
Dakota State University. C. Carlos, MD: "Buy Indocin online - Discount online Indocin".
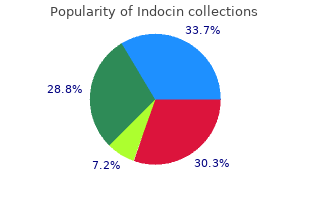
Commercially available kits for genotyping have made it possible to obtain results within 48–72 h order indocin 75mg line arthritis knee replacement surgery, thereby making this method more appealing for use in diagnostic molecular laboratories generic 75 mg indocin with mastercard arthritis in back of ankle. Direct sequencing generic 75mg indocin arthritis in the back ribs, along with deep sequencing (full genome sequenc- ing), is commonly used as the gold standard comparator methods for the identification of viruses or bacteria that do not grow well using culture techniques. Direct sequencing for ampli fi cation product detection and identification will be discussed in detail in Chap. Pyrosequencing Pyrosequencing is a totally different approach to sequencing compared to other chain termination method. Along with this template, the reaction mix also includes a sequencing primer, sulfurylase and 362 C. The generation of light indicates which nucleotide solution complements the first unpaired base of the template. In turn, the sequence of solutions which produced chemiluminescence determines the sequence of the template. However, this method is limited to short sequence analysis (about 300–500 nucleotides) and is mostly used for mutation detection and infectious disease typing like in determin- ing Hepatitis C virus genotypes [24], rather than for generating new sequences. It is also sometimes supplied with software for identifying the spots on the array by the array reader. Microarray technology has been used for over a decade in gene expression studies and is now gaining popularity in microbial identification and detection. Today, several commercial products that incorporate microarrays as the identification method are available in the market for the detection of a panel of respiratory viral pathogens [28–30]. This strategy allows multi- plex analysis and simultaneous identification of a broad range of microorganisms in a given sample. Multiple pairs of broad-range primers are used to amplify highly conserved regions of bacterial, viral, or fungal genomes. Using the masses of the base compositions of ampli- cons from all the primer pairs, the organisms present in the sample can be identified and quantified. However, even with the promise of faster turnaround time and accurate pathogen identification, it is not certain how these instruments will perform under diagnostic laboratory conditions. Persing D, Tenover F, Tang Y-W, Nolte F, Hayden R, van Belkum A (eds) (2011) Molecular microbiology: diagnostic principles and practice, 2nd edn. Buckingham LaF M (ed) (2007) Molecular diagnostics: fundamentals, methods, and clinical applications, 1st edn. Sambrook J, MacCullum P (eds) (2005) Molecular cloning: a laboratory manual, 3rd edn. Mallet F, Hebrard C, Brand D et al (1993) Enzyme-linked oligosorbent assay for detection of polymerase chain reaction-amplified human immunodeficiency virus type 1. Poljak M, Seme K (1996) Rapid detection and typing of human papillomaviruses by consensus polymerase chain reaction and enzyme-linked immunosorbent assay. Elahi E, Pourmand N, Chaung R et al (2003) Determination of hepatitis C virus genotype by pyrosequencing. Brunstein J, Thomas E (2006) Direct screening of clinical specimens for multiple respiratory pathogens using the Genaco Respiratory Panels 1 and 2. J Clin Virol 40(Suppl 1):S39–S46 20 An Introduction to Ampli fi cation–Production–Detection Techniques 365 31. J Clin Microbiol 49:908–917 Chapter 21 Gel Electrophoresis, Southern Blot, and Colorimetric Microwell Plate-Based System Jie He, Michael J. Loeffelholz , and Jiang Fan Introduction Infectious disease-related illnesses are a significant threat to human health resulting in substantial morbidity and mortality, worldwide. Timely and accurate diagnostic tools are critical for patient treatment decisions and disease outcomes. Molecular diagnostics are revolutionizing the clinical practice of infectious disease. The vari- ous formats of nucleic acid amplification are the most frequently used molecular tests in the diagnosis of infectious diseases due to its exquisite sensitivity and specificity. Gel electrophoresis and Southern hybridization are two basic technolo- gies that are used to display the specific amplification of targeted gene and are still used in the laboratories for diagnosis because it is such a powerful technique, and yet reasonably easy and inexpensive. Due to significant advances in technology, the conventional gel electrophoresis and Southern hybridization are not mainstream methods in molecular diagnostic laboratories anymore. Instead, continued refinements in electrophoresis technology, such as improvements in automation and throughput have allowed this technology to be increasingly adapted and integrated into various currently used state of the art molecular technologies used in clinical and research laboratories for rapid, highly sensitive and specific and quantitative pathogen detection [1–9 ]. Loeffelholz Department of Pathology , University of Texas Medical Branch , 301 University Blvd. Therefore, the gel electrophoresis and nucleic acid hybridization are the two basic technologies that are being used in most presently available advanced molecu- lar diagnostic assays and systems. In addition, some complex electrophoresis meth- ods, such as 2-D gel systems, have well developed and widely used in analyzing complex pathogenesis to get plenty of information and make molecular diagnosis even more powerful for clinicians providing better treatment and prevention. Thus, this section provides an up-to-date look at the general principles, diagnostic value, and the advances in development of the gel electrophoresis and Southern hybridiza- tion technology. The Principles and Application of Gel Electrophoresis Electrophoresis is a technique used to separate charged molecules in a gel matrix. Agarose is a polysaccharide consisting mainly of long chain of galactopyranose residues. Dissolved agarose can polymerize into a semisolid matrix by cross-linking the sugar polymers with each other to form the gel matrix. Polyacrylamide gels are formed from the polymerization of two compounds, acrylamide and N,N -methylene- bis-acrylamide. The polyacrylamide gels are neutral, hydrophillic, 3-D networks of long hydrocarbons cross-linked by methylene groups. The separation of molecules within an agarose or polyacrylamide gel is determined by the relative size of the pores formed within the gel. For agarose gel, the pore size of a gel is determined by the concentration of agarose. The pore size of a polyacrylamide gel is determined by two factors, the total amount of acrylamide present (designated as %T) and the amount of cross-linker (%C). The total acrylamide is given as a % (w/v) of the acrylamide plus the bis-acrylamide. In spite of the many physical arrangements for the apparatus, electrophoretic separations depend upon the charge distribution of the molecules being separated. Therefore, all of the proteins can migrate toward the anode when separated on a polyacrylamide gel. The traditional electrophoresis process is time-consuming that do not fit the requirement of rapid molecular diagnosis. In addition, the size information of amplicons that gel electrophoresis acquired is not specific enough to determine etiological pathogen.
Syndromes
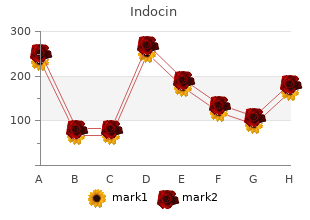
This distinction requires not only a difference in administration purchase discount indocin brauer arthritis relief cream, but also a difference in vigilance with respect to opioid side effects buy 25 mg indocin free shipping equine arthritis in back. During anesthesia one should be aware of hypotension and 1322 bradycardia order indocin 25 mg otc arthritis feet massage, a common side effect of strong opioids. In contrast, in the postoperative period the most important side effects to avoid are respiratory depression and severe sedation, while other non–life-threatening side effects impacting patient satisfaction and health costs are nausea/vomiting and loss of bowel motility. Morphine In two studies on the postoperative effects of morphine following major surgery, the average intravenous dose of morphine to reach 50% pain relief was 20 mg. This dose resulted in a plasma concentration of 34 ng/mL and a t½k of about 2 hours, although the initial onset of analgesia occurrede0 between 15 and 30 minutes. Surprisingly, these parameters are not influenced by the patient’s age, weight, and gender. Given the long time to peak analgesia, a practical strategy for dosing morphine in adults is to give an initial morphine bolus dose (0. Figure 20-7 Simulated effect of multiple bolus doses of fentanyl (100 to 150 μg) during anesthesia, and morphine during and following anesthesia, on the analgesic and 1323 hemodynamic state of the patient. The blue and red lines are the simulated fentanyl and morphine plasma concentration (Cp). During anesthesia, the combination of fentanyl and propofol (orange line) provides greater analgesia than opioids alone (green line). When propofol infusion is terminated the analgesic profile reverts to a lower level (from orange via orange-green to green line). The dotted lines are the arbitrary divisions between adequate anesthesia and inadequate anesthesia, and adequate analgesia and inadequate analgesia. First, the postoperative analgesic regimen should be multimodal with morphine (or any other opioid), and combined with opioid-sparing drugs such as acetaminophen and nonsteroidal anti-inflammatory drugs such as diclofenac. Second, some patients require large doses of morphine, yet their pain appears unresponsive to morphine. Both drugs are analgesics in their own right and enhance morphine’s analgesic effect. Like all opioids the analgesic response to intravenous fentanyl is highly variable. However, fentanyl’s t½k for analgesic effect is longer with valuese0 ranging between 10 and 20 minutes ; fentanyl’s potency (66 C ) for analgesia 50 ranges from 1 to 2 ng/mL. Fentanyl is used during anesthesia to dampen66 cardiovascular responses to noxious stimulation from laryngoscopy, intubation, skin incision, and surgical stress. On average, the requirements for inhalational anesthetics and propofol are reduced by about 50% when 1324 administering 1. Be aware that a continuous infusion leads to the accumulation of the drug in the body as its 50% context-sensitive half-time increases rapidly with the duration of infusion (Fig. Taking into account the drug’s t½k fentanyl shoulde0 be administered 5 to 10 minutes prior to an anticipated painful/stressful event such as laryngoscopy or skin incision (Fig. In the 1980s, high-dose fentanyl was often used in combination with nitrous oxide to provide both analgesia and suppression of consciousness. Although this combination provided excellent hemodynamic stability, it could not assure amnesia. For example, the fentanyl patch is used in a large number of cancer and noncancer chronic pain patients. The transcutaneous delivery of fentanyl ranges from 12 to 100 μg/hr, although absorption depends on a variety of factors such as skin thickness, subcutaneous fat layer, and subcutaneous perfusion. Peak analgesic effect is reached only after 10 to 12 hours and the effect of one patch lasts 3 to 4 days. Other methods of administration include intranasal fentanyl, sublingual fentanyl, fentanyl lozenges (a solid preparation in the form of a lollipop), mucosal patch—all four methods are used for treatment of breakthrough pain—and iontophoretic transdermal fentanyl applications. The home use of fentanyl in chronic pain patients comes with the danger of misuse and abuse by the patients or by family members or friends. Sufentanil Sufentanil is a thienyl derivate of fentanyl and about 10 times more potent than fentanyl; its lipophilicity is two times greater than that of fentanyl. Sufentanil is metabolized in the liver toe0 various inactive and one active compound, desmethylsufentanil. The latter has 10% of the activity of sufentanil, and since it is produced in minute quantities has no clinical relevance. Sufentanil is used predominantly as an analgesic 1325 during anesthesia, as it produces stable hemodynamics and cardiac output. The use of remifentanil in spontaneous breathing patients at relatively low infusion rates (<0. Top: The measured remifentanil plasma concentration (blue dots) and the pharmacokinetic data fit (blue line). Modeling the non-steady-state respiratory effects of remifentanil in awake and propofol sedated healthy volunteers. Like other 1326 opioids, remifentanil displays large variability in effect among patients. This difference can be accounted for by the difference in surgical stimulation of the prostatectomies versus hysterectomies. Like fentanyl, remifentanil causes a reduction in both volatile anesthetic and propofol requirements. When added to a constant propofol plasma concentration of 2 μg/mL, the remifentanil concentration required for suppression of hemodynamic and movement responses during abdominal surgery varies from 3 to 15 ng/mL. Interestingly, at a higher propofol concentration of 4 μg/mL, the variability was reduced to 0 to 5 ng/mL. These data reinforce that opioid dosing requires titration to effect based on careful observation of the clinical response of the patient. Between intubation and surgical incision, when there is no stimulation, decreases of 30% to 40% in blood pressure and heart rate are not uncommon unless the remifentanil infusion dose is reduced during that period. For example, after a 3-hour infusion of82 propofol and remifentanil for abdominal surgery, the shortest time to awakening (≈7 minutes) was observed after constant propofol and remifentanil concentrations of 2. The occurrence of postoperative pain following remifentanil “fast-track” anesthesia is frequently reported. Strategies to counteract this problem include starting morphine administration 30 to 45 minutes before the end of surgery, or a single fentanyl bolus of 50 μg or ketamine 0. Remifentanil–propofol interaction causing 50% probability of no response to surgical stimulation are given at t = 0 minutes. Next the infusion pumps are switched off causing the decreasing effect site concentrations. The bold line on top of the 3D surface represents the 50% probability of return of consciousness. The lowest point represents the optimal propofol–remifentanil concentration during surgery that gives the minimal recovery time after the pumps are switched off. Some83 examples of pharmacogenetic variations that influence opioid analgesia are given below. Animal and human studies indicate that specific mutations in this gene cause a phenotype of red hair, a fair, freckled skin, and an increase in μ-opioid analgesia (Fig.
The dosages of the neurolytic agents are 30 to 40 mL for the retrocrural and anterocrural approach purchase indocin with a visa arthritis diet rhubarb, and 10 to 15 mL on each side for splanchnic nerve blockade buy indocin 75 mg without prescription arthritis in my fingers and toes. Complications from the celiac plexus block include orthostatic hypotension purchase 25 mg indocin arthritis uveitis, back pain, retroperitoneal hematoma, reactive pleurisy, hiccups, hematuria, transient diarrhea, abdominal aortic dissection, transient motor paralysis, and paraplegia. The paraplegia and transient motor paralysis may be due to spasm of the lumbar segmental arteries that perfuse the spinal cord, direct vascular or neurologic injury, or retrograde spread to the nerve roots or spinal cord. Note that the tip of the needle is in the upper third of L1 and about 1 cm beyond the border of the vertebral body for the retrocrural technique; the spread of the contrast medium is cephalad. In contrast, the tip of the needle is the lower third of L1 and about 3 cm beyond the border of the vertebral body for the anterocrural technique; the spread of the contrast medium is caudad and in front of the aorta. A meta-analysis of 21 retrospective studies in 1,145 patients concluded that adequate-to-excellent pain relief was achieved in 89% of the patients during the first 2 weeks following the block and partial-to-complete pain relief continued in 90% of the patients at the 3-month interval. The plexus is located in the retroperitoneum, bilaterally extending from the lower third of the fifth lumbar vertebra to the upper third of the first sacral vertebra. For blockade of the plexus, the patient is placed in the prone position and two 7-cm needles are inserted, under fluoroscopy, in medial and caudal directions until the tips lie anterior to the L5 to S1 intervertebral disc space. After injection of contrast medium, 6 to 8 mL of local anesthetic is used for a diagnostic block while phenol or alcohol is employed for neurolysis. Anterior ultrasound-guided superior hypogastric plexus blocks appear to be effective for pelvic pain. Case reports support the efficacy of neurolytic superior hypogastric plexus block both in reducing pelvic pain secondary to cancer and in decreasing opioid consumption. Visceral afferents innervating the perineum, distal rectum, anus, distal urethra, vulva, and distal third of vagina converge at the ganglion. Four to 8 mL of local anesthetic is used for diagnostic block and 8% to 10% phenol or 50% alcohol is used for neurolysis. Similar to superior hypogastric plexus blocks, there are no controlled studies on its efficacy, although case reports confirm its effectiveness in relieving perineal pain secondary to cancer. Pharmacologic Management of Pain Opioids Morphine is the standard for opioid therapy for cancer pain (see Chapter 20, Opioids). The metabolites of morphine include morphine-6-glucuronide, which causes additional analgesia, and morphine-3-glucuronide, which can cause adverse effects. Controlled-release preparations are available, reducing the need to take the drug frequently. Hydromorphone, a μ-receptor agonist, is three to five times more potent than morphine when given orally and five to seven times more potent when given parenterally. Pruritus, sedation, nausea, and vomiting occur less frequently compared with morphine. Its metabolite, hydromorphone-3- glucoronide, lacks analgesic property but possesses properties similar to that of morphine-3-glucuronide. Methadone has a 60% to 95% bioavailability, high potency, and a long duration of action. Its potency compared with morphine ranges from 1:1 to 1:2 on acute dosing but can be 1:4 with chronic dosing. It has a long and unpredictable half-life of 8 to 80 hours that makes it difficult to achieve steady-state plasma concentrations, increasing the risk of accumulation and the need for careful and individualized dosing. There has been an “epidemic” of deaths due to 4050 unintentional overdose from methadone111 because many physicians do not appreciate the consequences of the drug’s long and unpredictable half-life. Most reports are based on high-dose maintenance (>120 mg) for the treatment of addiction; however, such occurrences have also been reported with lower dosages. It has a high bioavailability (60%) and is associated with a low incidence of itching and hallucinations. The controlled-release preparation (OxyContin, Purdue Pharma) has good analgesic characteristics but became a popular drug for abuse prior to its reformulation to include abuse-deterrent technologies. Oxymorphone has greater affinity to the μ-receptor than morphine and has little or no affinity to the κ-opioid receptor. Due to extensive first-pass hepatic metabolism, the bioavailability of oxymorphone is only 10%. It should not be taken with alcohol because this increases its plasma concentration by as much as 300%. The efficacy of oxymorphone in chronic and cancer pain is similar to other opioids. Buprenorphine is a partial agonist at the μ-receptor, a κ-antagonist, and a weak δ-agonist. It has a rapid onset (30 minutes) when given orally and a long duration of action of 6 to 9 hours. Buprenorphine antagonizes the opioid effects of full agonists such as morphine or hydromorphone due to its partial opioid agonist pharmacodynamics. Approximately 9% of Caucasians do not have the enzyme and do not experience analgesia from codeine. Children under 12 years of age lack maturity of the enzyme and cannot convert the drug to morphine, experiencing the drug’s side effects with minimal analgesia. It has bioavailability of 80% to 90%, low abuse potential, low incidence of constipation, and minimal risk of fatal respiratory depression, which is possibly limited to patients with severe renal failure. Tapentadol is similar to tramadol and also has a dual mode of action as a μ- opioid agonist and a norepinephrine reuptake inhibitor. Tapentadol has side effects and adverse reactions that are similar to those of tramadol, but has a higher risk of addiction and respiratory depression due to its opioid agonism. The oral equianalgesic doses of morphine 10 mg intravenously or 30 mg orally are (1) 200 mg of codeine, (2) 30 mg of hydrocodone, (3) 20 mg of oxycodone, (4) 150 mg of tramadol, and (5) 75 mg of tapentadol. A 2013 study determined, contrary to older studies, that individuals receiving stable doses of 20 mg of morphine or equivalent are at increased risk for motor vehicle collisions and this risk increases substantially at doses above 120 mg. Opioids are commonly used for cancer pain, with long-acting opioids supplemented by short-acting ones for breakthrough pain. Opioid monotherapy in cancer pain is rarely successful and adjuvants and procedural interventions are usually added for increased efficacy. The use of opioids for acute or short-term pain (<3 months) following surgery or traumatic injuries is well accepted and supported by the literature. The use of opioids for treatment of chronic (>3 months) noncancer pain is controversial. To date, there has been no randomized clinical trial establishing the efficacy of chronic opioid therapy for greater than 3 months. Studies show them to be effective in the treatment of neuropathic pain, although at higher doses. Because of the undesirable issues associated with the use of opioids, such as addiction, aberrant behaviors, and regulatory issues, opioids are a third-line drug for neuropathic pain.
Landmarks for location of the mandibular fossa are the same as those described for maxillary nerve blockade discount indocin 50 mg mastercard arthritis in fingers after broken wrist. The needle is then redirected posteriorly until it passes beyond the pterygoid plate buy discount indocin 75 mg on-line arthritis upper back exercises. Gentle exploration in a cephalad and caudad direction buy indocin 75mg cheap arthritis itchy back, from the initial point where the needle passes posterior to the plate, may be required. After slight needle withdrawal, 5 to 10 mL of solution is injected incrementally with repeated aspiration to avoid intravascular injection. Injection should be performed incrementally with small quantities, and there should be constant observation for signs of toxicity. During carotid surgery, local infiltration of the carotid bifurcation may be necessary to block reflex hemodynamic changes associated with glossopharyngeal stimulation. Deep Cervical Plexus Block Procedure • The patient is placed supine with a small towel under the head, which is turned 45 degrees to the opposite side with slight neck extension. If all transverse processes cannot be palpated, the most prominent tubercle of C6 (Chassaignac’s) is marked. A line is drawn from the mastoid process along the sternocleidomastoid muscle to reach the transverse process of C6. Two to three milliliters of local anesthetic solution are injected per segment for therapeutic or diagnostic purposes or for blocks in children, whereas 5 to 10 mL per segment may be sufficient for surgical block (limiting the total to approximately 20 mL if superficial blocks are also performed). Clinical Pearls • The deep block may be performed by single injection at C3 or C4 as originally described by Winnie et al. With94 2393 this approach, both the deep cervical plexus and sympathetic trunk can be blocked. Injection may occur into the vertebral artery, and subarachnoid or epidural injections are possible if the needle is advanced too far medially into the vertebral foramen. This is more likely in the cervical region because of the longer dural sleeves that accompany these nerve branches. Careful monitoring of the patient should continue for 60 minutes after the block has been performed. This block is not98 indicated in any patient who depends on the diaphragm for tidal ventilation, nor is bilateral blockade ever recommended. Superficial Cervical Plexus Block This block is performed in a position similar to deep cervical plexus block and results in anesthesia only of the sensory fibers of the plexus. Procedure • An “X” is made at the midpoint of the posterior border of the sternocleidomastoid muscle. Clinical Pearls • The most common approach for minimally invasive parathyroidectomy (involving a small unilateral incision rather than bilateral neck exploration) includes a combination of C2–C4 superficial cervical 2394 plexus block, infiltration along the incision line and infiltration of the upper thyroid pedicle. Figure 36-18 Lateral view of the head and neck, showing block needle insertion angles needed to perform superficial cervical plexus block. Initially, the needle is inserted perpendicular to the skin at the midpoint of the lateral border of the sternocleidomastoid muscle (where it is crossed by the external jugular vein). The needle can then be repositioned to superior and inferior angulations to reach the entire cervical plexus. Occipital Nerve Blocks 2395 The greater and lesser occipital nerves can be blocked by superficial injection at the points on the posterior skull where they emerge from below the muscles of the neck. This block is rarely used for surgical procedures and is more often applied as a diagnostic step in evaluating head and neck pain complaints. Procedure • The patient sits with their head tilted forward slightly to expose the prominent nuchal ridge of bone at the posterior base of the skull. A mark is placed on the nuchal line at the lateral border of the insertion of the erector muscles of the neck, usually 2. At this point, the branches of the greater occipital nerve usually pass laterally from behind the muscle to cross the nuchal line. During its ascent along the posterior skull, the lesser occipital nerve can be located an additional 2. Paresthesias are occasionally encountered but are not essential for obtaining simple skin anesthesia. A band of anesthetic solution is deposited along the line between skin entry and the mastoid process using 2 to 3 mL of local anesthetic. Clinical Pearls • Blockade of the lesser occipital and great auricular nerves (both blocked by subcutaneous injection from the angle of the mandible to the mastoid process) has been successful in providing postoperative analgesia after otoplasty. For chronic syndromes, the anterior region involving the trigeminal nerve is also blocked. Care must be taken not to advance the needle anteriorly under the skull, as the foramen magnum might be entered unintentionally with a long needle. Local hematoma may be produced with superficial injection, but this is only a temporary problem. Upper Extremity Although many approaches to the brachial plexus have been described, there are traditionally four anatomic locations where local anesthetics are placed: (1) the interscalene groove near the cervical transverse processes, (2) the subclavian sheath at the first rib, (3) near the coracoid process in the infraclavicular fossa, and (4) surrounding the axillary artery in the axilla. It is important to stress that clear visibility of the needle is essential for this block (and generally for all blocks of the brachial plexus). The appropriate choice of approach depends not only on the patient’s anatomy but also on the site of surgery and the method used to locate nerve structures. The terminal branches of the brachial plexus can also be anesthetized by local anesthetic injection along their peripheral course as they cross joint spaces, where they lie proximal to easily identifiable structures (Table 36-1), or by injection of a dilute local anesthetic solution intravenously below a pneumatic tourniquet on the upper arm (“intravenous regional” or Bier block). For example, the ulnar nerve can be blocked effectively at the medial surface of the mid-forearm, which may reduce the risk of ulnar nerve palsy posed by block at the elbow near the cubital tunnel. Brachial Plexus Block Interscalene Block This block, as described by Winnie111 in 1970, is indicated mostly for surgical anesthesia of the shoulder, upper arm, and forearm but is often insufficient 2397 for the hand. Frequently, it spares the lowest branches of the plexus, the C8 and T1 fibers, which innervate the caudad (ulnar) border of the forearm. Nevertheless, recent reports provide evidence that a low interscalene block (below C6, just superior to the clavicle) may provide sufficient anesthesia and analgesia for procedures on the lower arm. The main surface landmark used for this block—the sternocleidomastoid muscle—can be accentuated by asking the patient to reach for the ipsilateral knee and by rotating the head approximately 45 degrees to the nonoperative side. The head should also be elevated slightly, and the patient should be instructed to take a deep breath since contraction of the scalenus muscles accentuates the interscalene groove. This groove lies immediately behind the lateral border of the clavicular head of the sternocleidomastoid muscle at the level of the cricoid cartilage (C6). Procedure Using Nerve Stimulation Technique • Landmarks: Using the maneuvers described earlier, the interscalene groove is palpated by rolling the fingers posteriorly off the lateral border of the sternocleidomastoid muscle; mark the groove as high as possible. After the patient relaxes, the prominent transverse process of C6 can often be felt directly in the groove and should be marked. A 22-gauge, 36- to 50-mm insulated needle (shorter for pediatric patients) is introduced through the wheal.
Order indocin 75mg line. Carnivore Diet: A Cure for Depression and Rheumatoid Arthritis?.