
Cleveland Chiropractic College. Z. Lee, MD: "Purchase online Digoxin no RX - Safe Digoxin online".
This phenomenon may explain the association between elevated levels of lipoprotein(a) and 27 atherosclerosis (see also Chapters 45 and 48) buy 0.25 mg digoxin mastercard hypertension 140 90. Thrombosis A physiologic host defense mechanism discount digoxin master card blood pressure 70 over 40, hemostasis focuses on arrest of bleeding by forming hemostatic plugs composed of platelets and fibrin at sites of vessel injury buy discount digoxin 0.25 mg on line prehypertension range chart. In contrast, thrombosis reflects a pathologic process associated with intravascular thrombi that fill and occlude the lumens of arteries or veins. Arterial Thrombosis (see also Chapter 44) Most arterial thrombi occur on top of disrupted atherosclerotic plaques. Coronary plaques with a thin 1 fibrous cap and a lipid-rich core are most prone to disruption. Rupture of the fibrous cap exposes thrombogenic material in the lipid-rich core to blood and triggers platelet activation and thrombin generation. The extent of plaque disruption and the content of thrombogenic material in the plaque determine the consequences of the event, but host factors also contribute. Breakdown of the regulatory mechanisms that limit platelet activation and inhibit coagulation can augment thrombosis at sites of plaque disruption. Decreased production of nitric oxide and prostacyclin by diseased endothelial cells can 29 trigger vasoconstriction and platelet activation. Products of blood coagulation contribute to atherogenesis, as well as to its complications. Microscopic erosions in the vessel wall trigger the formation of tiny platelet-rich thrombi. Incorporation of microthrombi into plaque promotes their growth, and decreased endothelial cell production of heparan sulfate—which normally limits smooth muscle proliferation—contributes to plaque expansion. The multiple links between atherosclerosis and thrombosis have prompted the term atherothrombosis. Venous Thrombosis (see also Chapter 84) Venous thrombosis may be caused by genetic or acquired hypercoagulable states or by such factors as advanced age, obesity, or cancer, which are usually acquired and are associated with immobility (Table 93. Inherited hypercoagulable states and these acquired risk factors combine to establish the intrinsic risk for thrombosis in each individual. Superimposed triggering factors, such as surgery, smoking, pregnancy, or hormonal therapy, modify this risk, and thrombosis occurs when the combination of genetic, acquired, and triggering forces exceeds a critical threshold (Fig. Hereditary and acquired risk factors combine to create an intrinsic risk for thrombosis in each individual. If the intrinsic and extrinsic forces exceed a critical threshold at which thrombin generation overwhelms protective mechanisms, thrombosis occurs. For example, major orthopedic surgery, neurosurgery, multiple traumas, and metastatic cancer (particularly adenocarcinoma) entail the highest risk, whereas prolonged bed rest, the presence of antiphospholipid antibodies, and the puerperium are associated with intermediate risk; pregnancy, obesity, long-distance travel, and the use of oral contraceptives or hormonal replacement therapy are mild risk factors. The following sections describe the inherited and acquired hypercoagulable states. Inherited Hypercoagulable States Inherited hypercoagulable states fall into two categories. Some are associated with gain-of-function mutations in procoagulant pathways, such as factor V Leiden, the prothrombin gene mutation, and increased levels of procoagulant proteins; others are associated with loss-of-function mutations of endogenous anticoagulant proteins, such as deficiencies of antithrombin, protein C, and protein S. Factor V Leiden The factor V Leiden mutation, present in about 5% of white individuals, is the most common inherited thrombophilia. Because of a founder effect, the mutation is less common in Hispanics and blacks and rare in Asians. Caused by a point mutation in the factor V gene, the defect results in the synthesis of a factor V molecule with a Gln residue in place of an Arg residue at position 506, one of three sites where activated protein C cleaves factor Va to inactivate it. Consequently, activated factor V Leiden resists rapid proteolysis and persists 10-fold longer in the presence of activated protein C than its wild-type counterpart does. However, the absolute risk for venous thrombosis is low with factor V Leiden, and with a yearly risk of 0. An activated protein C resistance assay establishes the diagnosis of factor V Leiden in most cases. Prothrombin Gene Mutation The second most common thrombophilic disorder, the prothrombin gene mutation, reflects a G-to-A nucleotide transition at position 20210 in the 3′-untranslated region of the prothrombin gene. This mutation causes elevated levels of prothrombin, which enhance thrombin generation. The prevalence of the prothrombin gene mutation is about 3% in white persons and is lower in Asians and blacks. The mutation increases the risk for venous thrombosis to a similar extent as factor V Leiden does. Although persons heterozygous for this mutation have 30% higher levels of prothrombin than noncarriers do, the wide range of prothrombin levels in healthy individuals precludes the use of this phenotype for carrier identification. Although the molecular bases for the high levels of these coagulation factors have yet to be identified, genetic mechanisms probably contribute because these quantitative abnormalities have high heritability. Antithrombin Deficiency Synthesized in the liver, antithrombin regulates coagulation by forming a 1 : 1 covalent complex with thrombin, factor Xa, and other activated clotting factors. Heparan sulfate or heparin accelerates the rate of antithrombin interaction with its target proteases. Inherited antithrombin deficiency is rare; it occurs in approximately 1 in 2000 people and can be due to decreased synthesis of a normal protein or production of a dysfunctional protein. A parallel reduction in the levels of antithrombin antigen and activity identifies deficiencies caused by decreased synthesis, whereas decreased antithrombin activity in the presence of normal antigen levels identifies dysfunctional forms of antithrombin. Comparison of antithrombin activity with or without added heparin identifies variants with impaired heparin-binding capacity. Acquired antithrombin deficiency results from decreased synthesis, increased consumption, or enhanced clearance. Decreased synthesis can occur in patients with severe hepatic disease, particularly cirrhosis, or in those given L-asparaginase. Increased activation of coagulation can result in antithrombin consumption in disorders such as extensive thrombosis, disseminated intravascular coagulation, severe sepsis, disseminated malignancy, or prolonged extracorporeal circulation. Heparin treatment can also reduce antithrombin levels up to 20% by enhancing the clearance of antithrombin. Severe antithrombin deficiency can develop in some patients with nephrotic syndrome because of loss of protein in urine. Protein C Deficiency Thrombin initiates the protein C pathway when it binds thrombomodulin on the endothelial cell surface (see Fig. Thrombin bound to thrombomodulin activates protein C approximately 1000-fold more 9 efficiently than free thrombin does. For efficient inactivation of these factors, activated protein C must bind to protein S, its cofactor. Approximately 1 in 200 adults has heterozygous protein C deficiency inherited in an autosomal dominant fashion, but most have no history of thrombosis. The variable phenotypic expression of hereditary protein C deficiency suggests the existence of other, yet unrecognized, modifying factors. In contrast to antithrombin deficiency, in which the homozygous state is associated with embryonic lethality, homozygous or doubly heterozygous protein C deficiency can occur.
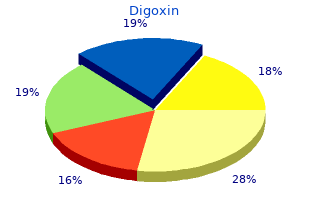
Usage: p.o.
Spinal nerve roots from C3 to L5 exit anterior to the zygapophysial joints through the neural foramina (Figs buy digoxin 0.25 mg low cost blood pressure scale uk. Each spinal nerve consists of a dorsal and a ventral root which come together to create a short purchase digoxin paypal prehypertension yahoo, unifed segment within the intervertebral neural foramen cheap 0.25 mg digoxin free shipping heart attack heart attack. This short, intraforaminal segment is the spinal nerve proper although it is sometimes imprecisely referred to as the spinal nerve root. The dorsal roots contain primarily afferent axons which originate from pseudounipolar neurons with cell bodies contained within the dorsal root ganglion. The Spinal Cord and Its Coverings These pseudounipolar neurons include A-delta and C fber pain afferents whose peripheral processes advance outward The relatively substantial dura mater surrounds the brain with the peripheral mixed nerves and whose central pro- and the spinal cord and contains the central nervous sys- cesses synapse with ascending pain afferents within the spi- tem within a single compartment flled with cerebrospinal nal cord dorsal horn as depicted schematically in Fig. Cephalad the spinal dura mater is bound to the edges Each dorsal root typically fans out into six or eight rootlets of the foramen magnum and to the posterior aspects of the which enter the cord in a vertical row. The spinal dura is then con- The frst cervical nerve is called the suboccipital nerve tiguous with the intracranial dura which continues intra- and is primarily motor with the dorsal primary ramus supply- cranially to surround the brain. The second cervical into the sacrum and ends with the flum terminale at nerve is a larger mixed sensory-motor nerve with a promi- approximately S1/S2 (Fig. The spinal fuid is cre- nent dorsal root ganglion which lies directly dorsal to the ated in the third, fourth, and lateral ventricles of the brain atlantoaxial joint. The medial branch of the dorsal primary by the actions of the highly vascular choroid plexuses. Other causes for chronic occipital pain may within the cranium associated with the cardiac cycle. There include injury or arthritis involving the atlanto-occipital, is a secondary slow circulation of spinal fuid throughout the atlantoaxial, and/or upper cervical zygapophysial joints. Cervical disc herniation may also cause pain referred into the Radioactive tracers injected into the lumbar intrathecal space occipital region. The Since there are seven cervical spinal levels and eight cer- spinal fuid is reabsorbed into the venous circulation through vical spinal nerves, the spinal nerve numbering convention is the arachnoid granulations which are located primarily different in the cervical region from that in the thoracic and within the superior sagittal sinus. The frst cervical foramen occurs at C2/ fuid is approximately 150 mL with 125 mL surrounding the C3 and transmits the C3 spinal nerve. C4 exits the C3/C4 foramen, and C7 exits the C6/C7 fora- The epidural space extends from the level of C1 down to men). Numbering changes at the C7/T1 foramen where the the sacral hiatus and encircles the spinal dura in a circumfer- C8 nerve exits since from T1/T2 and below, the numbering ential manner (Fig. The space is flled potential space between the closely apposed dura and arach- with fat, connective tissue, and a venous plexus. This space can bands may course through the epidural space, binding the sometimes be inadvertently entered with needles or catheters dura to the interior walls of the spinal canal. Nerve root flling not clearly identifed as in Anterior posterior view of lumbar myelogram demonstrating normal myelogram (c). Lateral demonstrating ventral deformities of the thecal sac at the L3/L4 and L4/ view of lumbar myelogram demonstrating ventral deformities (white L5 levels (d) (Adapted from Botwin [16] and Manchikanti and Singh arrows) of the thecal sac at the L3/L4 and L4/L5 levels (b). A contrast dye local anesthetic injected epidurally or intrathecally, and spread pattern that stops at the upper aspect of C1 is con- unintended subdural injection can sometimes account for sistent with an epidural location, whereas contrast that excessive sensory-motor block after epidural injection pro- extends above C1 is likely intrathecal (Fig. All rights reserved) 7 Anatomy of the Spine for the Interventionalist 85 Blood Supply to the Spinal Cord thoracic cord is most vulnerable to ischemia from hypoten- sion because it is most distant from the lower cervical and The spinal cord receives its blood supply from three longitu- upper lumbar anterior medullary feeding arteries. Since the number and position of segmental medullary The longitudinal arteries include a single anterior spinal spinal feeder arteries is variable and relatively unpredict- artery and two posterior spinal arteries. The anterior spinal able, great care must be taken with any injection into any artery is formed from paired branches which exit the bilat- intervertebral neuroforamen. The foramina most likely to eral vertebral arteries just prior to their anterior convergence contain these arteries are in the lower cervical, lower tho- to form the basilar artery (Fig. These paired branches racic, and upper lumbar regions of the spine, although any course caudally and unite in the anterior midline to form the intervertebral foramen may contain a feeding spinal artery single anterior spinal artery. These mid-thoracic region of the cord is considered to be the “vul- arteries typically anastomose with the anterior spinal arter- nerable zone” with respect to circulation and is most easily ies and provide direct routes for blood fow into the paren- damaged by severe hypotension. Any particulate matter (including rior spinal artery that penetrate the cord parenchyma are end particulate steroid) has the potential to occlude the distal arteries and do not anastomose further. There have which supply blood to the exiting spinal nerve roots at every been a number of cases of paralysis and death associated level. These segmental radicular arteries enter the spinal with inadvertent injection of particulate steroid into intrafo- canal through the neuroforamina to arborize around and pen- raminal segmental spinal feeding arteries during interven- etrate the parenchyma of the spinal nerve roots and supply tional pain procedures [9–13]. In the cervi- cal region, the segmental radicular arteries may originate from the vertebral arteries or less commonly from ascending Key Points or deep cervical arteries. In the thoracic region, the segmen- tal arteries originate from the posterior intercostal arteries 1. It is crucial for the spinal injectionist to have a detailed which branch directly from the aorta, and in the lumbar understanding of spinal anatomy. The spinal column is a complex structure consisting of In addition, the anterior spinal artery is reinforced at a multiple bones, ligaments, and intervertebral discs, number of levels by feeder arterial branches from various which are functionally integrated to facilitate upright arteries including lumbar arteries, intercostal arteries, and locomotion and to provide protection for the spinal cord. The image appearing on the fuoroscopic monitor is a mental anterior medullary arteries” and are important to the composite representation of the overlapping tissue den- spinal injectionist because they constitute a direct route for sities that lie between the x-ray tube and the image delivery of potentially damaging particulate medication into intensifer. The prototypical vertebra is composed of an anterior of eight anterior medullary feeder arteries (inclusive of all cylindrical block of bone called the vertebral body which spinal levels bilaterally), the largest of which is the great is connected to the posterior neural arch by the pedicles. Fluoroscopically, the pars interarticularis is represented total number of anterior medullary feeder arteries varies by the neck of the “Scotty dog,” and a pars defect appears from 2 to 17 in different individuals, with an average of three as a “collar” on the dog’s neck. The artery of Adamkiewicz typically in part to transmit weight from the upper body to the enters the cord on the left side (77% of specimens) anywhere lower extremities through the sacroiliac joints. The spinal cord begins within the skull, exits the fora- may be the main blood supply to the lower 2/3 of the spinal men magnum, and ends with the flum terminale at cord. In the cervical region, the largest anterior medullary approximately L1/L2, giving rise to 31 pairs of spinal arteries typically enter at C4/C5 or C5/C6 [8]. Schultz Posterior spinal arteries Anterior spinal artery Anterior segmental medullary artery Anterior radicular artery Posterior radicular artery Branch to vertebral body and dura mater Spinal branch Dorsal branch of posterior intercostal artery Posterior intercostal artery Paravertebral anastomoses Prevertebral anastomoses Thoracic (descending) aorta Section through thoracic level: anterosuperior view Right posterior spinal artery Sulcal (central) branches to right side of spinal cord Peripheral branches from pial plexus Posterior radicular artery Sulcal (central) branches to left side of spinal cord Anterior segmental Left posterior spinal artery medullary artery Pial arterial plexus Anterior and posterior radicular arteries Anterior spinal artery Posterior radicular artery Arterial distribution: schema Anterior segmental medullary artery Note: All spinal nerve roots have associated radicular or Pial arterial plexus segmental medullary arteries. Both types of arteries run along roots, but radicular arteries end before reaching anterior or posterior spinal arteries; larger segmental medullary arteries continue on to supply a segment of these arteries. All rights reserved) 7 Anatomy of the Spine for the Interventionalist 87 Crura of diaphragm Posterior longitudinal ligament Psoas Dura Pedicle Internal vertebral plexus of veins in extradural space Aorta Ligamenta flava Cauda equina Interspinous ligament Supraspinous ligament Quadratus lumborum Erector spinae Vein muscles Lumbar artery Intervertebral foramen Intervertebral disc Vertebra Skin Lamina Fig. Cervical transforaminal epidural injections are associ- vertebral bodies from C2 to the sacrum with a central ated with extremely high risk. In contrast, the arteries semiliquid nucleus pulposus surrounded by a circumfer- can be avoided in the majority of the patients with alter- ential annulus fbrosus. The spinal cord receives its blood supply from three lon- gitudinal arteries including a single anterior spinal artery Acknowledgments This book chapter is modifed and updated from a and two posterior spinal arteries and a variable number previous book chapter, “Spinal Anatomy for the Interventionalist” by David M. Anatomic dissection that demonstrates the References path of the C8 radicular artery (arrowheads) as it follows the inferior aspect of the C8 spinal nerve through the intervertebral foramen to join 1.
In victims of homicidal ligature strangulation cheap 0.25 mg digoxin with amex pulse pressure 60, hair is often found clutched in the hands buy digoxin from india pulse pressure journal. A control sample of the victim’s hair should be obtained for comparison generic 0.25 mg digoxin blood pressure chart download software, because the hair found in the hands almost invariably turns out to be that of the victim. Fingernail scrapings or cuttings (the latter are preferred) should be taken to look for tissue of the perpetrator under the nails. Unfortunately, unlike in fiction, such scrapings or cuttings have traditionally been of little help, with foreign tissue rarely identified. Manual Strangulation Manual strangulation is produced by pressure of the hand, forearm, or other limb against the neck, compressing the internal structures of the neck. The mechanism of death is occlusion of the blood vessels supplying blood to the Asphyxia 263 brain i. In the authors’ experience, it is the second most common method of homicidal asphyxia. In a study by DiMaio of 41 deaths caused by manual strangulation, females predominated, with the ratio of females to males 1. One cannot commit suicide by manual strangulation because, as soon as consciousness is lost, pressure is released and consciousness regained. Occasionally, it is claimed that the death of a healthy individual ascribed to manual strangulation is unintentional and caused by a vasovagal reaction (reflex cardiac death) brought on by touching, grasping, or striking the neck. The mech- anism of death in such a case would be an arrhythmia produced by stimu- lation of the carotid sinuses. The carotid sinus is a focal area of enlargement of the common carotid artery where it bifurcates into the external and inter- nal carotid arteries. Compression or stimulation of the carotid sinuses causes an increase in blood pressure in these sinuses with resultant slowing of the heart rate (bradycardia), dilatation of blood vessels (vasodilation), and a fall in blood pressure. Pressure on the common carotid artery below the sinuses reduces the blood pressure within the sinus by reducing the amount of blood flowing into it. This mimics hypotension or decreased blood supply from hemorrhage or shock, causing the heart to beat faster (tachycardia), the blood vessels to constrict (vasoconstriction), and a rise in blood pressure. This explains the fact that, while in most cases of manual strangulation there is bradycardia, vasodilation, and fall in blood pressure, in some cases, if the hands are lower down on the neck, there might instead be tachycardia, vasoconstriction, and a rise in blood pressure. In normal individuals, pressure on the carotid sinus causes minimal effects with a decrease in heart rate of less than six beats per minute and only a slight reduction in blood pressure (less than 10 mm Hg). In such individuals, there is slowing of the heart and cardiac arrhyth- mias ranging from ventricular arrhythmias to cardiac stand-still and hypotension. There are cases reported in which turning of the neck in varying positions or a high or tight collar has produced dizziness and fainting. Di Maio found petechiae present in the conjuctivae or the sclerae in 89% of his cases. The petechiae are most notice- able on the bulbar conjunctivae and conjunctival sac, the skin of the upper and lower eyelids, the bridge of the nose, the brows, and the cheeks. Con- junctival hemorrhages will be larger if the victim struggles and the assailant responds with increased pressure about the neck. The petechiae are caused by rupture of venules and capillaries secondary to increased intravascular pressure as a result of the obstructed venous return (the internal jugular veins) in conjunction with incomplete arterial obstruction, which permits the vertetbral arteries to continue supplying blood to the brain. The charac- teristic signs of asphyxia — cyanosis, and multiple petechiae — are most striking above the site of manual compression of the neck. If the body remains in the prone position for a prolonged length of time, such that it is approaching decomposition, postmortem petechiae can form in the distribution of the livor mortis. On occasion, in cases of manual strangulation, pulmonary edema is present, with foamy edema fluid visible in the nostrils. In most cases of manual strangulation, the assailant uses more force than is necessary to subdue and kill his victim. Typically, there are abrasions, contu- sions, and fingernail marks on the skin (Figures 8. Dissection of the throat usually reveals hemorrhage, often exten- sive, into the musculature. Depending on the age of the victim and the amount of force used, there might be fractures of the hyoid bone or thyroid cartilage. As age increases, so does calcification of these structures and the tendency to have fractures. Thus, these fractures are less common in individuals in their teens and late twenties than in individuals over 30 years of age. One must be careful not to mistake the cartilagenous separations between the greater horns of the hyoid and its body and the superior horns of the thyroid cartilage and thyroid plates for fractures. Hemorrhage must always be present at an alleged fracture site before it can be called an antemortem fracture. The incidence of fractures in manual strangulation is high if a careful dissection of the neck is conducted. In the 41 cases of manual strangulation studied by DiMaio, the incidence of fractures was 68. Of the 14 males, 10 had fractures of the hyoid, either alone (4 cases) or in combination with other structures (6); two had fractures limited to the thyroid cartilage; two to the cricoid cartilage. Bilateral fractures of superior horns of thyroid cartilage and fracture of cricoid cartilage. With unilateral fractures of the hyoid, fractures of the left side dominated 11 to 7. All the fractures of the thyroid cartilage involved the superior horns rather than the body of the thyroid. The latter fractures tend to be vertical and are usually caused by a blow to the thyroid cartilage. Because of its location high up in the neck, the hyoid bone is relatively safe from injury by direct blows unless the neck is arched. In direct blows to the neck, fractures of the hyoid are generally seen only in association with a fracture of the mandible. Whether the fractured ends of the hyoid bone are driven inward or outward is immaterial. The larynx, lying in front of the fourth through sixth cervical vertebrae, is protected in the midline only by skin and two layers of fascia. Thus, fractures of the body of the thyroid cartilage can be seen in blows to the neck. Lateral compression of the larynx, as might be expected in manual strangulation, causes fractures of the cornu (horns) of the thyroid. Fractures of the cricoid cartilage occur most frequently when the cartilage is compressed in an antero- posterior direction against the vertebral column. These fractures, which are usually vertical, might occur in the midline or laterally.