
Western New Mexico University. L. Rathgar, MD: "Order Minocycline - Cheap online Minocycline no RX".
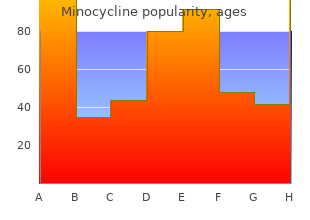
In patients who are not responding to antimicrobial therapy purchase minocycline 50mg overnight delivery antimicrobial journal, Pediatrics minocycline 50 mg with mastercard antibiotic resistance developing countries, 2011;159(2):181-5 buy minocycline mastercard antibiotics for dogs how long. There is geographic and temporal relationship to laboratory- seasonal and geographical variation in the causative organism. For surveillance purposes, all the acute or in which testing was performed but no etiological encephalitis cases to be reported under the heading of acute agent was identifed or in which the test results were encephalitis. Features of raised intracranial tension are at any time of year with the acute onset of fever and a change commonly present in acute stage of illness. The patient may in mental status (including symptoms such as confusion, develop difculty of speech and other neurological defcits disorientation, come, or inability to talk) and/or new onset like ocular palsies, hemiplegia, quadriplegia and may have of seizures (excluding simple febrile seizures). Other early extrapyramidal signs in the form of dystonia, choreoathetosis, clinical fndings may include an increase in irritability, and coarse tremors. T eir case management It is important to note that in an epidemic situation fever usually follows a common protocol along with situation with altered sensorium persisting for more than 2 hours with specifc treatment. To reduce severe history and Examination morbidity and mortality, it is important to identify early The following are the important aspects in history and warning signs and refer patients to health facility. In children above 12 years fuid should be examined for cytology, biochemistry, Gram 10 mg/kg 8 hourly. Duration of treatment in confrmed stain, Ziehl–Neelsen stain for acid fast bacilli, bacterial cases should be 14–21 days intravenous treatment and culture, latex agglutination, polymerase chain reaction minimum 21 days for those aged 3 months to 12 years for herpes simplex virus 1 and 2, and immunoglobulin • Artemether combination therapy: in cerebral malaria. Peripheral smear for malarial parasite and rapid • Steroids: pulse steroids (methylprednisolone or dexa- diagnostic test for malaria should be obtained. Chest X-ray methasone) to be given in children with suspected acute should also be obtained disseminated encephalomyelitis. Computed tomography may also show brain and exposure keratitis herniation, efacement of cisterns, infective collections • Complications like aspiration pneumonia, nosocomial such as brain abscesses and subdural empyema. Guidelines: Clinical Management of Acute Encephalitis Syndrome including Japanese Encephalitis. Management of suspected viral encephalitis in children-Association of British Neurologists and British Pediatric Allergy Immunology and Infection Group National Guidelines. Consensus ))Case fatality is high and survivors often have neurologic Guidelines on Evaluation and management of Suspected Acute Viral Encephalitis sequelae in Children in India. Japanese encephalitis immediate consideration of vital functions, identifcation of surveillance standards. Early recognition of acute osteomyelitis in young patients before extensive infection develops and prompt institution of appropriate medical and surgical therapy minimize permanent damage. Acute osteomyelitis in neonates and infants is commonly associated with septic arthritis due to peculiar vascularity of the physis and epiphysis. Once the growth plate forms, it acts as a barrier and in toddlers and children the infection is usually confned to the metaphysis. In the metaphysis, nutrient arteries branch into non-anastomosing capillaries under the physis, which make a sharp loop before entering venous sinusoids draining into the marrow (Fig. Blood fow in this area is sluggish and provides an ideal environment for bacteria seeding. Once a bacterial focus is established, phagocytes migrate to the site and produce infammatory exudates (metaphyseal abscess). The generation of proteolytic enzymes, toxic oxygen radicals, and cytokines result in decreased oxygen tension, decreased pH, osteolysis, and tissue destruction. As the infammatory exudate progresses, pressure increases spread through the porous metaphyseal space via the Haversian system and Volkmann canals into the subperiosteal space. In the newborns and young infants, transphyseal blood vessels connect the metaphysis and epiphysis (Fig. Joint involvement their association with diferent conditions once the physis forms may occur in joint where the metaphysis Common clinical association Microorganism is intraarticular (hip, ankle, shoulder, and elbow) and subperiosteal pus ruptures into the joint space. With trivial infections (catheters) Staphylococcus) trauma, the hematoma which forms in the metaphysis acts as a Nosocomial infections Enterobacteriaceae, Pseudomonas, perfect soil for bacteria to seed. Escherichia coli, Klebsiella, and Group B streptococci are also prominent pathogens in neonates. Group A streptococci constitutes less Box 1: Common clinical manifestations than 10% of all cases. Fungal • Local edema, erythema, tenderness, cellulitis infection usually occurs as part of multisystem disseminated disease. Candida osteomyelitis sometimes complicates • Limp or refusal to walk in older children with involvement fungemia in neonates with indwelling vascular catheters. It is very common scenario at our set up that out of the metaphysis into the subperiosteal space. It a neonate presents with acute osteomyelitis after few days of represents secondary soft tissue infammatory response discharge from nursery. The femur and tibia acute osteomyelitis in children in many parts of the world, together constitute almost half of the cases. The signs and symptoms of acute osteomyelitis are highly dependent on the age of the patient (Box 1). Pseudo- bone infections but are non-specifc and cannot distinguish paralysis (restriction of movement) is very common in between skeletal infections and other infammatory 236 neonates and young infants due to pain conditions. It may be positive in 50% of cases with infection hemaotgenous osteomyelitis • Efective in early detection and surgical localization of • Aspiration for Gram stain and culture is the defnitive osteomyelitis diagnostic technique. Conventional radiographs, ultrasonography, ascertain clinically computed tomography, magnetic resonance imaging and • Can detect osteomyelitis within 24–48 hours after onset of radionuclide studies may all contribute to establishing symptoms the diagnosis. Plain radiographs are often used for initial • T ree phase imaging with 99 m Tc has 85–100% sensitivity evaluation to exclude other causes such as trauma and foreign and 75–95% specifcity in hematogenous osteomyelitis bodies. Magnetic resonance imaging has emerged as a very • Sensitivity in neonates is much lower due to poor bone sensitive and specifc test and is widely used for diagnosis. Lytic bone changes • Hemophilia are not visible on radiographs until 30–50% of bony matrix • Collagen disorders is destroyed. Antibiotic Therapy (Box 4) Box 3: Radio imaging studies The primary treatment for osteomyelitis is parenteral anti- • Plain radiograph shows lytic bone changes after 7–14 days of biotics that penetrate bone and joint covities and most efective onset of infection. Contractures and Early Mobility {{ If neonate is a preterm baby or has a central vascular Prognosis catheter → Possibility of nosocomial bacteria like • When the pus is drained and appropriate antibiotic therapy pseudomonas or coagulase negative staphylococcus or is given, improvement in signs and symptoms is rapid fungi should be considered • Failure to improve or worsening by 72 hours, requires • In older infants and children: review of the appropriateness of antibiotic therapy, need {{ Common organisms are S. In addition to good anti-staphylococcus activity, clindamycin Acute osteomyelitis in children is an important condition has broad activity against anaerobes and is useful for the because of its potential to cause permanent disability. Long bones are commonly involved in acute osteomyelitis in erythema, tenderness, and cellulitis are other manifestations. The unique anatomy and circulation of the ends of There are no specifc laboratory tests for osteomyelitis. Blood culture should osteomyelitis in neonates and infants is commonly associated be routine in all cases of suspected osteomyelitis. Aspiration with septic arthritis due to peculiar vascularity of physis and for Gram stain and culture is the defnite diagnostic technique. Bacteria are the most common pathogens in acute Radio imaging studies play a crucial role in evaluation of osteomyelitis in children. Plain radiograph shows lytic bone changes after common infecting organism in all age groups, including 7–14 days of onset infection. Sickle cell anemia, penetrating injuries, nosocomial changes for diagnosis of acute osteomyelitis, it is very late.
Thus buy cheap minocycline antibiotics for klebsiella uti, ventricular rate is often some fixed ratio of the atrial rate (2:1 cheap minocycline 50mg visa treatment for dogs cracked nose, 4:1) with frequencies often 150 to 220 beats/min discount minocycline 50 mg with mastercard antibiotic resistance and public health. At nor mal heart rates, the physiological efects of the first-degree block are inconsequential. The danger, however, is that the slow conduction may deteriorate to an actual interruption of conduction. Atrial rate is often faster than ventricular rate by a certain ratio (eg, 2:1, 3:1, and 4:1). This condition may not represent a serious clinical problem as long as the ventricular rate is adequate to meet the pumping needs. Ventricular rate is very likely to be slower than normal (bradycardia) and is often slow enough to impair cardiac output. Atrial fbrilltion (trace 6 in Figure 5-1) is characterized by a complete loss of the normally close synchrony of the excitation and resting phases between individual atrial cells. Cells in different areas of the atria depolarize, repolarize, and are excited again randomly. Consequently, no P waves appear in the elec trocardiogram, although there may be rapid, irregular, small waves apparent throughout diastole. The mechanisms behind it are not well understood, but impulses are thought to progress repeatedly around irregular conduction pathways (sometimes called circus pathways, which imply a reentry phenomenon as described earlier and in Figure 5-3). Conduction blocks called bundl branch blocks or hemiblocks (trace 2 in Figure 5-2) can occur in either of the branches of the Purkinje system of the intraventricular septum, often as a result of a myocardial infarction. Ventricular depolarization is less synchronous than normal in the half of the heart with the nonfunctional Purkinje system. The direct physiological efects of bundle branch blocks are usually inconsequential. The shapes of the electrocardiographic records of these extra beats are highly variable and depend on the ectopic site of their origin and the depolarization pathways involved. The volume of blood ejected by the premature beat itself is smaller than normal, whereas the stroke volume of the beat following the compensatory pause is larger than nor mal. This is partly due to the diferences in flling times and partly to an inherent phenomenon of the cardiac muscle called posteastolic potentaton. Vntriculr tachycardia (trace 4 in Figure 5-2) occurs when the ventricles are driven at high rates, usually by impulses originating from a ventricu lar ectopic focus. Not only is diastolic flling time limited by the rapid rate, but also the abnormal excita tion pathways make ventricular contraction less synchronous and therefore less efective than normal. These clots can fragment and move out of the heart to lodge in small arteries throughout the systemic circulation. Consequently, anticoagulant therapy is usually prescribed for patients in atrial fbrillation. It may be genetic in origin (mutations infuenc ing various ion channels involved with cardiac excitability), may be acquired from several electrolyte disturbances (low blood levels of Ca2+, Mg2+, or K+), or may be induced by several pharmacological agents (including some antiarrhythmic drugs). This differs from the ordinary ventricular tachycardia in that the ventricular elec trical complexes cyclically vary in amplitude around the baseline and can deterio rate rapidly into ventricular fbrillation. In ventriculrfbrilltion (trace 6 in Figure 5-2), various areas of the ventricle are excited and contract asynchronously. The ventricle is especially susceptible to fbrillation whenever a premature excitation occurs at the end of the T wave of the previous excitation, that is, when most ventricular cells are in the "hyperexcitable" or "vulnerable" period of their electrical cycle. In addition, because some cells are repolarized and some are still refractory, circus pathways can be triggered easily at this time. Because no pumping action occurs with ventricular fbrillation, the situation is fatal unless quickly corrected by cardiac conversion. During conversion, the artif cial application of large currents to the entire heart (via paddle electrodes applied across the chest) may be effective in depolarizing all heart cells simultaneously, thus allowing a normal excitation pathway to be reestablished. Abnormal heart sounds, which often accompany cardiac valvular defects, are called murmurs. These sounds are caused by abnormal pressure gradients and turbulent blood flow patters that occur during the cardiac cycle. A number of techniques, ranging from simple auscultation (listening to the heart sounds) to echocardiography or cardiac catheterization, are used to obtain information about the nature and extent of these valvular malfunctions. In general, when a valve does not open fully (ie, is stenotic), the chamber upstream of the valve has to develop more pressure during its systolic phase to achieve a given fow through the valve. This increase in "pressure" work will induce hypertrophy of cardiac muscle cells and thickening of the walls of that chamber. When a valve does not close completely (ie, is insufcient), the regur gitant blood fow represents an additional volume that must be ejected in order to get sufcient fotward fow out of the ventricle into the tissues. If capillary hydrostatic pressures are elevated, tissue edema will ensue with consequences on the function of those upstream organs. A brief overview of four of the common valve defects infuencing left ventricu lar function is given in Figure 5-4. Note that similar stenotic and regurgitant abnormalities can occur in right ventricular valves with similar consequences on right ventricular function. Normally, the aortic valve opens widely and ofers a pathway of very low resistance through which blood leaves the left ventricle. If this opening is narrowed (stenotic), resistance to flow through the valve increases. A significant pressure diference between the left ventricle and the aorta may be required to eject blood through a stenotic aortic valve. As shown in Figure 5-4A, intraven tricular pressures may rise to very high levels during systole, while aortic pressure rises more slowly than normal to a systolic value that is subnormal. High intraventricular pressure development is a strong stimulus for cardiac muscle cell hypertrophy, and an increase in left ven tricular muscle mass invariably accompanies aortic stenosis. This abnormal turbulent flow can be heard as a systolic (or ejection) murmur with a properly placed stethoscope. The primary physiological consequence of aortic stenosis is a high ventricular afterload that is caused by restriction of the outflow tract. A pres sure diference of more than a few millimeters of mercury across the mitral valve during diastole is distinctly abnormal and indicates that this valve is stenotic. Consequently, as shown in Figure 5-4B, left atrial pressure is elevated with mitral stenosis. The high left 2 A useful analogy is to compare the hypertrophied skeletal muscles of the weightlifter (doing isometric or pressure work) to the nonhypertrophied but well-toned skeletal muscles of the long-distance runner (doing isotonic or shortening work). Characteristics of left ventricular valve abnormalities: (A) aortic stenosis, (B) mitral stenosis, (C) aortic regurgitation (insufciency), and (D) mitral insufciency. Elevated left atrial pressure is reflected back into the pulmonary bed and, if high enough, causes pulmonary congestion and "shortness of breath. The primary physiological consequences of mitral stenosis are elevations in left atrial pressure and pulmonary capillary pressure.
Alpinia Officinarum (Alpinia). Minocycline.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96299
The important functions performed by the kidneys include the following: They regulate the osmolarity of the body fluids by altering renal water reabsorption to excrete osmotically dilute or concentrated urine 50mg minocycline with amex virus 7g7 part 0. They eliminate the waste products of metabolism order minocycline 50mg line bacteria habitat, including urea (the main nitrogen-containing end product of protein metabolism in humans) discount 50 mg minocycline with visa topical antibiotics for acne in pregnancy, uric acid (an end product of purine metabolism), and creatinine (an end product of muscle metabolism). They are the major sites of production of certain hormones, including erythropoietin (see Chapter 9) and 1,25-dihydroxy vitamin D (see 3 Chapter 35). They degrade several polypeptide hormones, including insulin, glucagon, and parathyroid hormone. They synthesize ammonia, which plays a role in acid–base homeostasis (see Chapter 24). Dialysis and kidney transplantation are commonly used treatments for advanced (end-stage) renal failure. Each renal corpuscle is derived from a muscular afferent arteriole that forms a tuft of capillaries, the glomerulus, which is surrounded by the Bowman capsule. The Bowman capsule, which cups around the glomerulus, collects the fluid filtered from the glomerulus. The blood leaving the glomerulus that was not filtered is carried via the efferent arteriole. On the left is a long-looped juxtamedullary nephron; on the right is a superficial cortical nephron. Common causes include diabetes mellitus, hypertension, inflammation of the glomeruli (glomerulonephritis), urinary reflux and infections (pyelonephritis), and polycystic kidney disease. Renal damage may occur over many years and may be undetected until a considerable loss of functioning nephrons has occurred. Most of the signs and symptoms of renal failure can be relieved by dialysis, the separation of smaller molecules from larger molecules in solution by diffusion of the small molecules through a selectively permeable membrane. Two methods of dialysis are commonly used to treat patients with severe, irreversible (end-stage) renal failure. In continuous ambulatory peritoneal dialysis, the peritoneal membrane, which lines the abdominal cavity, acts as a dialyzing membrane. About 1 to 2 L of a sterile glucose/salt solution are + introduced into the abdominal cavity, and small molecules (e. The blood is separated from a balanced salt solution by a cellophane-like membrane, and small molecules can diffuse across this membrane. Hemodialysis is usually done three times a week (4 to 6 hours per session) in a medical facility or at home. Dialysis can enable patients with otherwise fatal renal disease to live useful and productive lives. However, many physiologic and psychologic problems persist, including alteration of body calcium levels and bone disease, disorders of nerve function, hypertension, atherosclerotic vascular disease, + sudden cardiac death due to plasma K disturbances, and disturbances of sexual function. There is a constant risk of infection and, with hemodialysis, clotting and hemorrhage. Anemia (primarily resulting from deficient erythropoietin production by damaged kidneys) was once a problem but can now be treated with recombinant human erythropoietin. Renal transplantation is the only real cure for patients with end-stage renal failure. Patients who have had a kidney transplant have more energy, can enjoy a less restricted diet, have fewer complications, and live much longer than if they had stayed on dialysis. In 2014, about 17,000 kidney transplantation operations were performed in the United States with about two thirds of the donated kidneys coming from living donors and the remaining third from deceased donors. At present, about 95% of kidneys grafted from a living donor related to the recipient function for 1 year; about 90% of kidneys from cadaver donors function for 1 year. The powerful drugs used to inhibit graft rejection compromise immune defensive mechanisms so that unusual and difficult-to-treat infections often develop. The limited supply of donor organs is also a major, unsolved problem; there are many more patients who would benefit from kidney transplantation than there are donors. In 2014, over 4,200 patients died awaiting kidney transplants with another 3,600 becoming too ill to receive a kidney transplant. The median waiting time for a kidney transplant is currently about 1,100 to 1,200 days. Fortunately, for people in the United States, Medicare covers the cost of dialysis and transplantation, but these lifesaving therapies are beyond the reach of most people in developing countries. This is subdivided into a proximal convoluted tubule followed by the proximal straight tubule. The straight portion heads toward the medulla, away from the surface of the kidney, and into the loop of Henle. In nephrons contained within the renal cortex, the loop of Henle includes the proximal straight tubule, a thin descending limb, and a thick ascending limb. In juxtamedullary nephrons, which are a subgroup of nephrons whose loops of Henle descend deep into the renal medulla, a thin ascending limb is interposed between the thin descending and thick ascending limbs. The thick ascending limb of both types of nephrons leads into the next segment of the nephron called the distal convoluted tubule. The distal convoluted tubule extends from the macula densa (see below) to a connecting tubule, which is connected to the collecting duct system. Approximately 12% of the total nephron population contain specialized sets of cells located between the renal corpuscle and the distal convoluted tubule. This specialized grouping is the juxtaglomerular apparatus, so named for its proximity to the glomerulus (Fig. The juxtaglomerular apparatus consists of three cellular components: the macula densa of the distal convoluted tubule, extraglomerular mesangial cells, and granular cells (also known as juxtaglomerular cells). The macula densa (dense spot) consists of densely crowded tubular epithelial cells on the side of the thick ascending limb that faces the glomerular tuft; these cells monitor the composition of the fluid in the tubule lumen. The extraglomerular mesangial cells are continuous with mesangial cells of the glomerulus; they may transmit information from macula densa cells to the granular cells. The granular cells are modified vascular smooth muscle cells with an epithelioid appearance, located mainly in the afferent arterioles close to the glomerulus. These cells synthesize and release renin, an enzyme that hydrolyses angiotensinogen to form angiotensin I and thus participates in the body’s renin–angiotensin–aldosterone system. It also contributes to the regulation of arterial blood pressure (see Chapters 17 and 23). A cross-section through a thick ascending limb is below, and part of a glomerulus is on top. The arrangement of the nephrons within the kidney gives rise to two distinct regions: an outer part, called the cortex, and an inner part, called the medulla (see Fig. All of the glomeruli, convoluted tubules, and cortical collecting ducts are located in the cortex. The medulla is lighter in color and has a striated appearance that results from the parallel arrangement of the loops of Henle, medullary collecting ducts, and blood vessels of the medulla. All nephrons originate in the cortex, but the glomeruli of the cortical nephrons lie in the outer layer of the cortex, whereas the glomeruli of the juxtamedullary nephrons lie in the inner layer of the cortex next to the medulla.
In the lung proven minocycline 50 mg treatment for uti bactrim dose, two additional factors (alveolar surface tension and pressure) are involved in fluid exchange buy minocycline discount antibiotic resistance world health organization. Alveolar surface tension enhances filtration order minocycline online pills k. pneumoniae antibiotic resistance, whereas alveolar pressure opposes filtration. The relatively low pulmonary capillary hydrostatic pressure helps keep the alveoli “dry” and prevents pulmonary edema. Mean pulmonary capillary hydrostatic pressure is normally 8 to 10 mm Hg, which is lower than the plasma colloid osmotic pressure (25 mm Hg). This is functionally important because the low hydrostatic pressure in the pulmonary capillaries favors the net absorption of fluid. Alveolar surface tension tends to offset this advantage and results in a net force that still favors a small continuous flux of fluid out of the capillaries and into the interstitial space. This excess fluid travels through the interstitium to the perivascular and peribronchial spaces in the lungs, where it then passes into the lymphatic channels (see Fig. The lymphatic vessels are not found in the alveolar–capillary area but are strategically located near the terminal bronchioles to drain off excess fluid. Lymphatic channels, like small pulmonary blood vessels, are held open by tethers from surrounding connective tissue. Pulmonary edema occurs when excess fluid accumulates in the lung interstitial spaces and alveoli and usually results when capillary filtration exceeds fluid removal. Pulmonary edema can be classified as cardiogenic pulmonary edema (due to heart dysfunction) or noncardiogenic pulmonary edema (due to lung injury). Cardiogenic pulmonary edema is caused by an increase in capillary hydrostatic pressure or by a decrease in plasma colloidal osmotic pressure. Increased capillary hydrostatic pressure is the most frequent cause of pulmonary edema and is often the result of an abnormally high pulmonary venous pressure (e. The second major cause of pulmonary edema is noncardiogenic and is due to increased alveolar surface tension and/or increased permeability of the alveolar–capillary membrane. Both types of noncardiogenic result in excess fluid and plasma proteins flooding the interstitial spaces and alveoli. Protein leakage makes pulmonary edema more severe because additional water is pulled from the capillaries to the alveoli when plasma proteins enter the interstitial spaces and alveoli. Increased capillary permeability occurs with pulmonary vascular injury, usually from oxidant damage (e. Loss of surfactant leads to high surface tension, which lowers the interstitial hydrostatic pressure with a concomitant increase in capillary fluid entering the interstitial space. Pulmonary edema can also flood2 small airways, thereby obstructing airflow and increasing airway resistance. Lung compliance is decreased with pulmonary edema because of interstitial swelling and the increase in alveolar surface tension. Decreased lung compliance, together with airway obstruction, greatly increases the work of breathing. The treatment of pulmonary edema is directed toward reducing pulmonary capillary hydrostatic pressure. This is accomplished by decreasing blood volume with a diuretic drug, increasing left ventricular function with digitalis, and administering a drug that causes vasodilation in systemic blood vessels. Although freshwater drowning is often associated with aspiration of water into the lungs, the cause of death is not pulmonary edema but ventricular fibrillation. The low capillary pressure that normally keeps the alveolar–capillary membrane free of excess fluid becomes a severe disadvantage when freshwater accidentally enters the lungs. The aspirated water is rapidly pulled into the pulmonary capillary circulation via the alveoli because of the low capillary hydrostatic pressure and high colloidal osmotic pressure. Consequently, the plasma is diluted and the hypotonic environment causes red cells to burst + + (hemolysis). The resulting elevation of plasma K level and depression of Na level alter the electrical activity of the heart. Ventricular fibrillation often occurs as a result of the combined effects of these electrolyte changes and hypoxemia. In saltwater drowning, the aspirated seawater is hypertonic, which + leads to increased plasma Na and pulmonary edema. Hypoxia relaxes vascular smooth muscle in systemic vessels and elicits vasoconstriction in the pulmonary vasculature. Hypoxic pulmonary vasoconstriction is the major mechanism regulating the matching of regional blood flow to regional ventilation in the lungs. With regional hypoxia, the matching mechanism automatically adjusts regional pulmonary capillary blood flow in response to alveolar hypoxia and prevents blood from perfusing poorly ventilated regions in the lungs. Regional hypoxic vasoconstriction occurs without any change in pulmonary arterial pressure. However, when hypoxia affects all parts of the lung (generalized hypoxia), it causes pulmonary hypertension because all of the pulmonary vessels constrict. With chronic hypoxia-induced pulmonary hypertension, the pulmonary artery undergoes major remodeling during several days. An increase in wall thickness results from hypertrophy and hyperplasia of vascular smooth muscle and an increase in connective tissue. Also, there is abnormal extension of smooth muscle into peripheral pulmonary vessels, where muscularization is not normally present; this is especially pronounced in precapillary segments. With severe, chronic hypoxia-induced pulmonary hypertension, the obliteration of small pulmonary arteries and arterioles as well as pulmonary edema eventually occurs. The latter is caused, in part, by the hypoxia-induced vasoconstriction of pulmonary veins, which results in a significant increase in pulmonary capillary hydrostatic pressure. A striking feature of the vascular remodeling is that both the pulmonary artery and the pulmonary vein constrict with hypoxia; however, only the arterial side undergoes major remodeling. The postcapillary segments and veins are spared the structural changes seen with hypoxia. Because of the hypoxia-induced vasoconstriction and vascular remodeling, pulmonary arterial pressure increases. The gravitational effect on pulmonary blood flow is dramatic and results in an uneven distribution of blood in the lungs. Because the vessels are highly compliant, gravity causes the blood volume and flow to be greater at the bottom of the lung (the base) than at the top (the apex). The difference in arterial pressure between the apex and the base of the lungs is about 30 cm H O. Because the heart is situated midway between the top and the bottom of the lungs, the2 arterial pressure is about 11 mm Hg less (15 cm H O ÷ 1. As a result, the low pulmonary arterial pressure results in reduced blood flow in the capillaries at the lungs’ apex, whereas capillaries at the base are distended because of increased pressure and blood flow is augmented. Gravity causes lungs to be underperfused at the apex and overperfused at the base. In an upright person, pulmonary blood flow decreases almost linearly from the base to the apex (Fig. Blood flow distribution is affected by gravity and can be altered by changes in body positions. For example, when a person is lying down, blood flow is distributed relatively evenly from the base to the apex.