues during the isovolumic relaxation and rapid filling phases order generic cefixime on-line antibiotic resistance evolution, illustrating the interdependency of systole and diastole. The filling phase consists of the early rapid filling phase, diastasis, and atrial contraction. Myocardial velocity of basal anterolateral segment of left ventricle is measured with pulsed-wave tissue Doppler. A practical approach to the echocardiographic evaluation of ventricular diastolic function. Echocardiographic assessments have been validated by cardiac catheterization and correlate with clinical presentation. The American Society of Echocardiography has issued62 recommendations for evaluating and grading left ventricular diastolic function using a combination of 2D echocardiography, pulsed-wave Doppler, M-mode color Doppler, and tissue Doppler. Imaging Views and Techniques The echocardiographic acquisition of the diastolic parameters is best done when integrated in a standard examination. Therefore, the displayed velocity waveforms parallel the changes in pressure gradient occurring in the left heart. A normal profile has a 1868 biphasic diastolic component: the early diastolic wave E′, which represents the myocardial elongation caused by early filling, and the late diastolic wave A′, which represents the myocardial distension generated by blood flow during atrial contraction (Fig. Adapted from the 2016 Recommendations for evaluation of left 63 ventricular diastolic dysfunction by echocardiography. The forward filling velocity at atrial contraction is low (small A wave) because of the decreased compliance (Fig. One of the important caveats to assessing diastolic function using pulsed-wave Doppler is that the flow patterns depend on pressure gradients and therefore are affected by both preload and afterload. The updated guidelines utilize 4 criteria to65 diagnose diastolic dysfunction (Fig. Pericardial pathologies, such as constrictive pericarditis or pericardial tamponade, impede diastolic flow. Two-dimensional echocardiography can be helpful in differentiating among these pathologies. In constrictive pericarditis, the pericardium appears thick, fibrotic, calcified, and thus echogenic; the inferior vena cava is dilated and the ventricular septum has an abnormal motion. Pericardial effusions can be global, surrounding the entire heart, or loculated, as seen mostly after cardiac surgery (Fig. Since the intrapericardial volume is constant, cardiac chambers are compressed when at their lowest pressure (atria in systole, ventricles in diastole). In summary, diastolic filling is an active process and a major component of effective cardiac performance. Evaluation of Valvular Heart Disease Two-dimensional echocardiography and Doppler are complementary methods 1870 in valve assessment. The 2D echocardiography provides evaluation of valve anatomy and function; Doppler assesses the physiologic consequences and severity of the lesion. B: M-mode echocardiography demonstrates separation of the epicardium from the pericardium (asterisks) from pericardial effusion. However, for any given68 valve area, the flow velocity and pressure gradient vary with changes in stroke volume and cardiac output. The2 echocardiographic cut-off values for grading aortic stenosis are shown in Table 27-3. The leaflets can appear thickened and calcified (thus, strongly echogenic), and there may be fusion of the chordae and papillary muscles. The right ventricle may be dilated and/or hypertrophied, with thickened walls, because of increased pressure work (Fig. The increased diastolic pressure gradient is measured with continuous Doppler in the midesophageal four-chamber or long-axis view. The early diastolic velocity of the transmitral flow (E wave)67 is increased (usually >1. B: In the midesophageal bicaval view, red blood cell clumping creates spontaneous echocardiography contrast. The anterior mitral leaflet exhibits diastolic doming whereas the posterior mitral leaflet is immobile. A: Diastolic blood acceleration upstream of the mitral valve is seen with color-flow Doppler (“rising sun”). B: Spectral display of the diastolic velocity decay is imaged with a pulsed-wave Doppler sample volume placed at the tips of the mitral valve. Echocardiographic findings may include any of the following:77 abnormal texture of leaflets (myxomatous degeneration), flail and/or prolapsing leaflet, ruptured chordae, papillary muscle dysfunction or rupture (secondary to ischemia), mitral annulus calcification, or endocarditis lesions. The leaflet motion is commonly reported using Carpentier classification as described in Table 27-6. In routine cases, such as coronary artery bypass surgery, evaluation of the aorta may reveal previously unknown, significant atheromatous disease of the aorta and alter the surgical plan (off-pump bypass, alternative sites for cannulation). In emergencies, the diagnosis of aortic pathology (dissection, aneurysm, transection) may prove life-saving. Atherosclerotic plaques are irregularly shaped, sometimes mobile protrusions inside the aortic lumen. The search for atheromas should be done by imaging the entire circumference of the aortic lumen (short-axis views). Once a particular lesion is found, scanning in long-axis view should be performed (Fig. Ascending aorta aneurysm distal to the sinotubular junction (midesophageal ascending aorta long-axis (A) and short-axis (B) views). C: Ascending aorta dissection (Stanford type A) originating from the sinotubular junction. Color-flow Doppler demonstrates blood flow inside the true lumen (which expands in systole) and the absence of flow inside the false lumen. Dissection is a separation between the intimal and medial layers of the aortic wall, creating a false lumen for blood flow (Figs. Both the true and false lumens fill with blood during82 systole, but only the true lumen has blood flow during diastole. Intramural hematoma is considered a precursor of dissection and should be treated similarly. Cardiac Masses Cardiac tumors either can originate from the heart or are metastases from other sites. The most common primary tumor is myxoma, which is located most frequently at the interatrial septum (Fig. The potential of 1882 myxomas to obstruct the inflow or outflow region of a ventricle is demonstrated with Doppler echocardiography. Pacemaker wires, thrombus, and normal anatomic structures that mimic the appearance of pathology (Eustachian valve, crista terminalis, Chiari network, or “Coumadin” ridge) should be differentiated from tumors. Ultrasound-guided Central Vein Cannulation The placement of central venous catheters is associated with complications including injury to vascular structures (carotid artery), pleura, nerve bundles, lymphatic system, and even the spinal canal. Historically, anatomic landmarks guided needle orientation during central venous access.
Acute respiratory acidosis may require mechanical ventilation unless a simple etiologic factor (i purchase discount cefixime antimicrobial toilet seats. Bicarbonate administration is never indicated unless severe metabolic acidosis is also present or unless mechanical ventilation is ineffective in reducing acute hypercarbia order generic cefixime on-line antibiotics for dogs at feed store. In contrast 200mg cefixime free shipping antibiotics for sinus and throat infection, chronic respiratory acidosis is rarely managed with ventilation but rather with efforts to improve pulmonary function. In patients requiring mechanical ventilation for acute respiratory failure, ventilation with a lung-protective strategy may result in hypercapnia, which occasionally may require administration of buffers to avoid excessive acidemia. Acid–base assessment usually can be completed before initiating therapy; however, the first step should be to determine whether there are life-threatening pH disturbances (e. The pH status will usually indicate the predominant primary process, that is, acidosis produces acidemia and alkalosis produces alkalemia. Note that the suffix “-osis” indicates a primary process that, if unopposed, will produce the corresponding pH change. The third step is to determine whether the entire arterial blood gas picture is consistent with a simple acute respiratory alkalosis or acidosis (Table 16-6). If neither an acute nor chronic respiratory change appears to explain the arterial blood gas data, then a metabolic disturbance must also be present. Table 16-7 Sequential Approach to Acid–Base Interpretation The fifth question addresses respiratory compensation for metabolic disturbances, which occurs more rapidly than renal compensation for respiratory disturbances (Table 16-3). Second, inadequate or excessive compensation suggests an additional primary disturbance. Third, hypobicarbonatemia associated with an increased anion gap is never compensatory. The sixth question, whether an anion gap is present, should be assessed even if the arterial blood gases appear straightforward. As noted previously, correct assessment of the anion gap requires correction for hypoalbuminemia. For instance, if metabolic acidosis results from administration of large volumes of 0. The seventh and final question is whether the clinical data are consistent with the proposed acid–base interpretation. Failure to integrate clinical findings with arterial blood gas and plasma electrolyte data may lead to serious errors in interpretation and management. Example 1 A 65-year-old woman has undergone 12 hours of an expected 16-hour radical neck dissection and flap construction. Patients under general anesthesia with controlled mechanical ventilation cannot compensate for metabolic acidosis. However, spontaneous hypocarbia of this magnitude would represent slight overcompensation for metabolic acidosis (Table 16-3) and would suggest the presence of a primary respiratory alkalosis. Metabolic acidosis occurring during prolonged anesthesia and surgery could suggest lactic acidosis and prompt additional fluid therapy or other attempts to improve perfusion. The arterial blood gases and serum electrolytes are compatible with the clinical picture. An arterial blood gas reveals the results shown in the third column of Table 16-9. The limits of respiratory compensation for metabolic alkalosis are wide and difficult to predict for individual patients. The diagnosis of a primary metabolic alkalosis with compensatory hypoventilation is consistent with the history of recurrent vomiting. Consider how the arterial blood gases could change if vomiting were sufficiently severe to produce hypovolemic shock and lactic acidosis (fourth column of Table 16-9). Complex or “triple disturbances” can only be interpreted using a thorough, stepwise approach. Fluid Management Physiology Body Fluid Compartments Accurate replacement of fluid deficits necessitates an understanding of the expected volumes of distribution spaces for water, sodium, and colloid. The predominant intracellular cation, potassium, has an intracellular concentration ([K ]) approximating 150 mEq/L. As an example of the static approach, assume that a 70-kg patient has suffered an acute blood loss of 2,000 mL, approximately 40% of the predicted 5 L blood volume. Kinetic21 models of intravenous fluid therapy allow clinicians to predict more accurately the time course of volume changes produced by infusions of fluids of various compositions. Kinetic analysis permits estimation of peak volume expansion and rates of clearance of infused fluid and complements analysis of “pharmacodynamic” effects, such as changes in cardiac output or cardiac filling pressures. For example, in chronically instrumented sheep, fluid infusion during isoflurane anesthesia was associated with greater expansion of extravascular volume than in the conscious state. Similar studies23 1012 in volunteers suggested that the influence of anesthesia on fluid kinetics could be related to lower mean arterial pressures and activation of the renin/angiotensin/aldosterone system. In subsequent studies in sheep,24 administration of catecholamine infusions before and during fluid infusions profoundly altered intravascular fluid retention, with phenylephrine diminishing and isoproterenol enhancing intravascular fluid retention (Fig. Rapid infusion of crystalloid fluids can potentially release noncirculating fluid volume that is trapped within the endothelial glycocalyx, resulting in26 apparent rather than actual plasma dilution. Water intake includes ingested liquids plus an average of 750 mL ingested in solid food and 350 mL that is generated metabolically. Thirst, the primary mechanism of controlling water intake, is triggered by an increase in body fluid tonicity or by a decrease in effective circulating volume. Catecholamine protocols are dopamine (Dopa, open diamonds), isoproterenol (Iso, closed circles), phenylephrine (Phen, open triangles), and no-drug control (Control, closed squares). Effects of different catecholamines on the dynamics of volume expansion of crystalloid infusion. Renal water handling has three important components:27 (1) delivery of tubular fluid to the diluting segments of the nephron, (2) 1014 separation of solute and water in the diluting segment, and (3) variable reabsorption of water in the collecting ducts. In the descending loop of Henle, water is reabsorbed while solute is retained to achieve a final osmolality of tubular fluid of approximately 1,200 mOsm/kg (Fig. In this pathway, decreased stretch in the baroreceptors of the aortic arch and carotid body and stretch receptors in the great veins, pulmonary vasculature, and atria result in increased sympathetic tone. Increased sympathetic tone, in combination with decreased renal perfusion, leads to renin release and formation of angiotensin I from angiotensinogen. Fluid Replacement Therapy Maintenance Requirements for Water, Sodium, and Potassium Calculation of maintenance fluid requirements is of limited value in determining intraoperative fluid requirements. However, calculation of maintenance fluid requirements (Table 16-10) is useful for estimating water and electrolyte deficits that result from preoperative restriction of oral food and fluids and for estimating the ongoing requirements for patients with prolonged postoperative bowel dysfunction. In healthy adults, sufficient water is required to balance gastrointestinal losses (100 to 200 mL/day), insensible losses (500 to 1,000 mL/day), and urinary losses of 1,000 mL/day. In the descending loop of Henle (2), water is absorbed to achieve osmotic equilibrium with the interstitium while electrolytes are retained. The numbers (300, 600, 900, and 1,200) between the descending and ascending limbs represent the osmolality of the interstitium in milliosmoles per kilogram.
Syndromes
However discount cefixime generic infection elite cme, metabolic factors are the primary physiologic determinants of coronary vascular tone and myocardial perfusion buy cefixime 200mg bacteria from water. The ratio of subepicardial to subendocardial blood flow remains near unity throughout the cardiac cycle despite the differentially greater systolic compressive forces exerted on the subendocardium cefixime 100 mg lowest price antibiotics for sinus infection and uti. The relative maintenance of subendocardial blood flow despite compression is also related to the redundancy of arteriolar and capillary anastomoses within the subendocardium. The heart normally extracts between 75% and 80% of arterial oxygen content, by far the greatest oxygen extraction of all the body’s organs. Heart rate is the primary determinant of myocardial oxygen consumption in the intact heart. Increases in myocardial contractility, preload, and afterload are also associated with greater myocardial oxygen consumption. Cardiac oxygen extraction is near maximal under resting conditions and cannot substantially increase during exercise. As a result, the primary mechanism by which myocardium is able to meets its oxygen requirements during exercise is through enhanced oxygen delivery, which is proportional to coronary blood flow when hemoglobin concentration is constant. Thus, it is not surprising that myocardial oxygen consumption is the most important determinant of coronary blood flow. For example, myocardial oxygen consumption and corresponding coronary blood flow increase by a magnitude of four- to fivefold during strenuous physical exercise. The difference between maximal and resting coronary blood flow (coronary reserve) determines the magnitude with which coronary blood flow can rise during exercise-induced increases in myocardial oxygen consumption. Coronary vascular resistance is greater in the resting, perfused heart than in the contracting heart. These data suggest that increases in coronary blood flow exceed those of perfusion pressure in response to greater myocardial oxygen consumption when the heart is contracting versus when it is quiescent. The precise mechanisms responsible for this close correlation between myocardial oxygen consumption and coronary vasomotor tone remain elusive. The factors responsible for coronary autoregulation (maintenance of coronary blood flow despite changes in perfusion pressure) and reactive hyperemia (the several-fold increase in coronary blood flow 753 above baseline after a brief period of myocardial ischemia) are also not clearly understood. Metabolic coronary vasodilation in response to enhanced myocardial oxygen consumption during exercise occurs, at least in part, as a result of enhanced local release of metabolic substrates (e. This latter effect causes a “feed-forward” vasodilation of small coronary arterioles by activating β adrenoceptors. An α adrenoceptor-13 induced vasoconstriction also occurs in larger coronary arteries during exercise. Although seemingly counterintuitive, this differential vasoconstriction of larger caliber upstream coronary arteries serves two important functions: reduction of vascular compliance and attenuation of the wide swings in coronary blood flow normally observed during the cardiac cycle. In contrast to the important role of the cardiac sympathetic nerves, parasympathetic innervation has a relatively minor direct effect on coronary blood flow regulation despite its well-known negative inotropic and chronotropic actions. The aforementioned conclusions about sympathetic nervous system control of the coronary circulation are based on alterations in the slope of the myocardial oxygen consumption–coronary venous oxygen tension relation during graded exercise in the presence of exogenous α or β adrenoceptor blockade. The β adrenoceptor appears to account for only one-fourth of the total coronary vasodilation observed during exercise-induced hyperemia, but most of this vasodilation is most likely related to local or autocrine metabolic factors that act on coronary vascular smooth muscle with or without the additional modulation by vascular endothelium. Adenine nucleotides from red blood cells or the myocardium itself may activate endothelial purinergic receptors to produce coronary vasodilation during exercise. Many factors14 have been proposed to individually or collectively modulate coronary blood flow at the arteriolar or capillary level, including adenosine, bradykinin, nitric oxide, arterial oxygen or carbon dioxide tension, acid–base status, osmolarity, plasma electrolyte (e. For example, hypoxia or ischemia decreases arterial oxygen tension and pH concomitant with increases in carbon dioxide tension, adenosine release, and the plasma concentrations of K and Ca+ 2+. These changes collectively augment coronary blood flow during exercise, but none individually is solely responsible for this vasodilation. Adenosine receptor blockade does not alter coronary blood flow under resting conditions or during exercise. Endothelin and thromboxane A produce direct2 coronary vasoconstriction in vitro, but the precise role of these substances on the regulation of coronary blood flow in vivo has not been defined. Cardiac Myocyte Anatomy and Function Ultrastructure The heart contracts and relaxes nearly three billion times during an average lifetime, based on an average heart rate of 70 beats per minute and a life expectancy of 75 years. A review of cardiac myocyte ultrastructure provides important insights into how this remarkable feat is possible. Deep invaginations of the sarcolemma, known as transverse (T) tubules, penetrate the internal structure of the myocyte at regular intervals. The T-tubules assure rapid, simultaneous transmission of the depolarizing impulses that initiate myocyte contraction. The cardiac myocyte is densely packed with mitochondria that are responsible for production of large quantities of high-energy phosphates (e. The myofilaments within each sarcomere are arranged in parallel cross-striated bundles of thin (containing actin, tropomyosin, and the troponin complex) and thick (primarily composed of myosin and its supporting proteins) fibers. Sarcomeres are connected in 755 series and produce characteristic shortening and thickening of the long and short axes of each myocyte, respectively, during contraction. Observations from light and electron microscopy led to the definition of the sarcomere’s distinctive structural features. The “I” band represents the region of the sarcomere that contains thin filaments alone, and this band is reduced in width as the cell contracts. Each “I” band is bisected by a “Z” (from the German zuckung [twitch]) line, which delineates the border between two adjacent sarcomeres. As a result, the length of each sarcomere contains a complete “A” band and two symmetric one-half “I” bands located between “Z” lines. This “M” band is composed of thick filaments spatially constrained in a cross-sectional hexagonal matrix by myosin-binding protein C. The contractile machinery and the mitochondria that power it occupy more than 80% of the total volume of the cardiac myocyte. This observation emphasizes that mechanical function, and not new protein synthesis, is the predominant activity of the cardiac myocyte. Intercalated discs connect adjacent myocytes through the fascia adherens and desmosomes that link actin and other proteins between cells, respectively. The intercalated discs also provide a seamless electrical connection between myocytes via large, nonspecific ion channels (known as “gap junctions”) that facilitate intercellular cytosolic diffusion of ions and small molecules. Contractile Apparatus Myosin, actin, tropomyosin, and the three-protein troponin complex compose the six major components of the contractile apparatus. Enzymatic digestion of myosin divides the structure into light (containing the tail section of the complex) and heavy (composed of the globular heads and the light chains) meromyosin. The elongated tail section of the myosin complex (light meromyosin) functions as the main structural 756 support of the molecule (Fig. The globular heads of the myosin dimer contain two “hinges,” located at the junction of the distal light chains and the tail helix, that play an essential role in myofilament shortening during contraction. The myosin molecules are primarily arranged in series along the length of the thick filament, but are abutted “tail-to-tail” in the center of the thick filament. This orientation facilitates shortening of the distance between “Z” lines during contraction as the thin filaments are drawn symmetrically toward the sarcomere’s center. Figure 12-6 Schematic illustration of the myosin molecule demonstrating double helix tail, globular heads that form cross bridges with actin during contraction, two pairs of light chains, and “hinges” (cleavage sites of proteolytic enzymes) that divide the molecule into meromyosin fragments (see text).
Order genuine cefixime on line. BEST TEAS FOR ACNE.