
Harding University. E. Dawson, MD: "Order cheap Azithromycin - Safe online Azithromycin no RX".
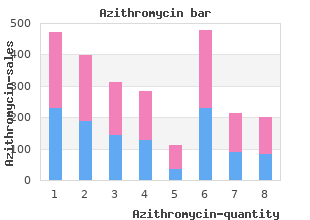
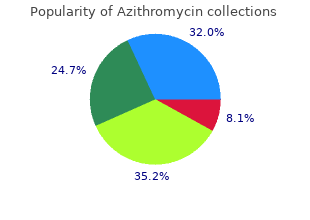
From June 1997 to December 1997 azithromycin 250mg amex virus 20 furaffinity, total of (58) gastroscopic biopsy were taken and examined generic azithromycin 500 mg line antibiotics for acne while nursing, including (8) of gastric adenocarcinoma cases buy 100 mg azithromycin amex varicella zoster virus. Comprising changes were chronic superficial gastritis 19 (38%), chronic atrophic gastritis 20 (40%), chronic gastritis with aberrant pancreatic rest 5 (10%), and chronic regenerative gastritis 6 (12%) respectively. They were pseudocysts of pancreas (14 cases), pancreatic phlegmon (14 cases), and pancreatic abscess (8 cases). Overall mortality rate of inflammatory pancreatic masses following acute pancreatitis was 19. Sex difference, serum amylase, urinary amylase and serum calcium could not be used as prognostic factors in these cases. However, when positive factors was 3 or more than 3, mortality rate became increased, along with increased number of positive factors. Serum amylase and urinary amylase levels were raised above normal in majority of cases but not that much as in early phase of acute pancreatitis. Means and standard deviations for serum amylase and urinary amylase levels were 544. Serum and urinary amylase levels in those cases remained high in blood longer than those of uncomplicated acute pancreatitis. Six cases underwent trangastric cystogastrostomy and no mortality as well as no recurrences were encountered. Seven responded well to non- operative treatment and achieved spontaneous regression. All of the spontaneous resolution started between two to six weeks from the onset of appearance of mass. Resolutions occured within 2 to 9 weeks after onset of attack of acute pancreatitis (mean=4. Anthropometric measurements were made every three months and growth rates were calculated. With the discovery of Helicobacter pylori, this organism has been shown to be responsible for several abnormalities of gastric secretion in duodenal ulcer. The presence of H pylori infection was confirmed and reassessed after infection eradication regime by the 20-minute 14carbon urea breath test. Eradication of organisms was revealed by significantly lower 14carbon-excretion at 20-minute breath sample. The latter was also measured by conventional titration method in H pylori infected duodenal ulcer patients. The twenty-four hour intragastric acidity and acid secretory response to pentagastrin in both the apparently healthy subjects and the H pylori infected duodenal ulcer 105 Bibliography of Research Findings on Gastrointestinal Diseases in Myanmar patients were high compared with reference values. A comparable trend of acid secretory response to pentagastrin was seen in both ambulatory continuous twenty-four hour pH monitoring method and the conventional titration method. High intragastric acidity in H pylori infected duodenal ulcer patient, persisted for one and a half months alter infection eradication regime. Bleeding oesophageal varices (22%) were more common than bleeding duodenal ulcer (17%). Ten patients (17%) with endoscopically proved duodenal ulcer were bleeding from another site and 28% of all patients had more than one lesion. This fact, and inability to detect the surface lesions limits the value of acute barium radiology, which was performed in 32 patients. Accurate diagnosis will help us in better understanding of individual lesion and more rational management of patients. Herewith we report the association of Helicobacter pylori in 49 Myanmar patients presenting with dyspepsia. Of 49 specimens, 3 were histologically normal and 46 showed histologic evidence of gastritis. Histologic evidence of Helicobacter pylori were demonstrated in 35 patients (76%). This preliminary but new study in Myanmar delineated the strong association between Helicobacter pylori and gastritis/peptic ulceration similar to other investigations. The three commonest causes were bleeding from acute erosive gastritis (32%), duodenal ulcer (22. Rare causes of upper gastrointestinal bleeding such as Mallory- Weiss tear (1 patient), bleeding from carcinoma stomach (2 patients), hepatocellular carcinoma with bleeding oesophageal varices (2 patients), haemobilia due to haemangioma left lobe of liver (1 patient) 106 Bibliography of Research Findings on Gastrointestinal Diseases in Myanmar were included in th study. All of them are clinically diagnosed as acute gastric erosion to whom endoscopy was done rather late. Compared to other 4 studies, the incidence of cases and endoscopic accuracy of this study were not much differed. Both are consistently sensitive to gentamycin, furoxone and norfloxacin but resistance to ampicillin, chloramphenicol and tetracycline. Gentamicin and furoxone were employed in 40 cases and average time for a clinical response was 4 days whereas with norfloxacin the symptoms stopped 2 days after employing the drug. Norfloxacin, a new quinolone antibiotic, is effective in drug resistant shigellosis and it also cuts down the duration of symptoms. Frequency distribution of cases, radiological findings and radiological diagnosis are discussed. Usefulness specificity and sensitivity of some importance radiological signs and radiological diagnosis seen on 2 films study are presented. The duration of illness before attending the hospital was found to be one to seven days. The frequency of motion among dysentery cases were found to be from 16 to 20 times per day. The initial safety record of this procedure has continued unblemished and it remains the safest operation in treating duodenal ulcer disease. Position of appendix was also studied on 21 barium Enema x-ray films and records of 32 cases of acute appendicitis from surgical unit of North Okkalapa General Hospital. Rectocaecal appendix were also observed and more than 90% of retrocaecal appendix were associated with ileal attachments. Half of the total numbers of appendicdes studied were provided with triangular mesoappendix which extended to the tip and one third of the cases lacked mesentry. The arterial supply to the appendix was studied on 78 cases by (a) plain gross dissection and after injection the ileocolicartery with plastic latex; (b) histological study after injecting the ileocolic artery with 1% trypan blue solution and (c) radiological examination after aqueous dionosil injection. Six trypan blue injected specimens were studied with Van Gieson s stain to study the intramutal arterial pttern. It was observed that the appendicular artery arose from six sources and most coomonly from ileocolic artery- 44. Anastomotic connection between the primary branches and between the appendicular artery and posterior caecal artery was lso identified. Two arterial plexus were found within the subserosa and submucosa layer of appendix. Correlation betweenthe presence of mesoappendix and position and position, arterial anastomosis and incidence of acute appendicitis were also discussed. Rectal swabs were also taken and investigated for culture and sensitivity at the Microbiology Department, Institute of Medicine I, Yangon.
Asthma diagnosed after September 11 buy discount azithromycin online virus infection, 2001 among rescue and recovery workers: findings from the World Trade Center registry buy azithromycin 250mg cheap bacteria zombie plants. Obstructive Airways Disease with Air- trapping among Firefighters Exposed to World Trade Center Dust buy discount azithromycin 250 mg line antibiotic resistance coalition. World Trade Center Sarcoid-Like Granulomatous Pulmonary Disease in New York City Fire Department Rescue Workers. Acute eosinophilic pneumonia in a New-York city firefighter exposed to World Trade center dust. World Trade Center dyspnea: bronchioloitis obliterans with functional improvement: case report. Biomonitoring of chemical exposure among New York City firefighters responding to the World Trade Center fire and collapse. American College of Gastroenterology: Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. They are usually performed in a lab or in a doctor s office and can be used to diagnose, assess severity and progression, and guide treatment of pulmonary diseases. Most pulmonary function measurements are routinely expressed as a percent predicted of normal so that the patient can see how they are doing compared to the population. Since pulmonary function measurements are known to be lower in shorter, older or female subjects, the percent predicted normal value automatically adjusts for age, height and gender. While obesity also has a direct effect in lowering pulmonary function measurements by placing a greater stress on the lungs, heart and skeletal muscles, the impact of obesity is not adjusted for automatically in the percent predicted equations. Therefore, if your values are low and you have central obesity (chest and/or abdomen) your values would likely be higher if you lost weight. As with the Olympics, the best effort counts and not the number of efforts required to produce that best effort. Simply, the patient blows as hard and fast as they can into a tube that measures the highest (or peak ) flow rate. The peak flow measurement occurs very early in expiration, when the flow rates are effort dependent. It is important to take a full breath in and blow out as hard as you can but after the first few seconds you don t have to blow out any further. Peak flow measurements are helpful in monitoring the status of chronic asthma, assessing the severity of acute exacerbations, evaluating therapy, and evaluating temporal (time-related or seasonal-related) relationships to triggers (ex. An asthma action plan can be written with instructions of what to do if the peak fow falls into these zones. Of note, falls in peak flow can occur even before symptoms worsen, making this a tool which potentially can lessen the severity of an exacerbation if the results are acted upon early on. Disadvantages of this test are that the results are not always reproducible and are effort dependent. A peak flow measure- ment does not obviate the need for spirometry to make the diagnosis of asthma. Spirometry Spirometry measures how much and how fast air moves in and out of the lungs. Spirometry, therefore, provides more data than a peak flow measurement and allows for a more accurate and reproducible measurement of asthma control. A typical study involves repeating the maneuver at least three times and the best of the three trials is accepted. Individual results are compared to normal values (predicted values) which are defined by a healthy population, adjusted for age, height and gender, and are expressed as a percentage of the predicted value. In healthy adults, spirometry results are normally distributed, meaning that 95% of test results in healthy adults will be between 80% - 120% of a predicted value. Perhaps more useful, however, is whether there is a rise or fall in these values in an individual patient over time. Because there are day-to-day variations in breathing capacity, a decline that is 15% or greater from your typical past recordings should be further evaluated by a physician. In obstructive lung diseases (such as asthma, emphysema and chronic bronchitis), the total amount of air that gets exhaled is normal or close to normal, but it takes more time for it to come out due to air flow limitation. For this reason, bronchodilator tests and full lung volumes (discussed later in this chapter) are necessary to distinguish obstructive from a restrictive abnormality. Flow Volume Loop The flow volume loop is a graph plotting forced expiratory and inspiratory flow against volume, and may reveal characteristic patterns associated with certain pulmonary diseases. The latter might be due to vocal cord abnormalities or obstruction in the upper trachea or larynx (voice box). In patients with obstructive lung disease, the expiratory curve is curvilinear or scooped in appearance, due to a reduction in flow as the volume of the lung decreases, which occurs as the patient exhales. Upper airway lesions alter inspiratory flow and will show as a flattening of the inspiratory loop. This can occur in patients with tracheal stenosis (scar in the wind pipe), which may occur after severe upper airway burns, prolonged intubation and mechanical ventilation. When the smooth muscle contracts, the diameter of the airways is reduced, resulting in a decrease in airflow. Certain inflammatory lung conditions, such as asthma or reactive airway disease (both discussed in later chapters), are characterized by hyperreactive (irritable/twitchy/spasmodic) airways, whereby certain triggers (ex. This relieves the airflow obstruction and can be demonstrated by repeating the spirometry after the bronchodilator is administered and waiting 10 minutes. Recall, spirometry only measures the amount of air entering or leaving the lungs and even after fully breathing out we always have some air left in our lungs. Therefore, in order to know the total amount of air in the lungs, one needs to know how much air is left in the lung after a complete exhale, or the residual volume. Residual volume can only be measured indirectly by gas dilution methods or body plethysmography. When airway obstruction is present, a slow vital capacity measurement may be more reflective of the true value. There are three methods to determine lung volumes: spirometry, the gas dilution technique and body plethysmography (also known as a body box). Spirometry has been discussed earlier and is limited by the inability to measure residual volume and therefore total lung capacity and functional residual capacity, because both contain the residual volume as part of their capacity. The other two techniques allow for the measurement or calculation of all lung volumes. By adding the residual volume to the vital capacity, total lung capacity can then be calculated. Typically, labs using the gas dilution technique utilize either the closed circuit helium (He) method or an open circuit nitrogen (N2) method. The starting volume of gas containing the helium is known and the amount of helium in the lungs at the start is zero. Since helium is inert, it does not diffuse across the alveolar- capillary membrane, and the gas equilibrates throughout the entire system. After the patient breathes normally for up to 10 minutes, equilibration usually occurs, and the amount of helium in the system is again measured. The open circuit nitrogen method is based on a similar principle of the helium technique, except here the expired concentration of nitrogen normally present in the lungs is now measured.
Discount azithromycin online master card. Fighting Antimicrobial Resistance!!!.
Edition six has 15 new chapters order azithromycin canada antibiotic zithromax, and the classic Drug Allergy chapter originated by Richard DeSwarte has been divided into three parts buy cheap azithromycin line antibiotics for sinus infection cephalexin. The new chapters covering radiologic findings of the sinuses and lungs safe 500mg azithromycin antibiotic resistance quorum sensing, role of rhinoscopy and surgery for chronic sinusitis, and work-up for immunodeficiency reflect the broadened base of knowledge required for the practice of Allergy-Immunology. In that asthma is now recognized as of one the most complicated disorders a physicians must treat, five new chapters were prepared to cover medications for asthma, inhaler devices and delivery systems, and novel approaches to treatment. There are shortages of specialists in Allergy-Immunology in practice and even more so in academic medical centers. We hope this textbook assists physicians to provide better care for their patients, inspires medical students and residents to pursue training in Allergy-Immunology, and assists investigators in advancing our knowledge. We are grateful to the authors for their superb chapters, each of which has been approved by us, should there be any oversights. We could not have completed this textbook without the love and support from our families who give us the time to continue in the Northwestern University Allergy-Immunology tradition that is now over 40 years old! Harris and Margaret Mateja Wieckert, our trainees and graduates, and our patients, from whom we can always learn. Assistant Professor of Clinical Medicine Department of Psychiatry Northwestern University Medical School Chicago, Illinois Andrea J. Instructor of Pediatrics (Allergy/Immunology) and Medicine Medical College of Wisconsin Milwaukee, Wisconsin Melvin Berger, M. Professor Departments of Pediatrics and Pathology Case Western Reserve University Chief Department of Pediatrics Rainbow, Babies and Children s Hospital University Hospitals Health System Cleveland, Ohio David I. Professor of Medicine Department of Immunology University of Cincinnati College of Medicine Cincinnati, Ohio Jonathan A. Associate Professor Department of Internal Medicine University of Cincinnati Cincinnati, Ohio Michael S. Clinical Professor Departments of Pediatrics and Medicine University of Tennessee, Memphis Department of Pediatrics Le Bonheur Children s Medical Center Memphis, Tennessee Bernard H. Clinical Professor Department of Medicine University of Mississippi Medical Center Jackson, Mississippi G. Department of Medicine University of Wisconsin Department of Medicine University of Wisconsin Hospitals and Clinics Madison, Wisconsin Robert K. Professor Department of Medicine University of Wisconsin-Madison Chief Department of Allergy William. Chief Resident Department of Otolaryngology Head & Neck Surgery Northwestern Memorial Hospital Northwestern University Chicago, Illinois David B. Assistant Professor Department of Otolaryngology Head & Neck Surgery Northwestern University Medical School Chicago, Illinois Thomas Corbridge, M. Associate Professor Department of Medicine Northwestern University Medical School Director Medical Intensive Care Unit Northwestern Memorial Hospital Chicago, Illinois Anne M. Assistant Professor Department of Medicine Division of Allergy-Immunology Northwestern University Medical School Chicago, Illinois Jordan N. Professor and Chief Department of Medicine Division of Allergy-Immunology Milwaukee County Medical Complex Milwaukee, Wisconsin Leslie C. Professor of Medicine Department of Medicine Vice Chief, Division of Allergy-Immunology Director, Ernest S. Bazley Asthma and Allergic Diseases Center Northwestern University Medical School Chicago, Illinois Thomas H. Associate Professor Department of Radiology Northwestern Memorial Hospital Northwestern University Medical School Chicago, Illinois Paul A. Professor of Medicine Department of Medicine Associate Chief, Education and Clinical Affairs Division of Allergy-Immunology Northwestern University Medical School Chicago, Illinois Kathleen E. Senior Life Sciences Researcher Department of Medicine Division of Allergy-Immunology Northwestern University Medical School Chicago, Illinois Mary Beth Hogan, M. Assistant Professor Department of Pediatrics West Virginia University School of Medicine Morgantown, West Virginia Carla Irani, M. Section of Allergy and Immunology Division of Pulmonary, Allergy Critical Care Medicine University of Pennsylvania School of Medicine Philadelphia, Pennsylvania Kevin J. Professor and Chief Department of Allergy/Immunology Medical College of Wisconsin Chief Department of Medicine Division of Allergy/Immunology Children s Hospital of Wisconsin Milwaukee, Wisconsin Robert C. Chairman Division of Otolaryngology Cook County Hospital Associate Professor Department of Otolaryngology-Head & Neck Surgery Northwestern University Medical School Chicago, Illinois Theodore M. Professor Department of Pediatrics University of Colorado Health Sciences Center Head Department of Pediatric Allergy-Immunology National Jewish Medical and Research Center Denver, Colorado Phil Lieberman, M. Clinical Professor Department of Internal Medicine and Pediatrics University of Tennessee College of Medicine Cordova, Tennessee Kris G. Associate Professor Department of Medicine Northwestern University Medical School Chief Department of Allergy-Immunology Saint Joseph Hospital Chicago, Illinois Roger W. Professor and Department Chair Department of Microbiology & Immunology School of Medicine and Health Sciences University of North Dakota Grand Forks, North Dakota W. Professor and Section Head Department of Allergy, Asthma and Immunology East Carolina University School of Medicine Greenville, North Carolina Babak Mokhlesi, M. Assistant Professor Department of Medicine Division of Pulmonary and Critical Care Rush Medical College/Cook County Hospital Chicago, Illinois Michelle J. Department of Radiology Northwestern Memorial Hospital Northwestern University Medical School Chicago, Illinois Sai R. Assistant Professor Department of Pediatrics Northwestern University Medical School Department of Pediatrics/Allergy Children s Memorial Hospital Chicago, Illinois Peck Y. Fellow Department of Pediatrics Division of Allergy and Immunology National Jewish Medical and Research Center Denver, Colorado Roy Patterson, M. Bazley Professor of Medicine Department of Medicine Chief Division of Allergy-Immunology Northwestern University Medical School Chicago, Illinois Neill T. Clinical Instructor Department of Dermatology Mercy Hospital and Medical Center Chicago, Illinois Jacqueline A. Assistant Professor Department of Pediatrics and Medicine Northwestern University Medical School Acting Division Head Department of Allergy Children s Memorial Hospital Chicago, Illinois Jacob J. Emeritus Professor of Microbiology Department of Medicine Division of Allergy-Immunology Northwestern University Medical School Chicago, Illinois Robert E. Clinical Professor Departments of Medicine and Pediatrics State University of New York at Buffalo Department of Medicine (Allergy/Immunology) Buffalo General Hospital Buffalo, New York Anthony J. Associate Professor of Medicine Seton Hall University Graduate School of Medicine Chairman Department of Medicine St. Professor Departments of Radiology, Neurosurgery, and Otolaryngology Northwestern University Chief of Neuroradiology Department of Radiology Northwestern Memorial Hospital Chicago, Illinois Carol A. Clinical Instructor Department of Medicine Division of Allergy-Immunology Northwestern University Medical School Chicago, Illinois Andrew Scheman, M. Associate Professor of Clinical Dermatology and Department of Dermatology Northwestern University Medical Center Chicago, Illinois William R.
With 100% Alcohol 250mg azithromycin otc antibiotics to treat bronchitis, obliteration of the varices was obtained in 4 patients purchase genuine azithromycin on line virus protection for android, 3 patients had some improvement and 1 patient died during the follow up period order azithromycin us virus x reader dmmd. The incidence of oesophageal ulceration and other side effects after the procedure were the same in both series. It is evident that 100% Alcohol is as effective as 1% Thrombar in the sclerosis of the oesophageal varices. Ulcer healing was achieved in 24 out of patients (95%) in Denol group and 29 out 30 patients (96. Helicobacter eradication was achieved in 17 out of 25 patients (68%) in Denol group and 8 out of 30 patients (26. Denol is superior in eradication of Helicobacter pylori infection, however, one week treatment of antibiotics is not sufficient to obtain satisfactory eradication rate for Helicobacter pylori infection. The specific study regarding bowel habit included retrospective and prospective studies done on 300 children aged 1 to 5 years. In the retrospective study investigated by asking the questionnaires to the mothers, each child passed 2 soft stools per day with an average of one tea cup for each motion. In the prospective study, in which each motion of every child was observed for one week, the amount of stool passed per motion ranged from 54. On average, they passed stools once daily for 5 days, and twice daily for at least one day. The small intestinal transit time, done on 74 children by breath hydrogen test, was 90. The whole gut transit time done on 30 children by colorimetric method using Norit capsules were 1009. The amount of daily stool output in our children was very much larger than that of children from the United Kingdom. The whole gut transit time of our 153 Bibliography of Research Findings on Gastrointestinal Diseases in Myanmar children was similar to those in Bangladesh. The study involved 1206 children aged 2-12 years in 21 villages in Myanmar [Burma] starting in August 1984. The intervention and non- intervention villages were comparable regarding almost all the important baseline variables, including prevalences of Ascaris infection (80. A significant increment of th th height gain was found, starting after the 6 month, and of weight gain after the 24 month, of the study among the treated 2-10 years old children when compared with the non-treated ones. Lesser increments in height-for-age and weight-for-age were also observed after successive treatments among the treated children with initially higher mean worm burdens. The findings are discussed in the context of causal relationship between ascariasis and malnutrition in children. The controls, consists of 6 children from the same locality as patients, were apparently healthy and in the same age group. Serum chloride tends to increase in the patients and the increase was more pronounced in the group suffering from both malnutrition and diarrhea. Serum aldosterone levels were raised in all the three groups of patients namely malnutrition, diarrhea. Rural area of Shwepyithar Township, Yangon Division and rural area of Tharbaung Township, Ayeyarawaddy Division were chosen for diarrhoea case management trained area (case) and non trained area (control) respectively. From each trained and non trained areas 100 mothers of under five children, 6 basic health staff and 4 voluntary health workers were included in the study. Regarding the result of basic health staff there was no difference between training and non training areas, both area showing reasonably good results. Most of the intestinal types were well and moderately differentiated, and most of the diffuse types were poorly differentiated. Peritoneal aspiration cytology was performed in 41 patients who were provisionally diagnosed as acute appendicitis. Patients with positive results underwent emergency surgery, 34 had histologically proven acute appendicitis and two patients were of other cause (tubo-ovarian abscess and Meckel s diverticulitis). It is concluded, therefore, that peritoneal aspiration cytology is a useful diagnostic test in management of patients with suspected acute appendicitis. Hence, the detection of Urease activity in gastric biopsies is used for assessment of the presence of Helicobacter pylori in chronic gastritis. With an aim to establish a sensitive and locally available test kit, microtiter biopsy urease broth testkit is developed. All cases presented with features consistent with findings reported by other s from developing countries. Smears were prepared from stool samples collected from those cohort infants with diarrhoeal episodes during the study period. The stool samples were also processed for virological examination and bacteriological culture of Salmonella, Shigella and Vibrio spp. Medical history, clinical conditions and examinations for those cases were recorded by field medical officers assigned. They were examined under oil immersion objective (x 100) and confirmed as Cryptosporidium when bright deep pink round or oval structures with clear halo, measuring about 4-5um were found. These oocysts may appear either as a clean central with dark periphery or with dark centre and light periphery. Watery diarrhoea and frequency of motions varying between 2-10 times per day were observed. Out of 42 cases of carcinoma of the oesophagus 20 involved the middle third and 22 involved the lower third. Histologically, 30 cases were squamous cell carcinomas and 12 cases were adenocarcinomas. Lymph nodal metastases were present in 20 patients and the most commonly involved lymph nodes were the coeliac group of lymph nodes. The sensitivity, specificity and accuracy in detecting lymph node metastases were 45%, 100% and 74% respectively. The sensitivity, specificity and accuracy in detecting peritoneal metastases were 25%, 100% and 93% respectively. Ultrasound could not detect intra-abdominal extra-oesophageal spread and infiltration to surrounding structures accurately. Because of its low sensitivity in detecting intra-abdominal metastases and its failure in detecting even intra-abdominal extra- oesophageal spread, ultrasound can not be used as a staging tool in carcinoma of the oesophagus. Pre and post operative treatment planning and the oral surgical technique applied is presented. Therefore, I conclude that graded compression ultrasonography was useful to rule out the diagnosis of acute appendicitis and helped to avoid unnecessary appendisectomies and negative laprotomies. After an overnight fast, the subjects drank a 100ml test solution conatining 5g of lactulose (7. Thin layer chromtography was carried to determine the urinary sugar content at a later date. It was a cross sectional analytical study consists of 30 cluster household survey on case management of diarrhoea, the health facility survey on diarrhoea case management and review of programme documents. It was found that no significant association 159 Bibliography of Research Findings on Gastrointestinal Diseases in Myanmar between sociodemographic characteristics of caretakers and satisfactory home management of diarrhoea. Health Facility survey on diarrhoea was conducted in twenty health facilities to assess the quality of diarrhoea case management.
However order 500 mg azithromycin free shipping infection x box, contributing factors may include higher concentrations of airborne pollution azithromycin 500mg without prescription virus 72 hour, such as diesel exhaust particles ( 10); rising dust mite populations ( 11); less ventilation in homes and offices; dietary factors ( 12); and a trend toward more sedentary lifestyles ( 13) generic azithromycin 250 mg without prescription infection years after a root canal. With the increased prevalence of allergic rhinitis, the disorder has increased in importance, and the suffering and annoyance that many experience should not be underestimated. In allergy-specific questionnaires ( 14,15), subjects with allergic rhinitis consistently reported lower quality of life than nonallergic controls. In a large health outcomes study of patients with moderate to severe allergic rhinitis symptoms, 70% of untreated patients reported being embarrassed or frustrated by their allergy symptoms, and 98% reported being troubled by practical problems ( 15). Considerable expenditures are involved in medications, physician fees, and economic loss secondary to absenteeism and inefficient performance at work. Ross estimated that the cost of decreased productivity in the United States labor force due to allergic rhinitis totaled $2. Conservative estimates report that prescription medication costs are greater than $1 billion per year, and over-the-counter medications are at least twice that amount (17). The severity of symptoms, however, may vary from year to year depending on the quality of pollen released and patient exposure during the specific pollinating seasons. Occasionally, the disease undergoes a spontaneous remission without specific therapy. Etiology Pollen and mold spores are the allergens responsible for seasonal allergic rhinitis ( Table 9. The pollens important in causing allergic rhinitis are from plants that depend on the wind for cross-pollination. Many grasses, trees, and weeds produce lightweight pollen in sufficient quantities to sensitize individuals with genetic susceptibility. Major aeroallergens in allergic rhinitis The pollination season of the various plants depends on the individual plant and on the various geographic locations. For a particular plant in a given locale, however, the pollinating season is determined by the relative amount of night and day and is constant from year to year. Weather conditions, such as temperature and rainfall, influence the amount of pollen produced but not the actual onset or termination of a specific season. Ragweed pollen, a significant cause of allergic rhinitis, produces the most severe and longest seasonal rhinitis in the eastern and midwestern portions of the United States and Ontario, Canada. In those areas, ragweed pollen appears in significant amounts from the second or third week of August through September. Occasionally, sensitive patients may exhibit symptoms as early as the first few days of August, when smaller quantities of pollen first appear. Although ragweed is the dominant airborne allergen in North America during the late summer and early fall, there are also other important weed pollens, such as sheep sorrel in the spring and plantain during the summer months. Late spring and early summer allergic rhinitis in this locale is caused by grass pollens, which appear from May to late June or early July. Roses coincidentally are in full bloom during the grass-pollinating season, and this accounts for the misconception. About 25% of pollinosis patients have both grass and ragweed allergic rhinitis, and about 5% have all three allergies. In other geographic locations, these generalizations are not correct, because of the particular climate and because some less common plants may predominate. For example, grass pollinates from early spring through late fall in the southwestern regions and accounts for allergic rhinitis that is almost perennial. Airborne mold spores, the most important of which throughout the United States are Alternaria and Cladosporium species, also cause seasonal allergic rhinitis. Warm, damp weather favors the growth of molds and thereby influences the severity of the season. Generally, molds first appear in the air in the spring, become most significant during the warmer months, and usually disappear with the first frost. Thus, patients with marked hypersensitivity to molds may exhibit symptoms from early spring through the first frost, whereas those with a lesser degree of hypersensitivity may have symptoms from early summer through late fall only. Define onset and duration of symptoms and emphasize any relationship to seasons or life events, such as changing residence or occupation or acquiring a new pet. Identify exacerbating factors, such as seasonal or perennial allergens and nonspecific irritants (e. Identify other associated allergic diseases, such as asthma or atopic dermatitis, or a family history of allergic diathesis. Obtain a complete medication history, including both prescription and over-the-counter medications. Sneezing is the most characteristic symptom, and occasionally one may have paroxysms of 10 to 20 sneezes in rapid succession. Sneezing episodes may arise without warning, or they may be preceded by an uncomfortable itching or irritated feeling in the nose. Sneezing attacks result in tearing of the eyes because of activation of the nasal lacrimal reflex. The rhinorrhea is typically a thin discharge, which may be quite profuse and continuous. Because of the copious nature of the rhinorrhea, the skin covering the external nose and the upper lip may become irritated and tender. Purulent discharge is never seen in uncomplicated allergic rhinitis, and its presence usually indicates secondary infection. Early in the season, the nasal obstruction may be intermittent or more troublesome in the evening and at night, only to become almost continuous as the season progresses. If the nasal obstruction is severe, interference with aeration and drainage of the paranasal sinus or the eustachian tube may occur, resulting in complaints of headache or earache. The headache is of the so-called vacuum type, presumably caused by the development of negative pressure when air is absorbed from the obstructive sinus or middle ear. Patients also complain that their hearing is decreased and that sounds seem muffled. Patients also may notice a crackling sensation in the ears, especially when swallowing. Nasal congestion alone, particularly in children, occasionally may be the major or sole complaint. With continuous severe nasal congestion, the senses of smell and taste may be lost. Itching of the nose also may be a prominent feature, inducing frequent rubbing of the nose, particularly in children. Eye symptoms (pruritus erythema and lacrimation) often accompany the nasal symptoms. Patients with severe eye symptoms often complain of photophobia and sore, tired eyes. Because of irritating sensations in the throat and the posterior drainage of the nasal secretions, a hacking, nonproductive cough may be present. A constricted feeling in the chest, sometimes severe enough to cause the patient to complain of shortness of breath, may accompany the cough. This sensation of tightness in the chest is particularly bothersome to the patients with severe nighttime cough.
Additional information: