
Bennett College. D. Larson, MD: "Order online Silagra no RX - Proven Silagra online".
Carefully planning for endotracheal intubation and subsequent hemodynamic management of these patients is vital buy silagra with visa erectile dysfunction doctor los angeles, as advanced airway techniques and critical fluid management with concomitant vasopressor use may be required order silagra canada erectile dysfunction 27. Succinylcholine should be used with caution in patients with pre-existing motor deficits as upregulation of nicotinic receptors at the neuromuscular junction can lead to increased risk of hyperkalemia generic silagra 50mg line erectile dysfunction medication cialis. Maintenance of Anesthesia The maintenance of general anesthesia in neurosurgical patients requires regimens that vary depending on the hemodynamic and monitoring goals for that procedure. To this end, once Mayfield fixation of the head and positioning are safely completed, mannitol (0. Anesthesia is either maintained or supplemented with intravenous drug infusions such as propofol with or without a short-acting opioid such as remifentanil or sufentanil. In the absence of muscle relaxant, immobility can be achieved with remifentanil infusions approaching 0. In cases of acute spinal cord injury, many of the same principles apply in regards to maintenance of anesthesia, as spinal cord perfusion (especially in cervical spine surgery) and the ability to perform neuromonitoring are of great concern. Ventilation Management Ventilatory management of patients undergoing neurosurgery is also a key consideration. For patients undergoing an intracranial procedure, tidal volume should be maintained at 6 to 8 mL/kg to minimize potential inflammatory injury to the lungs, with peak pressures kept at less than 40 cmH O. This strategy is generally not considered optimal, as the primary goal of fluid management in neurosurgical cases should be to maintain cerebral perfusion, which is a more important consideration and will actually lessen the amount of cerebral edema produced. Hypotonic solutions, such as Ringer lactate, when administered in large amounts, can contribute to cerebral edema. Glucose-containing solutions are avoided, as hyperglycemia is detrimental to cerebral metabolism (see section Glucose and Cerebral Ischemia), and because glucose is quickly metabolized and not osmotically active, leaving free water that can worsen brain edema. Depending on patient comorbidities and length of the surgery, electrolyte derangements may be common and require close monitoring. Hypertonic saline (3%) supplementation (given slowly at a rate of 50 to 100 mL/hr, and with the serum sodium level checked hourly) may be required in moderate to severe hyponatremic states. Rapid rises in serum sodium (more than 3 to 499 mEq/L/hr) must be avoided as this poses a risk for central pontine myelinolysis. Mannitol, especially at large doses, can cause mild electrolyte derangements which are generally short-lived (e. Also, diuresis from mannitol can result in dehydration that can impair cerebral perfusion. Preoperatively, coagulation studies, if available, should be carefully noted and are required in patients receiving anticoagulants. Neurosurgical patients having nonurgent surgery should have a platelet count over 100,000/mm. For patients having craniotomy for3 indications that would that would be at low risk for intraoperative bleeding, a “type and screen” with a negative antibody screen may be adequate. Red blood cells that are “typed and crossed” should be available for procedures with high risk for bleeding such as neurovascular procedures (e. For coagulopathies that may develop with the release of brain tissue thromboplastin, fresh frozen plasma, platelets, and cryoprecipitate may be needed. Complex spine surgery (especially with planned osteotomies or due to tumor) is usually associated with more profound blood loss, volume shifts, and the need for transfusion therapy. In recent years, however, strict glycemic control has been associated with increased risk for hypoglycemia that can be detrimental to the brain. For hyperglycemia exceeding this range, short-acting insulin should be readily available and can be given intravenously as a bolus with or without an infusion. In these cases, monitoring of serum glucose must be frequent enough to capture episodes of hypoglycemia. Emergence Emergence from general anesthesia following neurosurgical procedures requires meticulous attention to hemodynamic and ventilatory parameters, while also ensuring a prompt neurologic examination. Postcraniotomy hypertension is a well-described, albeit poorly understood, phenomenon, but 2516 can certainly be detrimental as it may increase bleeding from the surgical site and worsen cerebral edema. In patients having undergone posterior fossa surgery, and those in whom a pre-existing ventilatory disturbance was present due to brainstem compromise, emergence may be much slower and the time to safe extubation much more prolonged. Likewise, postoperative nausea and vomiting should be prophylactically treated in these cases for the same reasons. Also, dexamethasone should also be avoided following pituitary surgery as it can suppress the hypothalamic–pituitary–adrenal axis and significantly increase the false positive rate for diagnosis of postoperative hypopituitarism. The most common metastatic tumors to the brain include melanoma or those that originate in the lung, breast, or kidney. Infratentorial tumors in the posterior fossa are more common in children and include medulloblastoma, pilocytic astrocytoma, ependymoma, and brainstem glioma. Surgery for intracranial tumors can be safely accomplished with a careful preoperative evaluation and a smooth induction, maintenance, and emergence regimen. Steroids and anticonvulsants should be continued, and in many cases supplemented, prior to and during craniotomy. Hemodynamic instability during any part of the anesthetic should be minimized due to the possibility of impaired autoregulation in peritumoral brain parenchyma. Adequate vascular access (usually two large-bore peripheral intravenous catheters, and arterial catheter, and possibly a central venous catheter) is mandatory for brain tumor resection. The hemodynamic response is similar to laryngoscopy, and optimal control of blood pressure must again be sought, often by using propofol, opioids, or short-acting β-adrenergic antagonists such as esmolol. Excessive flexion, extension, or rotation of the neck may impair cerebral venous drainage via compression of the internal jugular veins. In patients with large tumors or known significant intracranial hypertension, efforts should be made to decrease brain volume for optimal surgical exposure and to minimize retractor-related edema. These include propofol, remifentanil, sevoflurane, desflurane, and possibly nitrous oxide unless otherwise contraindicated. Fluid maintenance should be accomplished with dextrose-free iso-osmolar crystalloids or colloids, with the goal of euvolemia (see earlier). Aberrations in blood pressure, usually systemic hypertension, can lead to worsening cerebral edema or tumor resection bed bleeding postoperatively, and short-acting and easily titratable drugs, such as labetalol, nicardipine, or esmolol should be immediately available. Adequate analgesia must be ensured as well, as craniotomy is painful and inadequate analgesia can worsen systemic hypertension. At the same time, avoiding analgesic doses which may obtund the patient and preclude a careful neurologic assessment is vitally important. These patients may more frequently require postoperative intubation and mechanical ventilation, due to altered levels of consciousness and delayed emergence. In adults, tumors of the posterior fossa include acoustic neuromas, metastases, meningiomas, and hemangioblastomas. These tumors, because of their proximity to the brainstem and cranial nerves, can cause altered respiratory patterns, cardiac dysrhythmias, or cranial nerve dysfunction.
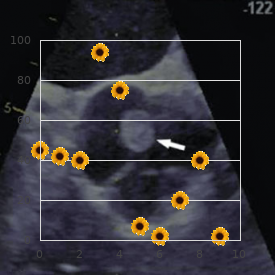
Both groins are prepped and draped in a sterile fashion discount silagra 100mg amex erectile dysfunction age 32, and the bilateral common femoral arteries are accessed with a 19- gauge needle purchase 50mg silagra fast delivery erectile dysfunction usmle. The needles are exchanged for arterial sheaths that are attached to a continuous heparinized saline fush discount silagra 100mg fast delivery impotence treatment reviews. A guide catheter is advanced through each sheath over a guide- wire into each internal carotid artery. Depending on the he- modynamic stability and hemorrhagic state of the patient, weight-based systemic heparin is dosed intravenously. The arrow points to the pseudoaneurysm of the into the high cervical segment of the internal carotid artery cavernous carotid artery. With the balloon infated 32 Managing Carotid Injury During Transphenoidal Surgery 331 until occlusion of the injured vessel, biplane angiography is of the vessel must occur both above and below the injury, performed over the cranium after injection of contrast into thereby “trapping” the perforation. Place- In formal balloon test occlusion cases, neurophysiologic ment adjacent to a branch vessel ensures that blood fow testing is performed on the patient at sequential time inter- is not static in the vicinity of the coil mass, decreasing the vals and with controlled drops in mean arterial pressure to chance for thrombus formation, propagation, and emboli. Indications and timing for cerebral blood fow based on imaging during angiography treatment are based on the severity of the symptoms, which is used to estimate the patient’s tolerance to subsequent ca- can include decreasing visual acuity, external ophthalmo- rotid occlusion. In patients for whom balloon test occlusion plegia, proptosis, hemorrhage, cortical venous drainage, in- fails, either through neurophysiologic testing or cerebral tolerable bruit/headache, and ischemia related to vascular blood fow imaging, surgical bypass remains a subsequent steal phenomenon. Venous drainage can extend anteriorly into the oph- ography performed through the vertebral artery can dem- thalmic veins, inferiorly into the pterygoid venous plexus, onstrate collateral supply to the anterior circulation via posteriorly into the petrosal sinuses, superiorly into the retrograde fow through a patent posterior communicating cortical veins via the sphenoparietal sinus, and across the artery. Often, a When vessel occlusion is required, endovascular emboli- mixed venous drainage pattern is seen. Also note the internal carotid artery angiogram after parent-vessel coil emboliza- artifact produced by the cottonoids packed into the sphenoid in the tion spanning from the ophthalmic segment to the petrous segment operating room. Note no anterograde fow of con- modalities of treatment, including carotid occlusion, which approaches, it is typical to inject contrast through an arterial runs the risk of recurrence by not obliterating the fstula. Endovascular therapy can be performed transarterially or A principal risk involved with the transvenous approach transvenously. Specifc manual maneuvers can be employed includes perforation of the relatively thin-walled venous to visualize the morphology of a high-fow fstula. The use of detachable platinum coils or transsphenoidal surgery does not lend itself to such a mor- liquid embolic material such as acrylic (N-butyl cyanoacry- phologic change. Often, the fow into a traumatic venous thrombosis may occur during catheterization. However, care must thalmic vein or intracranial hemorrhage from shunting into be taken not to decrease the pressure gradient between the cortical venous structures. Often, a formal balloon test occlusion does not most commonly via the ipsilateral jugular vein and infe- need to be performed, as anterograde fow through the ip- rior petrosal sinus. Both detachable coils and liquid embolic silateral internal carotid artery is already diverted fully into agents have been used successfully. Often, the sphe- nopalatine artery can be safely embolized after knowledge of the surrounding anastomoses so as not to jeopardize fow to collateral branches to the ophthalmic artery or menin- geal branches to the carotid artery supplying the trigeminal nerve. With the application of the transsphenoidal approach to the resection of tumors that spread outside the sellar com- partment, injuries to arteries within the intradural com- partment may occur. A commonly displaced or encased intradural artery by suprasellar extension of a tumor is the anterior cerebral artery. Iatrogenic perforation or laceration of this artery while dissecting adherent tumor from its wall is particularly devastating, as parent-vessel occlusion will often result in an ipsilateral stroke. Another possibility is avulsion of a small perforator from the anterior cerebral or anterior communicating artery (Fig. In select cases, when the laceration is small, an angled microcatheter can be advanced over a microwire distal to the site of perforation. Note the superior displacement of the left anterior form a plug outside the laceration while preserving distal cerebral artery secondary to underlying hematoma formation. Follow-up angiography and ophthalmologic examination can be performed on an elective basis from that point forward. I Management of Other Arterial Injuries Although injury to the cavernous segment of the carotid ar- tery accounts for the vast majority of vascular complications encountered with the transsphenoidal procedure, other ar- teries may be injured during the both the surgical approach and resection of a lesion. Injuries to the vasculature of the external carotid artery, most notably the sphenopalatine ar- tery, are less frequently recognized but important causes of epistaxis that can be easily treated. The complication usu- ally occurs during opening of the sphenoid ostium with a punch rongeur, as the artery is hidden in the inferior lateral corner of the sphenoidal sinus. Once avulsed, it can be dif- cult to coagulate because it has a tendency to retract toward the maxilla. Therefore, any patient who presents with advanced into the left anterior cerebral artery and retracted until it epistaxis after transsphenoidal surgery must obtain bilat- “pops” through the iatrogenic arteriotomy site into the subarachnoid eral external carotid artery angiograms with visualization space. In the event of an observed injury, immediate surgical stabilization and follow-up angiography are imperative to attaining a satisfactory outcome. With the evolution of endo- vascular imaging and technology, adequate tools are in place to treat the most commonly encountered arterial injuries, including carotid occlusions, stenoses, pseudoaneurysms, and fstulas. A normal postoperative angiogram mandates repeat follow-up study before discharge, as arterial injuries are often insidious and clinically occult until devastating presentation. Complications of transsphe- noidal surgery: results of a national survey, review of the literature, and personal experience. A microsurgi- otomy site demonstrating no further extravasation (arrow) of contrast cal study. J Neurosurg 1976;45:169–180 and preserved fow into the distal left anterior cerebral artery. J Neurosurg 1975;43:288–298 maintained, and the patient should receive intermittent an- 5. Surgical approaches to giographic studies and hyperdynamic volume and pressor the cavernous sinus: a microsurgical study. Surg Neurol 1998;50:174–177 Although the incidence of arterial injury during transsphe- 8. Certainly, tumors such such as the nasal septal mucosal fap16,17 have lowered these as craniopharyngiomas that extend into the third ventricle rates to levels similar to those of open approaches. Nonclinical sequelae include lar reconstructive techniques for separation of a direct com- prolonged hospitalization and increased cost of care. However, it can Although small dural defects can be reliably reconstructed be challenging to determine whether or not a patient is ac- using a variety of techniques and materials,18,19 large or tively leaking in the postoperative period. Alternative vascu- following surgery) as a consequence of patient activity, ex- larized reconstructions may be used when a septal fap is cessive debridement, or adjunctive therapy. The most common reasons for failure include of the recipient bed, elevation of the fap, placement of the high-fow defects, increased intracranial pressure, unsuit- able reconstructive material, improper placement of a fap, inadequate recipient bed, and disruption of the repair. These factors may be related to the disease (Cushing’s disease leading to obesity and poor healing) anatomical site (involvement of arachnoid cisterns or ventricles), reconstructive technique, adjuvant therapies, patient comorbidities (obesity, poor nutrition), or the pa- tient’s strenuous activities. Patients are overweight, heal poorly, and are at high risk for perioperative complications such as deep ve- Fig. We pre- rect communication between the ventricular system and sinus cavity fer vascularized repair such as a nasoseptal mucosal fap16,17 presents a unique challenge for reconstruction. There are other, secondary indicators of postop- ogy requires postoperative irradiation.
It runs N being supericial to the urogenital between gluteus medius and minimus over diaphragm and the dorsal N deep to it buy 50 mg silagra with amex erectile dysfunction medication canada. Emerges from N to Piriformis S1 cheap 100mg silagra mastercard impotence losartan,2 (remains in pelvis to the middle roots of the sciatic N and passes supply this muscle) out of the pelvis below piriformis through Posterior femoral cutaneous N S1 order 100 mg silagra mastercard erectile dysfunction in 20s,2,3 the greater sciatic foramen to enter gluteus (leaves pelvis via greater sciatic foramen) maximus. Perforating cutaneous N S2,3 (leaves pelvis via greater sciatic foramen) Posterior femoral cutaneous N (S1,2,3). Pudendal N S2,3,4 (leaves pelvis via greater Passes out of the pelvis below piriformis sciatic foramen) through the greater sciatic foramen. It Pelvic splanchnics (parasympathetic) S2,3,4 runs on the sciatic N, over the long head (remain in pelvis to supply pelvic organs) of biceps femoris to become subcutaneous Perineal branch of S4 (remains in pelvis to extending as far as the popliteal fossa. Arises From: Ant primary rami of L4,5,S1,2,3 from the anterior surface of the sciatic To: Tibial & common ibular (peroneal) Ns N in the pelvis and leaves the pelvis in this position through the greater sciatic It is formed in the upper sacral plexus and foramen, lying between the sciatic N and passes out of the greater sciatic foramen the ischium. In the buttock and thigh of obturator internus and the gemelli, it it lies initially deep to gluteus maximus supplies gemellus inferior before passing lying on gemellus superior, obturator into quadratus femoris from above. It passes out of the cover of gluteus from the anterior surface of the sciatic N maximus and for a short distance it is in the pelvis and leaves the pelvis through covered by only deep fascia, before it passes the greater sciatic foramen below piriformis deep to the two heads of biceps femoris. It passes runs vertically down in the midline of the medially over the ischial spine (lateral to posterior compartment of the thigh and the pudendal neurovascular bundle) and terminates by dividing into common ibular sends a branch to gemellus superior before (peroneal) and tibial Ns usually two-thirds turning forwards to pass through the lesser of the way down the thigh. In its course sciatic foramen, penetrating and supplying 6 over the gemelli, it is a close posterior obturator internus as it does so. It slopes gently medially in the lower To: Med & lat plantar Ns calf passing behind the medial malleolus of the lower tibia between the posterior tibial It arises in the lower third of the thigh artery anteromedially and the tendon of above the apex of the popliteal fossa as lexor hallucis longus posterolaterally. It the larger terminal branch of the sciatic runs under the lexor retinaculum where it N, and passes down in the midline into divides into terminal branches. Arises in the popliteal fossa, markedly lateral to the popliteal artery on passing out posteriorly over the ‘V’ behind entry to the popliteal fossa but then the the two heads of gastrocnemius and is artery crosses deep to the N to lie lateral joined by the sural communicating N from to it. The nerve leaves the fossa deep to the two It runs down laterally accompanied by the heads of gastrocnemius by passing deep to short saphenous vein to pass behind the the ibrous arch of soleus. It then runs deep lateral malleolus over the superior ibular to soleus on tibialis posterior in the midline, (peroneal) retinaculum to end in terminal crossing over the posterior tibial artery branches on the lateral side of the foot. It passes into the popliteal fossa along the upper lateral boundary just beneath It arises deep to ibularis (peroneus) the edge of biceps femoris and runs over longus and passes forwards deep to the plantaris, the lateral head of gastrocnemius muscle to wind around the ibula and to and the posterior capsule of the knee joint. It continues deep to extensor to wind around the neck of the ibula from digitorum longus to appear between it and posterior to lateral. It passes into ibularis tibialis anterior lying on the interosseous (peroneus) longus where it divides. It passes anterior to the tibia at the ankle joint between the anterior It arises deep to ibularis (peroneus) and tibial artery medially and the tendon of passes forwards and downwards to lie over extensor digitorum longus laterally, running the lateral surface of the ibula between beneath the superior and inferior extensor ibularis (peroneus) longus and brevis. It breaks up into terminal It pierces the deep fascia half way down branches on the dorsum of the foot. Its deep It arises beneath the lexor retinaculum terminal branches run medially beneath and runs forwards with the lateral plantar the long lexor tendons and across the artery around the sustentaculum tali of metatarsal shafts to end in muscular the calcaneus deep to abductor hallucis. It pierces the plantar From: Tibial N fascia in so doing and runs forwards over To: Terminal brs the tendon of lexor digitorum longus to appear more supericially again between It arises beneath the lexor retinaculum and abductor hallucis and lexor digitorum runs with the medial plantar artery around brevis in the sole of the foot. Hamstring portion: lower outer median N, its action is used as a test for quadrant of post surface of ischial this N in hand tuberosity Inserts Adductor portion: lower gluteal line & linea aspera. Short of triceps Inserts Post capsule of elbow jnt head: middle third of linea aspera, lat Action Lifts capsule away from jnt supracondylar ridge of femur Nerve Radial (C6,7,8) Inserts Styloid process of head of ibula, 8 lat collateral lig & lat tibial condyle Action Flexes & lat rotates knee. Post belly: Action Fixes perineal body & supports base of med aspect of mastoid process pelvic viscera Inserts Fibrous loop to lesser cornu of Nerve Perineal br of pudendal N (S2,3,4) hyoid bone Action Elevates hyoid bone. Ulnar head: sublime Nerve Lat plantar N (S2,3) tubercle (med border of coronoid process) & ibrous arch. Tendons of lexor Nerve Median N (C7,8,T1) (from med & digitorum longus pass through them lat cords) Action Flexes lat four toes. Lat tendon to Action Flexes distal phalanges of lat lat side of same, both via sesamoids four toes & foot at ankle. Med head: post surface of quarters into iliotibial tract (ant surface femur above med condyle of lat condyle of tibia) Inserts Tendo calcaneus to middle of three Action Extends & lat rotates hip. Maintains facets on post aspect of calcaneus knee extended via iliotibial tract Action Plantar lexes foot. Ulnar 2: cleft between rim of auditory tube tendons (bipennate) Inserts Palatine aponeurosis Inserts Extensor expansion (dorsum of Action Elevates, retracts & lat deviates prox phalanx) of ingers 2–5 radial side soft palate. Med 2: sympathetic) via pharyngeal br of vagus deep br of ulnar N (C8,T1) N (X) with its motor ibres from cranial Notes 60% have nerve supply as above. Arises Ant two-thirds of zygomatic arch & Post quarter: sup border of body of zygomatic process of maxilla hyoid bone Inserts Lat surface of angle & lower ramus Action Elevates hyoid bone, supports & of mandible raises loor of mouth. Med side of lat Arises Frontal process of maxilla pterygoid plate & fossa between med & Inserts Nasal aponeurosis lat plates. Action Clavicular head: lexes & adducts Passavant’s muscle closes nasopharyngeal arm. Arises Ant tubercles of transverse Extends hip processes of C3–6 Nerve Tibial portion of sciatic N (L5,S1,2) Inserts Scalene tubercle on sup aspect of irst rib Action Accessory to inspiration. Supericial part that make up inner layer of thoracic (downwards): lat epicondyle & lat lig of wall muscles. Others are innermost elbow & annular lig intercostals (lat) & transversus thoracis Inserts Neck & shaft of radius, between (ant) ant & post oblique lines Action Supinates forearm. Conjoint tendon Arises Post surface & muscular process of supports post wall of inguinal canal arytenoid cartilage Nerve Ant primary rami (T7–12). Joints classiied by type Articular disc can be present Fibrous joints Atypical synovial Joint cavity with Arytenocorniculate (can be synovial) synovial luid. Articular disc can be present Cuboideonavicular (can be synovial) Gomphosis (teeth) Types of synovial joint Radio-ulnar (interosseous membrane) Skull sutures Plane Sliding only Tibioibular (inferior) Hinge (ginglymus) One plane of Tibioibular (interosseous membrane) movement Modiied hinge (bicondylar) One plane of Primary cartilaginous joints movement + rotation Costochondral Condyloid (ellipsoid) Two planes of Sternochondral (irst rib) movement (circumduction) Spheno-occipital Saddle condyloid (sella) Two planes of movement + controlled rotation 9 Secondary cartilaginous joints Pivot (trochoid) Rotation only. One plane Intervertebral of movement Manubriosternal Ball and socket (spheroidal) Multi-axial. Sacrococcygeal Three planes of movement Symphysis pubis Xiphisternal Joints with interarticular Atypical synovial joints ibrocartilaginous discs Acromioclavicular Acromioclavicular (usually incomplete) Sternochondral (ribs 2–7) Femorotibial (knee) (incomplete—menisci) Sternoclavicular Radiocarpal (wrist) Temporomandibular Sternoclavicular Temporomandibular Typical synovial Acetabulofemoral (hip) Atlanto-axial (dens & facets) Atlanto-occipital Instant Anatomy, Fifth Edition. Ribs 2–10 with Type Condyloid own vertebra & one above (double Articulation Atlas with occipital bone cavity jnts separated by intra-articular lig). Talocalcaneal of inferior radio-ulnar) part (two facets) is part of subtalar jnt, 9 other being talocalcanean. Int carotid Site Between sphenoid, apex of petrous venous plexus connecting cavernous temporal & basilar occipital bones in sinus & int jugular vein middle cranial fossa Contains Int carotid art enters behind & exits above. Collectively making the spinal sphenopalatine notch of palatine bone canal (sup border of perpendicular plate & Contains Spinal cord/cauda equina, dura, orbital & sphenoidal processes). Anterior aspect of second rib Under surface of arch of aorta C1 Spinal root of accessory nerve crosses Ligamentum arteriosum transverse process of atlas Left recurrent laryngeal nerve Open mouth and dens Bifurcation of trachea Division of pulmonary trunk C2 Superior cervical ganglion Azygos vein (arch) enters superior vena cava C3 Body of hyoid bone T5 Thoracic duct crosses midline C4 Upper border of thyroid cartilage T5–8 Sternum Bifurcation of common carotid arteries T6 Upper border of liver C6 Cricoid cartilage T7 Inferior angle of scapula Larynx becomes trachea Accessory hemiazygos vein crosses Pharynx becomes oesophagus midline to azygos vein Middle cervical ganglion T8 Caval opening in diaphragm Vertebral artery enters foramen • Inferior vena cava transversarium of C6 vertebra • Right phrenic nerve Carotid tubercle of Chassaignac Left phrenic nerve pierces muscular Inferior thyroid artery crosses to diaphragm lat to central tendon thyroid gland Hemiazygos vein crosses to right to join azygos vein C7 First clearly palpable spinous process T8/9 Sternoxiphisternal joint (vertebra prominens) Stellate/inferior cervical ganglion T9 Superior epigastic vessels traverse diaphragm T2 Superior border of scapula Xiphoid T2/3 Suprasternal notch T10 Oesophageal opening in diaphragm 12 Oesophagus T3 Medial end of spine of scapula • Brs of left gastric vessels End of oblique issure of lung • Anterior and posterior vagi posteriorly at spine of T3 Instant Anatomy, Fifth Edition. Notes: (1) The thyroid gland arises from between the irst and second arch as a diverticulum (thyroglossal duct) which grows downwards leaving the foramen caecum at its origin. The head is separated from the neck with the line which begins on chin elevation – protuberantia mentalis, after that it laterally continues across the lower mandible edge, continues by the lower semicircle of outer aural meatus, goes on to the upper nuchal line, linea nuchae superior, and ends on both sides on outer elevation of occipital bone with protuberantia occipitalis externa. In general, the head is divided into cerebral cranium – cranium cerebrale and facial cranium – cranium faciale. Cerebral Cranium Limits: The cerebral cranium is separated from facial cranium with the anatomical formations described below.
The surgeon is able to verify complete A giant prolactinoma is classifed as having a diameter tumor removal in the suprasellar space and ensure that greater than 4 cm on imaging studies purchase silagra 100 mg fast delivery impotence and diabetes, a prolactin level over all accessible tumor has been removed silagra 50mg otc erectile dysfunction market. The prolactin levels may not correlate with size in sidual in up to 66% of macroadenomas cases order 50mg silagra with amex erectile dysfunction opiates, necessitating cases of giant prolactinomas, and the physician should be further tumor removal,34 published series about the use of alert to the possibility of a hook efect. Surgery can also be ofered in young patients with microprolactinomas and preoperative prolactin levels below 200 ng/mL. Medi- I Management of Prolactinomas in cal therapy generally consists of treatment with dopamine Pregnancy agonists, principally bromocriptine but also cabergoline. In Before pregnancy, patients are preferably treated with bro- some cases, the patient can be weaned from medical ther- mocriptine because of the larger clinical experience with apy if prolonged normoprolactinemia is maintained. The transsphenoidal techniques are performed from a surgical resection before the pregnancy. Women with through a microscope, endoscope, or both, depending on the a medically treated microprolactinoma can be treated with surgeon’s preference. These techniques can be supplemented contraceptive pills to prevent pregnancy as long as the dose by the use of stereotaxy as well as intraoperative imaging. A systematic recommendation cannot be made for treat- The goal of surgery is dependent on the size, suprasellar ment with estrogens in cases of macroprolactinomas. Surgery can be curative in more than 90% of the patient stopping the use of dopamine agonists when the cases of microprolactinomas but less than 50% of cases of pregnancy is confrmed. Rarely, prolactinomas can be more aggressive and pres- Cases of symptomatic tumor enlargement during preg- ent as invasive prolactinomas or degenerate into carcinomas. There is no evidence to suggest that References lactation increases the tumor size. Pituitary tumors: an endocrinological and neurosurgical Prolactinomas are the second most common form of pitu- challenge. Clin Neurosurg 1992;39:114–122 itary adenomas and are categorized as either microadeno- 4. Women are more commonly symptomatic and the introduction of macroprolactin screening: application of a new strict laboratory defnition of macroprolactinemia. Clin Chem present earlier in the course of the disease with amenor- 2003;49:1504–1509 rhea, galactorrhea, infertility, visual and cranial nerve dys- 6. Men more commonly present Med 1999;44(12, Suppl):1095–1099 with macroadenomas, and the early signs of hypogonadism 7. Endocrinol Metab Clin North treatment, and surgery is usually reserved for cases in which Am 1987;16:731–753 96 Endoscopic Pituitary Surgery 9. Con- standard dopamine agonists respond to chronic cabergoline treat- servative management of pituitary apoplexy: a prospective study. J Clin Endocrinol Metab 1997;82:876–883 J Clin Endocrinol Metab 1995;80:2190–2197 10. J Neurosurg up of prolactinomas: normoprolactinemia after bromocriptine with- 2000;93(Suppl 3):10–13 drawal. Clin Endocrinol (Oxf) 1990;33:619–624 Gamma knife radiosurgery for medically and surgically refractory pro- 13. Predictive value of se- noidal surgery: results of a national survey, review of the literature, rum prolactin levels measured immediately after transsphenoidal and personal experience. Intraoperative Semin Neurosurg 2001;12:289–294 magnetic resonance imaging to determine the extent of resection 17. Pituitary apoplexy—an endocrine emer- of pituitary macroadenomas during transsphenoidal microsurgery. World J Surg 1982;6:686–688 Neurosurgery 2001;49:1133–1143, discussion 1143–1144 18. What are the markers of technique for radiosurgical treatment of cavernous sinus pituitary aggressiveness in prolactinomas? Pituitary tumor apoplexy: char- 2007;156:143–153 acteristics, treatment, and outcomes. J Neurosurg Sci 1999;43:25–36 with an aggressive prolactin-secreting pituitary neoplasm: morpho- 21. Ann Endocrinol (Paris) 2007;68:106–112 case report of Sheehan’s syndrome with acute onset, hyponatremia 41. Acta Biomed 2009;80:73–76 tration of bromocriptine in the prevention of neurological complica- 26. Post Although acromegaly has been recognized as an entity for death is largely due to an increase in cardiovascular disease a very long time, it was frst clinically described by Pierre in the acromegalic population. Initially acromegaly was thought to be a disease, primarily bone hypertrophy, and pituitary gland enlargement was regarded as a further manifestation of gen- 2,3 4 I Presentation eralized bodily organ enlargement. Massalongo was the frst to suggest that the pituitary gland may be the cause of Acromegaly is found in the general population at a rate of the disease, and in 1900 Benda5 postulated that the eosinic 50 to 70 cases per million with an incidence of 3 to 4 cases granules that were observed in the glands of acromegalics per million per year. Paul attempted a temporal craniotomy to adenomas make up approximately 16% of surgical cases of remove a large pituitary tumor. Once the epiphyseal plates have closed, the sphenoidal operation for acromegaly, and one year later manifestations are that of acromegaly. Patients may frst notice although initially well accepted, fell out of favor in exchange changes in shoe size, ring size, and a coarsening of their fa- for the transcranial approaches, and due to the rather high cial features, with enlargement of their lips, macroglossia, morbidity and relatively poor results, surgical treatment of a prominent brow, prognathism, and increased spaces be- acromegaly was employed only for decompression for mass tween their teeth. Overgrowth contributes to a signifcant the available treatments at the time were far from optimal, the increase in weight and stress on the joints, cartilaginous time was right for the reintroduction of the transsphenoidal erosion, and severe osteoarthritis. Gerard Guiout12–14 merous cardiovascular complications, such as cardiomyopa- and his pupil Jules Hardy,15–17 incorporating the operative thy, arrhythmias, and coronary artery disease. The vast majority of patients presenting with acromeg- Growth hormone is under the control of the hypothalamic aly have an underlying pituitary tumor. Because must be considered to avoid potentially unnecessary pitu- of this there still exists test-to-test variation until adequate itary surgery. Analysis revealed it has prompted further evaluations of what is considered that there were statistically signifcant increases in survival “normal” levels of these hormones. The association between acromegaly and malig- assay were considered within normal limits,46 and <2 µg/L nancy is unclear. Orme et al36 performed a large retrospec- after oral glucose was also considered normal. The pa- treatment for acromegaly, though craniotomy rarely is indi- cated as a primary surgical intervention. We believe that adequate exposure of the sella and surrounding structures can be aforded by the microscope I Histopathology and Prognosis or the endoscope, but there are situations where some may Microscopically, the appearance of adenoma is very varied. The Surgical resection of the adenoma provides the highest nuclei may be cytologically pleomorphic with mitotic fg- hope for cure and is generally safe with acceptable morbid- ures and a stippled chromatin appearance. Further analysis tumor mass needs to be removed or signifcantly enough re- revealed the rather unsurprising fact that tumors can fur- duced so that there is no chance of recurrence and so that ther be subclassifed beyond micro and macroadenoma, the optic nerves are free of compression or impending threat and that increasing size correlates with decreasing success of such. Similarly, many as 5% of patients with acromegaly present after the Freda et al68 found 80% and 90% cure rates of micro- and age of 65. Results levels are routinely the test of choice in the immediate post- of resection are extremely good. These patients may experience improvement the frst postoperative day are found to correlate with surgi- in their cardiac function, glucose tolerance, and hyperten- cal success in 99% of patients.
Buy silagra no prescription. 5 Spices That Cure Erectile Dysfunction - How To Enhance Your Sex Life.