
Hanover College. H. Nasib, MD: "Purchase Atrovent no RX - Cheap online Atrovent no RX".
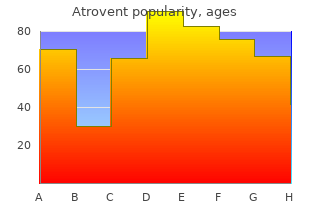
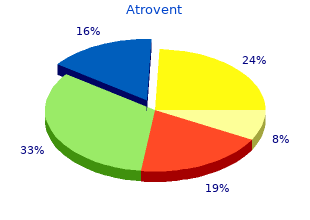
It is preferred over codeine in most situations where cough suppression is needed atrovent 20mcg with mastercard treatment ulcerative colitis. Oxymorphone given parenterally is approximately ten times more potent than morphine buy atrovent 20 mcg low price symptoms 5th disease, but when administered orally discount atrovent american express medications ending in zole, the potency drops to about three times that of morphine. Oxymorphone is available in both immediate-release and extended-release oral formulations. Oxycodone is approximately two times more potent than morphine and is available in an immediate-release formulation, alone or in combination with acetaminophen, aspirin, or ibuprofen. It is preferred over morphine in patients with renal dysfunction due to less accumulation of active metabolites. Hydrocodone is the methyl ether derivative of hydromorphone, but is a weaker analgesic than hydromorphone, with oral analgesic efficacy comparable to that of morphine. This agent is often combined with acetaminophen or ibuprofen to treat moderate to severe pain. Fentanyl has 100-fold the analgesic potency of morphine and is used for anesthesia and acute pain management. The drug is highly lipophilic and has a rapid onset and short duration of action (15 to 30 minutes). Fentanyl is combined with local anesthetics to provide epidural analgesia for labor and postoperative pain. Many fast-acting transmucosal and nasal fentanyl products are available for cancer-related breakthrough pain in opioid-tolerant patients. The transdermal patch creates a reservoir of the drug in the skin and has a delayed onset of at least 12 hours and a prolonged offset. It is contraindicated in opioid-naïve patients and should not be used in management of acute or postoperative pain. Sufentanil and carfentanil are even more potent than fentanyl, whereas the other two are less potent and shorter acting. Sufentanil, alfentanil, and remifentanil are mainly used for their analgesic and sedative properties during surgical procedures requiring anesthesia. The drug is not used in clinical practice; however, it is of toxicological interest as it is used to lace heroin and has contributed to several opioid-related deaths. Therefore, it is useful in the treatment of both nociceptive and neuropathic pain. Methadone may also be used for opioid withdrawal and maintenance therapy in the setting of prescription opioid and heroin abuse. The withdrawal syndrome with methadone is milder but more protracted (days to weeks) than that with other opioids. Methadone induces less euphoria and has a longer duration of action than morphine. Understanding the pharmacokinetics of methadone is important to ensure proper use. After oral administration, methadone is biotransformed in the liver and excreted almost exclusively in the feces. Methadone is very lipophilic, rapidly distributed throughout the body, and released slowly during redistribution and elimination. This translates into a long half-life ranging from 12 to 40 hours, although it may extend up to 150 hours. Despite the extended half- life, the actual duration of analgesia ranges from 4 to 8 hours. Attainment of steady state can vary dramatically, ranging from 35 hours to 2 weeks, so dosage adjustments should occur only every 5 to 7 days. Upon repeated dosing, methadone can accumulate due to the long terminal half-life, leading to toxicity. Overdose is possible when prescribers are unaware of the long half-life, the incomplete cross-tolerance between methadone and other opioids, and the titration guidelines to avoid toxic accumulation. Methadone can produce physical dependence like that of morphine, but it has less neurotoxicity than morphine due to lack of active metabolites. It is used for acute pain and acts primarily as a κ agonist, with some μ agonist activity. Meperidine is very lipophilic and has anticholinergic effects, resulting in an increased incidence of delirium compared with other opioids. Meperidine has an active metabolite (normeperidine), which is potentially neurotoxic. Normeperidine is renally excreted, and in patients with renal insufficiency, accumulation of the metabolite may lead to delirium, hyperreflexia, myoclonus, and seizures. Due to the short duration of action and the potential for toxicity, meperidine should only be used for short-term (≤48 hours) management of pain. Partial Agonists and Mixed Agonist–Antagonists Partial agonists bind to the opioid receptor, but they have less intrinsic activity than full agonists (see Chapter 2). Drugs that stimulate one receptor but block another are termed mixed agonist–antagonists. In individuals who are opioid-naïve, mixed agonist–antagonists show agonist activity and are used to relieve pain. In the presence of a full agonist, the agonist–antagonist drugs may precipitate opioid withdrawal symptoms. Buprenorphine is very lipophilic and has a longer duration of action due to its high affinity for the opioid receptors when compared to morphine. Due to high affinity for the mu receptor, buprenorphine can displace full μ agonists, leading to withdrawal symptoms in an opioid-dependent patient. Because of the partial μ agonist activity, buprenorphine provides a “ceiling effect,” causing less euphoric effects and a lower abuse potential than that of full agonists. Buprenorphine is available in sublingual, transmucosal, buccal, parenteral, subdermal, and transdermal formulations. Certain formulations (for example, sublingual and subdermal) are approved for use in medication-assisted treatment of opioid addiction due to its ability to provide prolonged suppression of opioid withdrawal, the ability to block other μ agonists, and less frequent dosing requirements. In contrast to methadone, which is available only at specialized clinics when used for opioid detoxification or maintenance, buprenorphine is approved for office-based treatment of opioid dependence. It has been shown to have shorter and less severe withdrawal symptoms compared to methadone (ure 14. Adverse effects include respiratory depression that cannot easily be reversed by naloxone and decreased (or, rarely, increased) blood pressure, nausea, and dizziness. Risk factors to evaluate when consideringc buprenorphine include cardiovascular factors and concurrent drugs that may prolong. Pentazocine produces less euphoria compared to morphine, but in higher doses, respiratory depression, increased blood pressure, tachycardia, and hallucinations can occur.
Diseases
The shunt should be clamped until cardiopulmonary bypass is discontinued generic 20 mcg atrovent amex symptoms 7, at which point the shunt is opened order atrovent with visa medications ordered po are. Vigorous hyperventilation may be required in the early postbypass period because pulmonary vascular resistance is often elevated during this time generic atrovent 20 mcg on line treatment of chlamydia. The ultimate goal is to achieve a circulation in which the systemic venous return is delivered directly to the pulmonary arteries, and the single ventricle is used for systemic blood flow. The original Fontan operation utilized an atriopulmonary connection for patients with tricuspid atresia. Since then, the procedure and its indications have evolved, allowing for a Fontan circulation in many single-ventricle patients. Obstruction to systemic flow may lead to inadequate systemic perfusion and a low cardiac output state. The flow of blood through a patent ductus arteriosus bypasses the obstruction in either the pulmonary or systemic circulation, maintaining a clinically stable state. However, as the pulmonary vascular resistance diminishes over the first several weeks of life, pulmonary blood flow increases and congestive heart failure develops. If pulmonary venous obstruction is present, the patient may be cyanotic owing to increased pulmonary vascular resistance. Management of the neonate with a single ventricle is directed at achieving adequate systemic oxygenation while preventing the development of pulmonary vascular disease. Surgical intervention may be required to achieve unimpeded outflow from the single ventricle into the systemic circulation. These hemodynamic parameters allow the patient to become a candidate for a subsequent Fontan procedure. Surgical Management Infants younger than 3 months with inadequate pulmonary blood flow require a systemic-pulmonary artery shunt (see Chapter 18). Infants with excessive pulmonary blood flow with no obstruction to systemic outflow require early intervention aimed at reducing the volume load on the systemic ventricle and reducing pulmonary blood flow to prevent pulmonary vascular disease. However, pulmonary artery banding may not limit pulmonary blood flow sufficiently or may result in distortion of the right or both pulmonary arteries. Therefore, many surgeons believe that division and oversewing of the proximal main pulmonary artery with construction of a systemic-pulmonary shunt is the best palliation in these cases. Patients who have both excessive pulmonary blood flow and obstruction to systemic outflow are best treated with a combined Damus-Kaye-Stansel procedure and a shunt (see Chapter 30). Management after the Neonatal Period the goal in these patients is to minimize both the pressure and volume load on the single ventricle as soon as possible. If signs or symptoms of ventricular dysfunction, atrioventricular valve problems, or increased pulmonary vascular resistance are noted, the study should be performed earlier. Therefore, during cardiac catheterization, a search for collateral vessels should be made, and, if present, they should be occluded with coils. Any aortic arch or subaortic obstruction that has not been dealt with previously must be corrected before proceeding with any other surgical interventions. Subaortic obstruction may require a Damus-Kay-Stansel procedure (see Chapter 30) or enlargement of the bulboventricular foramen. Aortic arch obstruction or discrete coarctation may respond to balloon angioplasty or may require surgical intervention (see Chapters 15 and 29). This is true whether the pulmonary blood flow is provided through a systemic-pulmonary artery shunt, or through controlled forward flow from the single ventricle, as is seen with pulmonic stenosis or following a pulmonary artery banding procedure. A superior cavopulmonary connection removes some of the volume load from the ventricle because all pulmonary blood flow is directly from the superior vena cava. This procedure can be performed successfully once the elevated pulmonary vascular resistance has fallen, usually after 3 months of age. By performing the Fontan connection in two stages, the operative risk for the completion Fontan operation has been reduced. When the volume load is acutely removed from the ventricle, the afterload of the single ventricle has been shown to increase. This afterload increasing effect is smaller when only the superior vena cava is connected to the pulmonary artery as compared to the Fontan procedure in which all systemic venous return is diverted into the pulmonary artery. By staging the Fontan, the sometimes fatal combination of ventricular hypertrophy and a sudden decrease in diastolic volume can be avoided. The bidirectional superior cavopulmonary anastomosis, or bidirectional Glenn, allows superior vena caval return to enter both the right and left pulmonary arteries. Because only 40% to 50% of the systemic venous return is presented to the pulmonary arterial bed, patients who would not be candidates for a full Fontan procedure may be able to undergo a bidirectional Glenn shunt. The bidirectional Glenn may also be used in patients with small or dysfunctional right ventricles to create a so-called one and one-half ventricle repair. This may allow some patients who are not candidates for a two-ventricle repair to have the right ventricle manage part of the systemic venous return. A bidirectional Glenn may be performed without cardiopulmonary bypass, using a shunt between the most proximal aspect of the superior vena cava and the right atrial appendage. In this case, two right-angled venous cannulas are selected, approximating the size of the superior vena cava. Purse-string sutures are placed at the superior vena cava-innominate vein junction and in the right atrial appendage. The blood from the right atrium is allowed to fill this cannula, which is then connected to the first cannula, making sure no air is trapped in the connector. The azygos vein is doubly ligated with fine silk ties and divided between the ligatures to allow full mobilization of the superior vena cava and prevent later venous runoff after the Glenn. A tape around the superior vena caval cannula is now snared, and an angled vascular clamp is placed just above the right atrium-superior vena cava junction. The right atrium-superior vena cava junction is oversewn with a running 6-0 Prolene suture, and the vascular clamp is removed. Torsion of the Superior Vena Cava A marking suture should be placed on the superior vena cava to maintain the orientation of the vessel during the anastomosis. The superior aspect of the right pulmonary artery is either grasped with a curved clamp or the branch pulmonary P. The anastomosis of the superior vena cava to the right pulmonary artery is then accomplished with a running 6-0 or 7-0 Prolene suture beginning at the most medial aspect of the pulmonary arteriotomy, completing the posterior row with one needle, and then the anterior aspect with the second needle. If the bidirectional Glenn is to be performed off pump, the source of pulmonary blood flow must be maintained during the construction of the anastomosis. If the pulmonary flow is from the ventricle through a native valve, pulmonary band, or ventricular-pulmonary shunt, placement of the clamp on the right pulmonary artery should be well tolerated. However, if a systemic-pulmonary shunt to the right pulmonary artery is present, the clamp on the right pulmonary artery must be placed carefully. Unless the previous shunt is centrally located on the right pulmonary artery, it may not be possible to perform the bidirectional Glenn without cardiopulmonary bypass. Tension on the Superior Vena Cava-Pulmonary Artery Anastomosis Tension on the anastomosis between the superior vena cava and right pulmonary artery must be avoided by leaving the superior vena cava as long as possible and placing the opening on the right pulmonary artery as close to the transected superior vena cava as feasible. This avoids any tension on the anastomosis that may lead to intraoperative bleeding from the suture line, dehiscence of the suture line, or long-term fibrosis and narrowing of the anastomosis.
Larix europaea (Larch Turpentine). Atrovent.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96621
The Magpie (Magnesium normal physiological fluid shifts during the early post- Sulphate for Prevention of Eclampsia) trial [15] recruited partum period make pre‐eclamptic women particu- 10 141 women with pre‐eclampsia and randomized them larly vulnerable to pulmonary oedema at this time buy cheap atrovent on-line symptoms 10 days before period. The greatest effect was seen and in all women injudicious fluid management in pre‐ in women who were at the highest risk: 63 women with eclampsia was felt to be a significant contributory factor buy discount atrovent 20 mcg on-line rust treatment. No benefit was seen in other outcomes including deaths in this group of patients in the following triennial maternal or neonatal morbidity or mortality discount atrovent 20 mcg otc medicine 513. Cochrane reviews have reported that magnesium sul- the current recommended practice is to restrict fluid fate is superior to diazepam or phenytoin for the treat- intake to 80mL/hour until a postpartum diuresis is ment of eclampsia [43]. In women where there are ongoing losses or maternal fits is reduced and improved neonatal out- where persistent minimal urine output raises concerns comes, including reduced need for admission to special about renal injury, invasive monitoring may help guide care baby unit or ventilation, are seen in women who fluid replenishment whilst avoiding overload. The precise mechanisms by which magnesium sulfate Anaesthetic issues acts to reduce cerebral irritability is unclear. It is a vasodi- lating agent and contributes to reduction of cerebral per- Both regional and general anaesthesia can be problematic fusion pressures but it also has other relevant properties in the pre‐eclamptic patient. Magnesium sulfate is advocated for labouring pre‐eclamptic women due to the emerging as a potential agent to reduce rates of cerebral belief that it will contribute to lowering of blood pressure palsy in preterm infants, although the mechanism and by reducing both pain‐associated anxiety and peripheral optimal dose for this purpose remain unclear. Whilst there may be a modest antihyper- erties may contribute to improved neonatal outcomes in tensive effect there do not appear to be any significant women who deliver preterm due to pre‐eclampsia. As in the gen- dose over 5min followed by an infusion of 1g/hour eral obstetric population, epidural anaesthesia is associ- which is usually maintained for 24 hours. Recurrent sei- ated with a longer second stage and increased incidence zures should be treated with a further dose of 2–4 g over of instrumental delivery. There is therefore no evidence 5 min and diazepam should be reserved for use in women to recommend the routine use of epidural anaesthesia in who continue to fit despite magnesium sulfate. The ther- labouring pre‐eclamptic women and the diagnosis should apeutic range for magnesium plasma levels is 4–8mg/ not influence the woman’s choice of analgesia for labour. A platelet count 9 excreted in the urine and toxicity is therefore more likely below 80 × 10 /L is a contraindication to regional anaes- in women who have renal manifestations of pre‐eclamp- thesia due to the increased risk of spinal haematoma. Calcium gluconate 1g (10mL of 10% solution) over General anaesthesia can be complicated by exacerba- 2min is administered to reverse magnesium toxicity tion of severe hypertension in response to intubation. Furthermore, laryngeal oedema can make intubation technically difficult and should only be undertaken by senior anaesthetic clinicians. The greatest risks are seen in women who have not been appropriately stabilized Summary box 7. Complications ● Magnesium sulfate is the drug of choice for the pre- Hepatic vention of eclamptic seizures. Approximately 12% of women with severe pre‐ ● Over 25% of eclamptic seizures will occur postnatally. Not all components are necessarily evident at presentation and the diagnosis is not necessarily asso- One‐third of women who have had pregnancy‐induced ciated with the most severe hypertensive presenta- hypertension or pre‐eclampsia will sustain hypertension tions. Many affected women will be asymptomatic or in the postnatal period and this increases to over 75% in will present with non‐specific malaise and nausea, women who have had preterm delivery triggered by although a few will describe classical epigastric and maternal hypertensive disease. The diagnosis is tension causes anxiety for the woman and her carers, based on laboratory investigations including a blood delays discharge to the community and can occasionally film, platelet count and measurement of liver transam- put her at risk of significant complications. High‐dose evidence to inform clinicians when managing postpar- steroids have been used to try to hasten the recovery of tum hypertension and until such evidence is available a thrombocytopenia but this has not been shown to be pragmatic approach has been recommended [17]. This complication is All women who have been prescribed antenatal antihy- associated with a significant risk of maternal mortality. Women who have been given methydopa should may be appropriate in the postpartum patient who is be changed to an alternative agent before the third post- haemodynamically stable and where the haematoma is natal day due to the association of methyldopa with post- not expanding. If the blood pressure is persistently stasis at laparotomy include compression, haemostatic below 140/90 mmHg, then reduce the dose. Most women sutures, application of topical coagulation agents, embo- will not require medication beyond 6 weeks. Renal Women who have not previously been treated with Although glomerular capillary endotheliosis is a classic antihypertensives should have their blood pressure mon- pathological feature of pre‐eclampsia and relative oligu- itored four times daily while an inpatient and should be ria is common in the early postpartum period, these fea- treated if blood pressure is above 150/100mmHg. Acute renal failure is Women in the community should have their blood pres- a rare complication of pre‐eclampsia, with an estimated sure measured once between days 3 and 5 using a similar incidence of 1 in 10 000–15 000 pregnancies. If medication is initiated, fol- haemorrhage is a much more common precipitating fac- low‐up should be within 48 hours to ensure an appropri- tor in this population. Dialysis is rarely required in women who do not woman describing severe headache or epigastric pain have pre‐existing renal pathology. Women who have developed pre‐eclampsia should be offered an obstetric review around 6 weeks after birth. This affords Neurological the opportunity to confirm that hypertension and pro- Neurological sequelae of pre‐eclampsia, other than fits, teinuria have resolved, or to arrange referral for further include cerebral haemorrhage, encephalopathy and tem- investigation if there are concerns about underlying porary blindness (amaurosis). Women should be made aware of their risk of autoregulation, increased perfusion pressures and developing pre‐eclampsia in future pregnancies; overall increased vascular permeability are contributory factors the risk of recurrence is around 16% but this increases to but the aetiology is complicated by haemoconcentration 55% if they were delivered before 28 weeks’ gestation due predisposing to thrombosis and vasospasm associated to hypertensive disease. Any focal neurological signs should be investi- identify any other modifiable risk factors which might be gated with cranial imaging to exclude other pathologies addressed prior to embarking on another pregnancy, for but no specific treatment is recommended. Both the who are at increased risk of future cardiovascular mor- American College of Obstetricians and Gynecologists bidity. The proposed pathogenic remains a paucity of evidence as to which health profes- hypotheses include shared genetic risk factors for pre‐ sionals are best placed to carry out the assessment and eclampsia and cardiovascular disease causing pregnancy what should be included beyond informing the woman to reveal an underlying susceptibility [46], persistence of of her increased risk. Whatever the underlying patho- circulating factors that promote endothelial dysfunction genesis, it seems plausible that targeting monitoring and [47] or altered endothelial progenitor cell function activity lifestyle modifications to this group of women might [48]. Alternatively, persistent subclinical impairment of ameliorate future cardiovascular events. Soluble Global, regional, and national levels and causes of endoglin contributes to the pathogenesis of maternal mortality during 1990–2013: a systematic preeclampsia. Obstet and lessons learned to inform maternity care from the Gynecol 2002;99:159–167. Oxford: National pre‐eclampsia, and their babies, benefit from Perinatal Epidemiology Unit, University of Oxford, 2015. Instituting surveillance to endothelial dysfunction, hypertension, and guidelines and adverse outcomes in preeclampsia. Glomerular endothelial cell Hypertension in Pregnancy: Diagnosis and differentiation. Increased revised British Hypertension Society protocol for the expression of sFlt‐1 in in vivo and in vitro models of evaluation of blood pressure measuring devices. Uteroplacental Hypertension recommendations for conventional, ischemia results in proteinuric hypertension and ambulatory and home blood pressure measurement. The measurement of blood combining clinical risk and biomarkers: the Screening pressure and proteinuria in pregnancy. Lack of reproducibility in pregnancy of Korotkoff endogenously encoded soluble receptor. Reductions of vascular endothelial Accuracy of urinalysis dipstick techniques in predicting growth factor and placental growth factor significant proteinuria in pregnancy. Magnesium sulphate and other anticonvulsants for angiogenic factors and the risk of preeclampsia. Delayed postpartum preeclampsia: an suspected preeclampsia: a prospective multicenter experience of 151 cases.