
Syracuse University. V. Gamal, MD: "Purchase Finast no RX - Discount Finast OTC".
Reported toxicities include elevations in liver enzymes purchase finast 5mg with amex hair loss experts, rash purchase cheap finast line hair loss 7 year cycle, and cheap finast american express hair loss xeloda, in a third of patients, transient ocular toxicity [50]. Posaconazole Posaconazole is a second-generation triazole approved for the treatment of oropharyngeal candidiasis, including infections refractory to itraconazole and/or fluconazole [51]. It is approved also as prophylaxis for invasive Aspergillus and Candida infections in patients older than 13 years who are at high risk of developing fungal infections, such as hematopoietic stem cell transplant recipients with graft-versus-host disease and neutropenic patients with hematologic malignancies [52,53]. Limited clinical experience suggests efficacy for the treatment of infections due to Zygomycetes and as salvage therapy for patients with invasive aspergillosis and coccidioidomycosis. Posaconazole currently is available only as an oral tablet or suspension and requires administration with food or a nutritional supplement to assure adequate bioavailability. Recommended therapy of oropharyngeal candidiasis is a loading dose of 200 mg (100 mg twice daily), followed by 100 mg daily for 13 days. Refractory oropharyngeal candidiasis may be treated with 400 mg twice daily, with the duration based on clinical response and the patient’s underlying disease. Experimental treatment of invasive fungal infections with posaconazole at 200 mg orally four times daily and maintenance therapy at 400 mg orally twice daily is based on pharmacokinetic data; however, package labeling does not include this indication. The most common adverse effects associated with the use of posaconazole include headache, fever, nausea, vomiting, and diarrhea. In a phase 3 clinical trial, isavuconazole demonstrated non-inferiority to voriconazole on the primary endpoint of all-cause mortality at day 42 for the treatment of adult patients with invasive aspergillosis or other filamentous fungi [54]. The overall safety profile for isavuconazole demonstrated similar rates of mortality and non-fatal adverse events as the comparator, voriconazole. Similar to posaconazole, dose adjustment is not required in the presence of renal and/or hepatic insufficiency. Caspofungin can be used for refractory cases of invasive aspergillosis in patients intolerant of voriconazole and amphotericin B. All these agents may be used to treat candidemia with similar success but with fewer side effects than amphotericin B [55]. Caspofungin is metabolized by the liver, and dose adjustment is required when it is given with other drugs that alter cytochrome P450 activity. Caspofungin is classified as pregnancy category C and should be used during pregnancy only if the potential benefit outweighs the potential fetal risk. Micafungin appears comparable to fluconazole as antifungal prophylaxis in patients undergoing hematopoietic stem-cell transplantation [56] and anidulafungin has been used in neutropenic children. Absence of antagonism in combination with other antifungal agents suggests that combination antifungal therapy warrants further study, particularly for severe aspergillosis and candidiasis [57]. It has activity against Gram-positive and Gram-negative bacteria, Nocardia spp, and Pneumocystis jiroveci (previously known as P. The dose for serious bacterial infections is 8 to 10 mg/kg/d (of the trimethoprim component), divided every 6 to 12 hours. Pyrimethamine–Sulfadiazine For the treatment of systemic and invasive (including encephalitis) toxoplasmosis in the compromised host, the alternate double-antifolate combination of pyrimethamine–sulfadiazine usually is used. Pyrimethamine is administered orally with a loading dose of 200 mg, then at 75 mg daily (with folinic acid 5 mg daily) together with sulfadiazine orally at 6 g daily in four divided doses. Nevertheless, antiviral therapy remains problematic and limited in scope as compared with antibacterial treatments. Administered as a prodrug, acyclovir requires phosphorylation to a monophosphate form by a virus- generated thymidine kinase and then to a triphosphate form by host cellular enzymes. After oral administration, absorption is slow and incomplete, with oral bioavailability of only 15% to 30%. In general, it is well tolerated, but thrombocytopenia and hemolytic-uremic syndrome have been reported in immunocompromised patients. Other side effects are similar to those of acyclovir and include encephalopathy, fevers, seizures, and rash. Acyclovir, or valacyclovir, is used prophylactically in patients who are undergoing bone marrow or solid organ transplantation. Ganciclovir and valganciclovir are cleared by the kidney and dosage adjustments must be made in patients with renal impairment, especially in light of the relationship between drug serum levels and myelosuppression. Nonrenal adverse effects include nausea, vomiting, anemia, seizures, and metabolic abnormalities (hyperphosphatemia and hypophosphatemia, hypercalcemia and hypocalcemia, hypokalemia, and hypomagnesemia). Anti-Influenza Agents Amantadine and rimantadine are oral antiviral compounds that inhibit influenza A, and zanamivir, oseltamivir, and peramivir are neuraminidase inhibitors that inhibit both influenza A and B viruses. If initiated within 48 hours of the onset of symptoms, all four agents may reduce the intensity of influenza infection in patients infected with susceptible viruses [45,64]. For patients who are immunocompromised or who have ongoing viral replication and progressive symptoms, therapy after 48 hours may also be beneficial, although supporting data are not available. American Thoracic S; Infectious Diseases Society of America: Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Paul M, Lador A, Grozinsky-Glasberg S, et al: Beta lactam antibiotic monotherapy versus beta lactam-aminoglycoside antibiotic combination therapy for sepsis. Charlier C, Hart E, Lefort A, et al: Fluconazole for the management of invasive candidiasis: where do we stand after 15 years? Nagappan V, Deresinski S: Reviews of anti-infective agents: posaconazole: a broad-spectrum triazole antifungal agent. Hiramatsu Y, Maeda Y, Fujii N, et al: Use of micafungin versus fluconazole for antifungal prophylaxis in neutropenic patients receiving hematopoietic stem cell transplantation. To assist in this challenge, as these diseases are discussed, key historical points and clinical clues will be emphasized. Family members may need to be interviewed if the patient is too ill to participate fully in the history. Key points of the exposure history include travel, employment, hobbies, and exposure to pets, wildlife, and livestock. This portion of the interview will yield better results if it is carried out in a slow-paced conversational manner, allowing the patient or family member to chat a bit. It is less focused than a standard social history and review of symptoms, owing to the heterogeneous nature of the exposures being sought. In assessing vital signs, one must evaluate hypothermia (temperature less than 36°C) in the same light as fever (temperature higher than 38°C). Laboratory studies should include a complete blood count with platelet and differential counts; prothrombin and partial thromboplastin times; electrolytes, including calcium and magnesium; blood glucose; renal and liver functions; two sets of blood cultures, urine for culture and urinalysis; and a chest radiograph. If a serious infection is under diagnostic consideration, the hematology laboratory should supplement the automated differential leukocyte count with a manual differential count by microscopic examination of the peripheral blood film. This may require a specific request from the physician, especially if the total leukocyte count falls within the normal range. It is a multisystem disease characterized by acute onset of high fever, hypotension, diffuse macular rash, severe myalgia, vomiting, diarrhea, headache, and nonfocal neurologic abnormalities. The primary focus of staphylococcal infection may be mucosal, typically vaginal, associated with tampon or diaphragm use, or a wound.
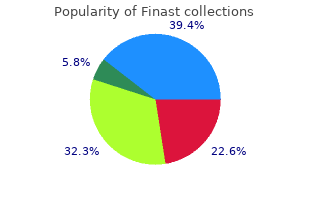
Examples are serial Papanicolaou (Pap) smears of response to anticancer treatment buy finast 5 mg overnight delivery lakme prevention shampoo hair loss. The 28 tubal ligation and reduced incidence of these (as well as 000 women in the screening arm underwent annual serous) cancers [11] order genuine finast on-line hair loss 19 year old male. Patients then received postal follow‐up present at tubal–mesothelial junctions [33] buy finast 5mg line hair loss disease alopecia. Patients were screened for six consecutive years and Screening and prophylactic followed up for 7 years from randomization. Final data were published in 2015, 4 years can clearly be made for screening women to try to iden- after the last patient was recruited in 2011. Interestingly, there was Surgical and Medical Management of Epithelial Ovarian Cancer 889 evidence of a statistical trend towards improved survival hysterectomies. Although the follow‐up ingly being offered as an alternative to tubal ligation for period has therefore been extended to confirm late sur- contraception in view of its cancer‐protecting effects. Endometrioid adenocarcinomas and clear urement) to women with known ovarian cancer predis- cell carcinomas are the next commonest histological posing mutations. Ovarian carcinosarcomas are epithelial tumours with sarcomatous differentiation but these are rarely encoun- Risk‐reducing surgery tered. There is evidence that clear cell and mucinous Prophylactic oophorectomy has been shown to reduce ovarian cancers are far less responsive to chemotherapy the incidence of subsequent ovarian and breast cancer than serous and endometrioid ovarian cancers. Borderline tumours are lactic bilateral salpingo‐oophorectomy is performed not regarded as cancers and in general have an excellent on completion of childbearing or at the age of 40 years prognosis. However, there are no clear guide- Patterns of spread of ovarian cancer lines in place and management of these patients var- ies widely. The new versus old staging is shown in bone health) is excessive and women should undergo Table 63. With the exception of malignant unilateral or disseminate along locoregional, lymphatic and blood‐ bilateral pleural effusion, and involvement of the umbili- borne routes. This is often accompanied by malig- familial ovarian cancers that have a very high (73%) inci- nant ascites and lymph node involvement is relatively dence of visceral metastatic disease [47]. Cytological diagnosis, such as from a sample Surgical management of newly diagnosed of ascites, is considered inadequate for definitive diagnosis. This timing of surgery, the value of surgery at relapse and how is a change from the 20% threshold previously defined by to optimize postoperative quality of life. Conventional imaging has not been shown to sensitivity of disease to platinum‐based chemotherapy. Non‐fertility‐sparing surgery consists of perito- with advanced disease with poor performance status or neal washings or cytology, ideally taken prior to manipu- where primary debulking surgery is predicted to be too lation of the tumour, bilateral salpingo‐oophorectomy, 892 Gynaecological Cancer hysterectomy, multiple peritoneal biopsies from the par- ing rates have significantly better survival. Positive nodes resection techniques such as extensive peritoneal strip- were detected in 22% of patients undergoing systematic ping, full‐thickness diaphragmatic resection, removal of lymphadenectomy compared with only 9% of patients bulky pelvic/para‐aortic lymph nodes, splenectomy and who underwent lymph node sampling (P= 0. However, risk of up to 11% of positive contralateral pelvic lymph the caveat was that, in this study, only approximately nodes in women with unilateral disease despite negative one‐third of the patient cohort were optimally cytore- ipsilateral nodes [71,72]. The median survival time for patients It is not yet fully clarified whether this association is with and without lymphadenectomy was 103 and 84 causal or whether resectable tumours are biologically months, respectively, and 5‐year survival rates were more chemosensitive (than those that are unresectable) 67. Future trials are in development that are fit, lacking in comorbidities (especially those exac- will be conducted in centres with established surgical erbated by the treatment or its supportive therapies) and quality to answer the question of timing and will address able to cope with combination chemotherapy. Palliative care specialist input may be or as weekly dose‐dense therapy (80 mg/m ). A similar question was then addressed in and community services within one framework. This raises the question of why intravenous chemotherapy beyond an expected median the benefit of dose‐dense paclitaxel was so much greater survival of this optimally debulked group of 4 years. However, intraperitoneal bevacizumab (Arm B1), the Japanese regimen with- chemotherapy was associated with enhanced toxicities, out bevacizumab (Arm B2) or the Japanese regimen with including neuropathy, gastrointestinal toxicity and myel- bevacizumab (Arm B3). Interestingly, in those who did tions of intraperitoneal catheters and fear of excessive not receive bevacizumab, weekly paclitaxel was asso- toxicity [95]. However, the study accrual difficulties and concluded that, of three different was not truly randomized as the study patients self‐ regimens intraperitoneal carboplatin given with intrave- selected bevacizumab. The intra- Intraperitoneal chemotherapy peritoneal treatment was well tolerated with low Ovarian cancer is principally a disease of locoregional complication rates. Importantly, this study demonstrated peritoneal dissemination within the abdominal cavity. The common factor is that all have intraperitoneal paclitaxel with intravenous bevacizumab Surgical and Medical Management of Epithelial Ovarian Cancer 895 (Arm 3). This followed a number of clinical tri- whether upfront debulking or neoadjuvant chemother- als in heavily pretreated relapsed ovarian cancer patients apy is preferred. Palliation and optimization of quality of life 896 Gynaecological Cancer are important considerations in this clinical scenario, improvement in survival for carboplatin and paclitaxel including careful symptom management and the judi- as front‐line chemotherapy in advanced ovarian cancer. Tumour that has ommended for patients relapsing more than 12 months relapsed more than 12 months following prior treat- from last chemotherapy [106]. Other strategies include Platinum‐sensitive recurrence replacing platinum with an alternative cytotoxic such as Platinum‐sensitive recurrence has several definitions. Although toxicity of the combination biological predictors were the main determinants of sub- was higher than in those receiving olaparib alone, this sequent response, with the treatment‐free interval cor- study gave an indication that the spectrum of activity of relating closely with tumour size. The recently reported benefit was conducted in patients relapsing more than 6 months of niraparib maintenance (see above) in those with a after last chemotherapy. Surgical and Medical Management of Epithelial Ovarian Cancer 897 Platinum‐resistant recurrence longer survival compared with surgery leaving any post- There are various definitions of platinum‐resistant operative residual disease (median 45. These findings recurrent disease requiring treatment within 6 months challenge clinicians to accurately identify those patients of completing last chemotherapy. For this to benefit (or fail to benefit) equally from all convention- reason, based on a multivariate model, three clinical ally dosed and scheduled chemotherapeutic agents. Participating number of novel approaches, including using immuno- centres prospectively enrolled patients with platinum‐ therapy (discussed below). While tion was 76%, thus confirming the validity of this score many supporters of surgical cytoreduction at relapse regarding positive prediction of complete resectability in advocate that complete tumour resection may result more than two‐thirds of patients [117]. The situation is even vaguer in the tertiary bosis rate, while 52% of the patients required postopera- setting and beyond. There are future plans to combine results significance for complete tumour resection, whilst from both trials to achieve a larger cohort and more residual tumour at secondary and tertiary surgery, robust survival data. Despite these encouraging retrospective data it is still not clear if Management of bowel obstruction the surgery itself is influencing survival or whether oper- in the palliative setting ability is just a surrogate marker of more ‘favourable’ tumour biology and therefore a better overall prognosis. The most frequent tumour dissemi- proximal ileostomy or jejunostomy since, due to peri- nation site was the pelvis (73%). Most importantly, common institutional and physical resources and consideration of clinicopathological characteristics such as tumour stage, total parenteral nutrition. Benefits should be very carefully stitute a selection bias since patients who are fit enough balanced with risks for each individual patient. Factors to tolerate chemotherapy following radical surgery may such as comorbidities, baseline quality of life, previ- have more favourable survival rates than those for whom ous response to chemotherapy, treatment intervals and chemotherapy was contraindicated. The most common complications were infection/ bowel obstruction, a single stent or stoma formation is sepsis (13%) and re‐laparotomy (4.
Purchase finast 5mg without prescription. Vatika Hair Oil- Does it Stop Hair fall Hair Loss and make Hair Grow Longer and Faster??.

This is more likely to occur in patients on chronic peritoneal dialysis cheap 5mg finast visa hair loss vs shedding, in whom dialysis is performed every day buy finast no prescription hair loss cure 2014 histogen. Clinical Manifestations Most individuals with mild hypokalemia exhibit no symptoms referable + to the low plasma K concentration purchase finast with a mastercard hair loss in men 1920. The major disturbances seen with + more severe K deficiency are changes in cardiovascular, neuromuscular, and renal function. Cardiac toxicity may be manifested by serious arrhythmias because of hyperpolarization of the myocardial cell membrane, leading to a prolonged refractory period and increased susceptibility to reentrant arrhythmias. Hyperpolarization also slows down nerve conduction and muscle contractions, which may contribute to symptoms such as muscle weakness, cramps, and paresthesias, although these are usually not + observed until the plasma K concentration is less than 2. Increased thirst results from direct stimulation of the hypothalamic thirst center as well as from an appropriate response to polyuria. The surreptitious vomiting of bulimia or the diarrhea of laxative abuse may be omitted from the patient’s history. Measurement of blood pressure and urinary potassium excretion and assessment of acid–base balance are often helpful in such cases. In the presence of potassium depletion, a healthy subject should lower urinary potassium excretion to less than 30 mEq per day; values above this level reflect at least a contribution from urinary potassium wasting. Random measurement of the urine potassium concentration can be used but is less accurate than a 24-hour collection. Extrarenal losses probably are present if the urine potassium concentration is less than 15 mEq per L, unless the patient is markedly polyuric. Once urinary potassium excretion is measured, the following diagnostic possibilities should be considered in the patient with hypokalemia of uncertain origin: Metabolic acidosis with a low rate of renal potassium excretion is suggestive of lower gastrointestinal losses as a result of diarrhea, laxative abuse, or a villous adenoma. A salt-wasting nephropathy can produce similar findings, with the associated renal insufficiency responsible for the acidemia. Metabolic alkalosis with a low rate of urinary potassium excretion may be as a result of surreptitious vomiting or diuretic use if the urinary collection is obtained several days after the vomiting or diuretic use has been halted. Metabolic alkalosis with renal potassium wasting and a normal blood pressure most often results from ongoing vomiting, diuretic use, or, far less commonly, from Bartter’s syndrome or Gitelman’s syndrome. A low urine chloride concentration helps to distinguish the hypokalemia of vomiting from that of diuretics or Bartter’s syndrome and Gitelman’s syndrome. Metabolic alkalosis with potassium wasting and hypertension suggests surreptitious diuretic therapy in patients with underlying hypertension, renovascular disease, or one of the causes of primary mineralocorticoid excess. The possible presence of primary mineralocorticoid excess (with aldosterone and, to a lesser degree, deoxycorticosterone being the major endogenous mineralocorticoids) should be suspected in any patient with hypertension and unexplained hypokalemia and metabolic alkalosis. The active compound in licorice, glycyrrhizic acid, inhibits renal 11β-hydroxysteroid dehydrogenase activity. The result is cortisol-induced stimulation of the mineralocorticoid receptor, leading to renal sodium retention and potassium loss. It is important to be aware that hypokalemia is characteristic of malignant hypertension, which is a high renin, high aldosterone state, regardless of the underlying cause. Treatment Although hypokalemia can be transiently induced by the entry of potassium into the cells, most cases are caused by gastrointestinal or urinary losses. Optimal therapy depends on the severity of the potassium deficit; somewhat different considerations are required to minimize continued urinary losses caused by diuretic therapy or, less often, to one of the causes of primary hyperaldosteronism. The total potassium deficit can only be approximated because there is no strict correlation between the plasma potassium concentration and total body potassium stores. In general, the loss of 200 to 400 mEq of potassium is required to lower the plasma potassium concentration from 4 to 3 mEq per L; the loss of an additional 200 to 400 mEq lowers the plasma potassium concentration to approximately 2 mEq per L. Continued potassium losses do not as readily worsen the degree of hypokalemia because of the release of potassium from the intracellular pool. These estimates assume a normal distribution of potassium between the cells and the extracellular fluid. The most common setting in which this does not apply is diabetic ketoacidosis, a disorder in which hyperosmolality and insulin deficiency favor the movement of potassium out of the cells. As a result, patients with this disorder may have a normal or even elevated plasma potassium concentration at presentation, despite having incurred a marked potassium deficit owing to urinary or gastrointestinal losses, or both. Potassium supplementation for these patients should begin once the plasma potassium concentration is 4. First, potassium chloride more rapidly raises the plasma potassium concentration than does potassium bicarbonate or potassium citrate, the citrate being rapidly metabolized to bicarbonate. The retention of chloride in the extracellular fluid, obligated by the need to maintain electroneutrality, limits the initial entry of potassium into the cells, thereby maximizing the rise in the plasma potassium concentration. For example, with diuretic therapy, vomiting, and hyperaldosteronism, hydrogen loss accompanies that of potassium. Potassium must be given with chloride to such patients if both the hypokalemia and the alkalosis are to be corrected optimally (see Chapter 198). Oral potassium chloride can be given in crystalline form (salt substitutes), as a liquid, or in a slow-release tablet or capsule. Salt substitutes contain 50 to 65 mEq per level teaspoon; they may be the ideal form of oral therapy, because they are safe, well tolerated, and much cheaper than the other preparations. Potassium chloride solutions, on the other hand, are often unpalatable, and the slow-release preparations can, in rare cases, cause ulcerative or stenotic lesions in the gastrointestinal tract as a result of the local accumulation of high concentrations of potassium. Merely increasing the intake of potassium-rich foods such as oranges and bananas is generally less effective in the absence of renal insufficiency. These foods contain phosphate and citrate rather than chloride and are, therefore, less likely to correct the hypokalemia and metabolic alkalosis. Potassium chloride can be given intravenously to patients who are unable to eat or who have severe hypokalemia. It is usually added to a solution in which the concentration should generally not exceed 40 mEq of potassium per L because higher concentrations can lead to pain and sclerosis of a peripheral vein. A saline solution is preferred to a dextrose solution for initial therapy because the administration of dextrose can lead to a transient 0. Treatment in this setting is directed toward replacing the lost potassium, usually beginning with 40 to 80 mEq of potassium chloride per day, and toward treating the disorder responsible for the loss of potassium. Potassium replacement alone may be insufficient to treat patients with ongoing urinary losses caused by chronic diuretic therapy, tubular dysfunction, or primary hyperaldosteronism. Potassium-sparing diuretics such as amiloride, triamterene, the aldosterone antagonists, spironolactone, and eplerenone are generally more effective than other agents, because they limit further urinary losses of both potassium and magnesium. It is frequently underappreciated, however, that, in the presence of high levels of aldosterone, greater-than-usual doses (up to 20 to 40 mg of amiloride and 150 to 300 mg of spironolactone) may be required to block potassium secretion. The combination of a potassium- sparing diuretic with potassium supplements should be used only with careful monitoring to prevent possible overcorrection with development of hyperkalemia and should be avoided in most patients with renal insufficiency. In light of these fluxes, careful monitoring is required, and more potassium should be given as necessary. Some patients with severe hypokalemia must be treated intravenously because of medical instability or an inability to take medication orally. There are two potential limitations to intravenous therapy: A maximum concentration of 50 to 60 mEq per L can be administered via a peripheral vein without irritation, and, because saline solutions are preferable, volume overload is a potential risk in susceptible subjects. Because these patients are also quite volume depleted, the addition of 40 to 60 mEq of potassium chloride to each liter of half- isotonic saline can supply large quantities of potassium with less risk of pulmonary congestion.
More than just survival benefit generic finast 5mg with mastercard hair loss blog, a successful transplantation can free a patient from the demands of dialysis and provide a higher quality of life at a fraction of the overall cost compared to those not transplanted [3] purchase 5 mg finast with amex hair loss in men 1 syndrome. The half- life graft survival is projected for deceased donor recipients to be 10 years; for living-related donor recipients buy 5mg finast overnight delivery hair loss 2015, almost 18 years [4,5]. Enthusiasm for kidney transplantation is undoubtedly fueled by these promising outcomes; however, a donor shortage crisis remains. These protracted waiting times subject our patients to a great deal of harm from the ill effects of uremia and dialysis. Critical care providers, therefore, are facing a cohort of patients awaiting kidney transplantation who are sick and getting sicker. This chapter discusses the salient points of critical care to optimize outcomes after kidney transplantation. It is therefore imperative that the pretransplant evaluation should be exhaustive (covering cardiovascular, gastrointestinal, pulmonary, neurologic, genitourinary, and infection disease concerns). The goal is not only that the patient should survive the operation and hospitalization, but also survive in the long term so that there is a realization of the potential graft life of the donor allograft. The cardiovascular examination is the most important because cardiac events constitute the most common cause of death in the perioperative and postoperative periods [7]. Ironically, our preoperative screening with noninvasive cardiac stress testing is notoriously unreliable. In a meta- analysis, the sensitivity of the pretransplant cardiac perfusion study for myocardial infarction was only 0. The onus remains on the transplant clinician to be highly suspicious of potential cardiac morbidity, even in younger patients with prolonged renal failure. Abnormalities detected by stress testing require coronary angiography to investigate the need for coronary stenting or even coronary artery bypass. It may also be reasonable to perform coronary angiography on high-risk patients with significant comorbidities or a pronounced history of cardiac problems with unremarkable stress testing. Recurrent urinary tract infections or bladder dysfunction requires urodynamic testing and urology consultation. Abnormal results require hematology consultation and a plan for therapeutic measures in the perioperative period. In addition to electrolyte screening, a complete history and physical examination, electrocardiogram, chest X-ray, and laboratory examination should be performed just prior to the operation to uncover any possible health derangements since the last physician visit. Intraoperative Care the degree of invasive monitoring during the operation should reflect the extent of the recipient’s comorbidities. Central venous catheters are commonly introduced to guide intraoperative and postoperative fluid management. Continuous arterial blood pressure monitoring is also quite common and facilitates blood pressure management during the case. It is justified when recipients have significant cardiac dysfunction, valvular abnormalities, or significant pulmonary artery hypertension. A 20-F three-way Foley catheter is useful to inflate the bladder with saline that greatly facilitates the ureteroneocystostomy. After completion of this anastomosis, urine output is checked frequently to guide fluid resuscitation. Optimizing the chance of immediate graft function requires careful communication and coordination between anesthesia and surgical teams. Most patients, however, can receive appropriate care on a solid-organ transplant ward provided there is mechanism for proper fluid resuscitation. This can be challenging, with the voluminous urine output often encountered with immediate graft function. The basis of the resuscitation is the equivalent replacement of urine output milliliter for milliliter, which is measured hourly. After 24 hours, the fluid replacements are converted to a continuous rate between 100 and 150 mL per hour based on the recipient weight and kidney function. Serial blood counts, coagulation profiles, and chemistries should be obtained in the postoperative period. Electrolyte abnormalities, especially hyperkalemia, hypokalemia, hypomagnesaemia, and hypocalcaemia are common and should be corrected. Serial troponins should be obtained to exclude myocardial ischemia with select recipients with significant cardiac comorbidity. Kidney transplant recipients are prone to complications owing to their significant comorbidities, intense immunosuppression, and variable graft function. It is estimated that between 15% and 30% of high-risk transplant candidates will require specific critical care. Diuresis on its own may be a result of the urine produced by the recipient’s native kidneys or the residual effect of diuretics infused during the operation. Intensivists must be aware that ultrasound can rule out surgical complications that require immediate therapeutic maneuvers to salvage the graft including clearing of arterial or venous thromboses. Most importantly, surgical complications need to be ruled out, most notably, thrombosis with a Doppler ultrasound. Acute Rejection Acute rejection in kidney transplantation is of great significance, but a comprehensive review is beyond the scope of this chapter. There are two types of acute rejection, cellular rejection and antibody-mediated rejection; both can diminish graft function and survival [16]. At present, this diagnosis is secured with a kidney biopsy, although there are efforts underway for noninvasive diagnostics. After vascular thrombosis and urologic complications are ruled out, the next step is often a biopsy to rule out rejection. Acute cellular rejection, which is a lymphocytic attack against donor tissue, is most often treated with a course of steroids or thymoglobulin. In antibody-mediated rejection, preformed or de novo alloantibodies target capillary endothelium and by activating the complement system can result in rapid destruction of the allograft. It may be recurrent or de novo, with the patient’s calcineurin inhibitor being a well-known causative agent [17]. Surgical Complications Leading to Early Graft Dysfunction Hemorrhage after surgery is always a possibility but is rare in kidney transplantation because the surgical field is confined to the retroperitoneal space, so bleeding usually tamponades. Bleeding is suspected if the patient is tachycardic, hypotensive, oliguric, and requiring blood transfusions. Subscapular bleeding in the allograft is an entirely different matter, as it can lead to compression and quick deterioration of allograft function. If this is recognized on Doppler ultrasound with evidence of compression, immediate reexploration is imperative to release the hematoma. Arterial thrombosis is a devastating complication in kidney transplantation, as the renal arteries are end arteries without collateralization. Therefore, arterial thrombosis almost invariably results in graft loss; however, fortunately it is rare (0.